doi: 10.56294/saludcyt2024.1100
ORIGINAL
The Efficacy of Multi-Layer Compression System and TIME-Concept for the Management of Leg Ulcers in Patients with Ambulatory Venous Hypertension – Truth and Myth
La Eficacia del Sistema de Compresión Multicapa y el Concepto TIME para el Manejo de Úlceras en las Piernas en Pacientes con Hipertensión Venosa Ambulatoria - Realidad y Mitos
Petro Bodnar1 ![]() *, Anatoliy Bedenyuk1
*, Anatoliy Bedenyuk1 ![]() *, Tetiana Bodnar1
*, Tetiana Bodnar1 ![]() *, Sergii Karpeniuk1
*, Sergii Karpeniuk1 ![]() *
*
1L.Ya. Kovalchuk Department of Surgery No.1, Urology, Minimally Invasive Surgery, I. Horbachevsky Ternopil National Medical University, Ternopil, Ukraine.
Cite as: Bodnar P, Bedenyuk A, Bodnar T, Karpeniuk S. The Efficacy of Multi-Layer Compression System and TIME-Concept for the Management of Leg Ulcers in Patients with Ambulatory Venous Hypertension – Truth and Myth. Salud, Ciencia y Tecnología. 2024; 4:.1100. https://doi.org/10.56294/saludcyt2024.1100
Submitted: 10-01-2024 Revised: 16-04-2024 Accepted: 13-08-2024 Published: 14-08-2024
Editor: Dr.
William Castillo-González ![]()
ABSTRACT
Introduction: venous leg ulcers are late manifestations of chronic venous insufficiency that can cause disability and serious complications. The elderly are more commonly affected. This study was designed to test the effectiveness, healing rates, quality of life and costs of multi-layer compression system and TIME-concept (tissue management, infection control, moisture balance and wound edge optimization) for the management of leg ulcers in patients with ambulatory venous hypertension.
Method: a prospective clinical study on 50 outpatients with venous leg ulcers, treated three times weekly for 12 weeks or until healed, with all patients consenting and independently mobile associated with a multi-layer compression system along with the TIME-concept treatment.
Results: the study revealed that, the cohort was predominantly female (66 %) with a mean age of 61,7 years. Universal presence of varicose veins and secondary lymphedema was noted. Specific conditions included postthrombotic syndrome (24 %), calf pump dysfunction (8 %), and venectomy history (32 %). All patients achieved complete epithelialization, with an average healing time of 8,5±8,3 weeks and a median of 5,5 weeks (P=0,0064), with 88 % healing within 12 weeks. No significant complications were reported. The median number of clinic visits was 16,5, and the median treatment cost was UAH 11 240. Patients’ satisfaction with the treatment was 100 % according to completed wound healing.
Conclusions: the study demonstrates effective management of venous leg ulcers using a multi-layer compression system and the TIME concept, achieving high healing rates with minimal complications and manageable treatment costs.
Keywords: Leg Ulcers; Multi-Layer Compression System; TIME Concept; Ambulatory Venous Hypertension; Efficacy; Management.
RESUMEN
Introducción: las úlceras venosas de la pierna son manifestaciones tardías de la insuficiencia venosa crónica que pueden causar discapacidad y complicaciones graves. Las personas mayores se ven afectadas con mayor frecuencia. Este estudio se diseñó para probar la eficacia, las tasas de curación, la calidad de vida y los costes del sistema de compresión multicapa y del concepto TIME para el tratamiento de las úlceras de pierna en pacientes con hipertensión venosa ambulatoria.
Método: estudio clínico prospectivo en 50 pacientes ambulatorios con úlceras venosas en las piernas, tratados tres veces por semana durante 12 semanas o hasta su curación, con el consentimiento de todos los pacientes y movilidad independiente.
Resultados: el estudio muestra que, la cohorte fue predominantemente femenina (66 %) con una edad media de 61,7 años. Se observó la presencia universal de varices y linfedema secundario. Las afecciones específicas incluían síndrome postrombótico (24 %), disfunción de la bomba de la pantorrilla (8 %) y antecedentes de venectomía (32 %). Todos los pacientes lograron una epitelización completa, con un tiempo medio de cicatrización de 8,5±8,3 semanas y una mediana de 5,5 semanas (P=0,0064), con un 88 % de cicatrización en 12 semanas. No se notificaron complicaciones significativas. La mediana del número de visitas clínicas fue de 16,5, y el coste medio del tratamiento fue de 11 240 UAH. La satisfacción de los pacientes con el tratamiento fue del 100 % según la cicatrización completa de la herida.
Conclusiones: el estudio demuestra un tratamiento eficaz de las úlceras venosas de la pierna mediante un sistema de compresión multicapa y el concepto TIME, logrando altas tasas de cicatrización con mínimas complicaciones y costes de tratamiento manejables.
Palabras clave: Úlceras de Pierna; Sistema de Compresión Multicapa; Concepto TIME; Hipertensión Venosa Ambulatoria; Eficacia; Gestión.
INTRODUCTION
Venous leg ulcers are a pervasive challenge to the modern healthcare system, representing about 1 % to 3 % of people in Western countries and having a higher prevalence among the aged.(1,2) This often results in ulcers because of chronic venous insufficiency, which can lead to disability and serious complications. The global demographics are skewed towards the aging population, leading to an increase in venous leg ulcers’ incidence globally.(3,4) The origin of venous leg ulcers is mostly associated with ambulatory venous hypertension caused by such issues as ischemia, autoimmune diseases and lifestyle factors further aggravated by venous reflux or obstruction.(5) A successful management is based on dealing with these underlying causes and optimizing wound bed preparation, TIME concept focusing on tissue management, infection control, moisture balance and wound edge optimization. One must manage the tissue, keep infection in check, balance moisture, and optimize wound edges if they are to treat wounds effectively.(6) Still, a significant number of venous leg ulcers remain constant and problematic to close despite the improvement of treatments, with substantial consequences on patients’ quality of life and healthcare costs.(7,8) However, complete healing rates can be enhanced by integrating multi-layer compression systems together with TIME concept thus reducing the probability of recurrence.(9) According to studies that were done, long-term positive effects could be achieved if there was a sustained compression; this would prevent ulcer comeback hence improving patients’ well-being.(10) Additionally, various systematic reviews pointed out that applying a compressing dressing in treating venous leg ulcers boosts the wound healing rate and minimizes related complications.(11) Compression therapy combined with Wound bed preparation according to TIME principle is what ensures success in healing venous leg ulcers. Given the mechanisms behind venous ulcers, it’s crucial to identify and address the causes of ambulatory venous hypertension and associated factors such as lower limb ischemia, autoimmune diseases, and patient lifestyle.(12,13) Approximately 93 % of venous leg ulcers heal within 12 months with treatment; 7 % remain unhealed over 5 years. Median healing is 3-6 months. Recurrence is high, requiring ongoing compression therapy for prevention.(14,15) Treating chronic venous ulcers involves compressive therapy, with multilayer bandages proving more effective. Our study shows rapid healing and improved bacteriological profiles with four-layer bandages, emphasizing 30–40mmHg compression.(16,17) The TIME concept complements multi-layer compression by addressing tissue management, infection control, moisture balance, and wound edge optimization in wound bed preparation.(18) In the real world, care quality varies widely from ideal trial conditions.(19) Fife et al. found a 44,1 % healing rate for venous leg ulcers within 12 weeks in the US Wound Registry, contrasting with a reported 92 % average. They suggest achieving over 40 % may be unrealistic for complex patients.(20) The persistent, recurring nature of VLUs challenges effective management, impacting patient quality of life and healthcare costs, despite treatment advancements.
Research Aim
To evaluates effectiveness, healing, quality of life impact, and economic implications of compression for venous ulcers.
METHOD
Study Design
A prospective clinical study on 50 outpatients with venous leg ulcers.
All 50 independent patients with trophic ulcers consented to outpatient treatment, visiting the clinic thrice weekly. With standard deviation (σ) of 14,14, a significance level (α) of 0,05, a power (1 - β) of 80 %, and a minimum detectable effect size (Δ) of 5,60 sample size was calculated using formulae.
![]()
The study will continue for a period of 12 weeks or until complete healing is achieved, whichever is earlier. In case the recovery does not happen within the 12-week period, we will stay with the patient till he/she recovers.
Inclusion and Exclusion criteria
Inclusion criteria: postthrombotic syndrome, varicose disease, venectomy history, secondary lymphedema, or calf pump dysfunction; angiopathy Toe-Brachial Pressure Index (TBPI ≥ 0,5), BMI > 35, trophic ulcer ≥ 1 cm² with tendon contact.
Exclusion criteria: ischemia (WIfI scale grade 1-3), bone in wound, visual impairment, cancer, HIV, end-stage renal failure, ulcers < 1 cm², hindering tissue repair conditions.
Procedure
Treatment Protocol
The treatment protocol applied a multi-component elastic bandage from the foot to the knee, tailored to individual limb and wound characteristics. Bandage quality featured high-quality, cohesive materials by Wero Swiss, ensuring optimal compression aligned with ankle specifications per Laplace’s law.
Assessment and Monitoring
Edema regression was assessed with a centimeter tape. Wound care followed the TIME concept, incorporating debridement, exudation control, infection management, and wound edge formation. Dressings included Farmactive CMC/Alginate and Farmactive PU foam, with additional treatments like hydrogels and silicone dressings, and antiseptic solutions were used.
Photofixation and Wound Monitoring
Photofixation using WoundDoc software from Dalian Orientech Co. Ltd followed ISO 13485 standards, capturing wound dimensions in 2D mode per 2010 EWMA and FDA guidelines.
Outcome Measures
Healing was assessed via photofixation, defining complete healing as full epithelialization, with follow-ups at 72 hours and 14 days. Patient satisfaction used a 1-10 scale, and treatment costs considered clinic visits, dressing materials, and elastic bandage use.
Follow-Up
Patients were observed for 12 weeks or until complete healing, with clear recommendations for recurrence prevention provided to all patient’s post-treatment.
Statistical Analysis
Healing Efficiency: Evaluated using the Kaplan-Meier test with XLSTAT software, Lumivero.
At Significance Level 5 % (Log-rank test, P < 0,05). Ethical considerations typically revolve around several key areas: informed consent, privacy, minimizing bias, respect participants, ethical approval, and accurate reporting for investigating healing efficiency.
RESULTS
The study described demographics and clinical characteristics of 50 ambulatory venous hypertension patients: 66 % female, mean age 61,7 years, all with varicose veins and secondary lymphedema; 24 % postthrombotic syndrome; 32 % venectomy history (table 1).
|
Table 1. Clinical Characteristics and Demographics of Patients with Ambulatory Venous Hypertension in a Study on Multi-Layer Compression System and TIME Concept Efficacy for Leg Ulcer Management |
|
|
Variables |
Frequency |
|
N (% females) |
50 (66 %) |
|
Age (years) |
61,7±10,6 |
|
Presence of angiopathy, TBPI<0,7 (yes / no) |
2/48 |
|
Patients TBPI (≥60 mmHg) |
50 |
|
Varicose veins (yes/no) |
50/0 |
|
Venectomy in the past (yes/no) |
16/34 |
|
Postthrombotic syndrome (yes/no) |
12/38 |
|
Secondary lymphedema (yes/no) |
50/0 |
|
Calf pump dysfunction |
4/46 |
|
Contact with bone, joint, tendon (yes/no) |
1/49 |
|
Received antibacterial therapy (yes/no) |
0/50 |
Kaplan Meier survival curve for complete epithelialization showed that all 50 patients achieved complete epithelialization. Average healing time: 8,5±8,3 weeks, median 5,5 weeks (P=0,0064). 88 % healed within 12 weeks; outliers, up to 48 weeks. No major complications, except mild maceration (figure 1).
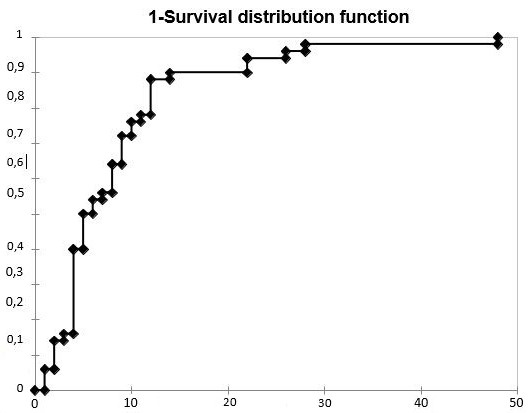
Figure 1. Survival curve, Kaplan-Meier method, time to complete ulcer healing
Patients categorized by prior venectomy and presence of postthrombotic syndrome showed significant differences in ulcer size (6,9 ± 7,7 cm² vs. 19,38 ± 35,8 cm², P=0,16, Mann-Whitney test). This comparison highlights the potential impact of prior venectomy on ulcer size in this patient population (figure 2).

Figure 2. Area of the leg ulcer in the patients with and without past venectomy
The Kaplan-Meier survival curve comparing time to heal ulcers in patients with and without past venectomy showed no significant difference in mean healing time (4,86±2,23 vs. 6,29±3,8 weeks, P=0,094). This comparison of time to complete ulcer healing with and without venectomy is shown in (figure 3).

Figure 3. Comparison of the mean time to complete healing in the group with and without venectomy
After excluding postthrombotic syndrome patients, no significant difference in healing time was found between those with and without venectomy (4,86 ± 2,23 vs. 6,0 ± 3,67 weeks, Log-rank test, P=0,163). When excluding post-thrombotic syndrome patients, prior venectomy does not seem to have significantly changed the time required for complete ulcer healing in this group (figure 4).

Figure 4. Comparison of the mean time to complete healing in the group with and without venectomy (postthrombotic syndrome excluded)
The results of the study show that there is a considerable difference in the time and costs needed for treating leg ulcers. The average patient visits to the clinic: 25,5±25 visits; median 16,5 visits. Average clinic stays: 19,4±18,7 hours; median 12,4 hours. Cost of treatment: UAH 16,280,0±13,999,4; median UAH 11,240 as shown in (table 2).
|
Table 2. Duration of treatment until complete healing of leg ulcer and associated costs |
||
|
Parameter |
Median |
D’Agostino-Pearson Test (P-value) |
|
Time to complete healing of the ulcer (weeks) |
8,5 ± 8,3 |
5,5, P < 0,0001 |
|
Number of visits to the clinic |
25,5 ± 25 |
16,5, P < 0,0001 |
|
Time of immediate stay in the clinic (hours) |
19,4 ± 18,7 |
12,4, P < 0,0001 |
|
Cost of complete healing (UAH, bandage included) |
16 280,0 ± 13,999,4 |
11 240,00, P < 0,0001 |
DISCUSSION
The current study examines the study on venous leg ulcers in 50 patients found all achieved complete healing. Average healing time was 8,5 ± 8,3 weeks (P=0,0064); 88 % healed within 12 weeks. Complex cases took up to 48 weeks. Another study highlighted 4-layer bandaging’s efficacy, achieving a significant 58,62 % wound area reduction compared to Unna’s boot and short-stretch bandages. Additionally, multilayer elastic compression demonstrated substantial benefits in a 73-year-old woman, achieving complete healing within three months despite prior treatment failures.(21) A meta-analysis of pneumatic compression therapy versus bandage compression found comparable effectiveness in wound healing rates and adverse events (OR: 1,02, p=0,96; OR: 1,62, p=0,20) but emphasized the need for further high-quality trials to assess its broader feasibility and cost-effectiveness.(22) These findings underscore the varied yet promising approaches in managing venous leg ulcers, each offering unique benefits and considerations for clinical application.
The Kaplan-Meier survival curve shows the probability of complete healing over time. The majority of patients healed within 12 weeks, though there were significant outliers who required up to 48 weeks. A review underscores the chronicity of VLUs in aging populations due to chronic venous disease, emphasizing their significant impact on quality of life and the need for a personalized, multidisciplinary approach. Another study supports the essential role of compression therapy in VLU management, advocating early venous interventions to mitigate disease progression and recurrence.(23) Additionally, a systematic review of randomized controlled trials found that educational interventions, despite showing potential benefits like reduced ulcer size and improved patient outcomes, did not reach statistical significance in wound healing effects. This underscores the importance of combining academic techniques with clinical operations to enable patients manage VLUs efficiently.(24)
The study examined the impact of veneectomy on venous leg ulcer healing, revealing smaller wound areas post-venectomy (6,9 ± 7,7 cm² vs. 19,38 ± 35,8 cm²), although statistically insignificant (P=0,16). Differences in healing times for ulcers <10 cm² were also non-significant (4,86 ± 2,23 weeks vs. 6,29 ± 3,8 weeks, P=0,094), even after excluding post-thrombotic syndrome patients (4,86 ± 2,23 weeks vs. 6,0 ± 3,67 weeks, P=0,163). Other studies underscore wound size, infections, and comorbidities as key healing predictors.(25) While highlighting compression therapy’s role in faster healing.(26) Advanced wound dressings containing growth factors or antimicrobials were more effective than traditional ones.(27) Age (>65 years) correlated with longer healing times due to age-related skin changes.(28) While veneectomy may influence wound size, factors like wound characteristics and patient comorbidities are pivotal in wound healing rates.(29)
Patients averaged 25,5 ± 25 clinic visits (median 16,5), spending 19,4 ± 18,7 hours per patient, and incurring UAH 16 280,0 ± 13 999,4 (median UAH 11 240,00) for healing costs, all significant (P<0,0001). Treating a venous leg ulcer in the UK costs £166,39 per person every 2 weeks, while an Australian wound clinic spends $445,13 weekly, with $123,00 from health systems and $322,13 out-of-pocket.(30) Furthermore, a study shows that Australian hospital costs for venous leg ulcers are about US$802,55 million. Outpatient compression treatments are cost-effective, but substantial overall costs underscore the need for better prevention and management strategies.(31) Outpatient compression therapies are cost-effective versus complex inpatient care, yet venous leg ulcer treatment costs remain high, necessitating effective prevention strategies.
Most patients achieved complete healing within 12 weeks using multi-layer compression and the TIME-concept. Factors like past veneectomy and post-thrombotic syndrome minimally affected outcomes. Despite costs and clinic visits, high patient satisfaction underscores treatment protocol effectiveness in ulcer healing. Compression therapy improves venous return, reduces edema, and aids healing, consistent with literature, yet limited by small, specific sample size.
CONCLUSION
This study proves that multi-layer compression is effective and supports the TIME-concept for managing VLUs with most patients healing fully within 12 weeks. Some factors like wound characteristics and comorbidities of patients have greatly influenced the results though there were different rates of ulcer healing. The high costs associated with treating VLU emphasize the need for better prevention as well as management approaches. Hence, it is imperative that future research concentrates on studying various populations, comparing different types of compression therapy and optimizing cost effective treatment protocols to improve VLU management strategies.
REFERENCES
1. Bodnar P. Structural features of the lower limb deep vein remodeling as a morphologic component in the pathogenesis of pulmonary thromboembolism in cancer patients. Rep. of Morph. [Internet]. 2019Dec.19 [cited 2024Jul.1];25(4):11-6. Available from: https://morphology-journal.com/index.php/journal/article/view/394
2. Sopilnyk L, Dotsenko V, Aleksandraviciute B. Preservation of labour potential in the Ukrainian healthcare sector: on the way to the third SDG fulfilment in pandemic conditions. LBSHerald [Internet]. 2021;1(3):17–24. Available from: http://dx.doi.org/10.46489/lbsh.2021-1-3-3
3. Robles-Tenorio A, Lev-Tov H, Ocampo-Candiani J. Venous Leg Ulcer. Phlebology, Vein Surgery and Ultrasonography: Diagnosis and Management of Venous Disease. 2022:341-53.
4. Gai L, Hruzevskyi O, Koltsova I, Dubina A, Tabulina A. The use of immunological drugs for the treatment of wound infections in military personnel during hostilities. FM [Internet]. 2024 Mar. 15 [cited 2024 Jun. 29];3(1):59-70. Available from: https://futurity-medicine.com/index.php/fm/article/view/121
5. Millan SB, Gan R, Townsend PE. Venous ulcers: diagnosis and treatment. Am Fam Physician. 2019 Sep 1;100(5):298-305.
6. Ortega MA, Fraile-Martínez O, García-Montero C, Álvarez-Mon MA, Chaowen C, Ruiz-Grande F, et al. Understanding chronic venous disease: A critical overview of its pathophysiology and medical management. J Clin Med [Internet]. 2021;10(15):3239. Available from: http://dx.doi.org/10.3390/jcm10153239
7. Bavaresco T, Lucena A de F. Low-laser light therapy in venous ulcer healing: a randomized clinical trial. Rev Bras Enferm [Internet]. 2022;75(3). Available from: http://dx.doi.org/10.1590/0034-7167-2021-0396
8. Odynets O. Philosophy of Health Within the Metamodern Worldview Paradigm. FPH [Internet]. 2024 Jun. 19 [cited 2024 Jun. 29];3(3):42-59. Available from: https://futurity-philosophy.com/index.php/FPH/article/view/89
9. Burnet M, Metcalf DG, Milo S, Gamerith C, Heinzle A, Sigl E, et al. A host-directed approach to the detection of infection in hard-to-heal wounds. Diagnostics (Basel) [Internet]. 2022;12(10):2408. Available from: http://dx.doi.org/10.3390/diagnostics12102408
10. Farah MH, Nayfeh T, Urtecho M, Hasan B, Amin M, Sen I, et al. A systematic review supporting the Society for Vascular Surgery, the American Venous Forum, and the American Vein and Lymphatic Society guidelines on the management of varicose veins. J Vasc Surg Venous Lymphat Disord [Internet]. 2022;10(5):1155–71. Available from: http://dx.doi.org/10.1016/j.jvsv.2021.08.011
11. Todd M. Assessment and management of older people with venous leg ulcers. Nurs Older People [Internet]. 2018;30(5):39–48. Available from: http://dx.doi.org/10.7748/nop.2018.e1004
12. Raffetto JD, Ligi D, Maniscalco R, Khalil RA, Mannello F. Why venous leg ulcers have difficulty healing: Overview on pathophysiology, clinical consequences, and treatment. J Clin Med [Internet]. 2020;10(1):29. Available from: http://dx.doi.org/10.3390/jcm10010029
13. Ren S-Y, Liu Y-S, Zhu G-J, Liu M, Shi S-H, Ren X-D, et al. Strategies and challenges in the treatment of chronic venous leg ulcers. World J Clin Cases [Internet]. 2020;8(21):5070–85. Available from: http://dx.doi.org/10.12998/wjcc.v8.i21.5070
14. Lazarus G, Valle MF, Malas M, Qazi U, Maruthur NM, Doggett D, et al. Chronic venous leg ulcer treatment: future research needs: Future research needs for venous ulcers. Wound Repair Regen [Internet]. 2014;22(1):34–42. Available from: http://dx.doi.org/10.1111/wrr.12102
15. Mahlapuu M, Sidorowicz A, Mikosinski J, Krzyżanowski M, Orleanski J, Twardowska‐Saucha K, et al. Evaluation of LL‐37 in healing of hard‐to‐heal venous leg ulcers: A multicentric prospective randomized placebo‐controlled clinical trial. Wound Repair and Regeneration. 2021;29(6):938-50.
16. Tiwary SK, Choubey KK, Nath G, Kumar P, Khanna AK. Effect of four-layer dressing on the microbiological profile of venous leg ulcer. J Wound Care [Internet]. 2023;32(Sup3):S22–30. Available from: http://dx.doi.org/10.12968/jowc.2023.32.sup3.s22
17. Mabeba M. The Effect of Military Expenditure on Economic Prosperity in Croatia. FSocS [Internet]. 2024 May 7 [cited 2024 Jun. 29];2(2):4-20. Available from: https://futurity-social.com/index.php/journal/article/view/34
18. Derwin R, Patton D, Strapp H, Moore Z. The effect of inflammation management on pH, temperature, and bacterial burden. Int Wound J [Internet]. 2023;20(4):1118–29. Available from: http://dx.doi.org/10.1111/iwj.13970
19. Raju S, Knight A, Lamanilao L, Pace N, Jones T. Peripheral venous hypertension in chronic venous disease. J Vasc Surg Venous Lymphat Disord [Internet]. 2019;7(5):706–14. Available from: http://dx.doi.org/10.1016/j.jvsv.2019.03.006
20. Fife CE, Horn SD. The Wound Healing Index for predicting venous leg ulcer outcome. Adv Wound Care (New Rochelle) [Internet]. 2020;9(2):68–77. Available from: http://dx.doi.org/10.1089/wound.2019.1038
21. Velozo BC, Colenci R, Abbade LPF. Multilayer elastic compression for the treatment of a 30-year venous ulcer. An Bras Dermatol [Internet]. 2020;95(2):263–4. Available from: http://dx.doi.org/10.1016/j.abd.2019.08.025
22. Xu Q, Li Z. Effects of pneumatic compression therapy on wound healing in patients with venous ulcers: A meta-analysis. Int Wound J [Internet]. 2023;21(3):e14438. Available from: http://dx.doi.org/10.1111/iwj.14438
23. Bernatchez SF, Eysaman-Walker J, Weir D. Venous leg ulcers: A review of published assessment and treatment algorithms. Adv Wound Care (New Rochelle) [Internet]. 2022;11(1):28–41. Available from: http://dx.doi.org/10.1089/wound.2020.1381
24. Bossert J, Vey JA, Piskorski L, Fleischhauer T, Awounvo S, Szecsenyi J, et al. Effect of educational interventions on wound healing in patients with venous leg ulceration: A systematic review and meta-analysis. Int Wound J [Internet]. 2023;20(5):1784–95. Available from: http://dx.doi.org/10.1111/iwj.14021
25. Jacinto MAG, Oliveira AC de S, Martínez CSG, Schlosser TCM, Dantas BA da S, Torres G de V. Healing of venous Leg Ulcers influenced by individual aspects: Cluster analysis in a Specialist Wound Management Clinic. J Prim Care Community Health [Internet]. 2024;15:21501319231223458. Available from: http://dx.doi.org/10.1177/21501319231223458
26. Aloweni F, Mei CS, Lixuan NL, Fook-Chong S, Yobas P, Yuh AS, et al. Healing outcomes and predictors among patients with venous leg ulcers treated with compression therapy. J Wound Care [Internet]. 2022;31(Sup3):S39–50. Available from: http://dx.doi.org/10.12968/jowc.2022.31.Sup3.S39
27. Yousefian F, Hesari R, Jensen T, Obagi S, Rgeai A, Damiani G, et al. Antimicrobial wound dressings: A concise review for clinicians. Antibiotics (Basel) [Internet]. 2023;12(9):1434. Available from: http://dx.doi.org/10.3390/antibiotics12091434
28. Lee SY, Lee MJ, Byun SB. Analysis of the factors of wound healing problems after transtibial amputation in diabetic patients. Int J Low Extrem Wounds [Internet]. 2023; Available from: http://dx.doi.org/10.1177/15347346231198940
29. Scotton MF, Miot HA, Abbade LPF. Factors that influence healing of chronic venous leg ulcers: a retrospective cohort. An Bras Dermatol [Internet]. 2014;89(3):414–22. Available from: http://dx.doi.org/10.1590/abd1806-4841.20142687
30. Urwin S, Dumville JC, Sutton M, Cullum N. Health service costs of treating venous leg ulcers in the UK: evidence from a cross-sectional survey based in the north west of England. BMJ Open [Internet]. 2022;12(1):e056790. Available from: http://dx.doi.org/10.1136/bmjopen-2021-056790
31. Barnsbee L, Cheng Q, Tulleners R, Lee X, Brain D, Pacella R. Measuring costs and quality of life for venous leg ulcers. Int Wound J [Internet]. 2019;16(1):112–21. Available from: http://dx.doi.org/10.1111/iwj.13000
FINANCING
The author received no financial support for the research, authorship, and/or publication of this article.
CONFLICT OF INTEREST
The author declares the absence of any conflict of interest regarding the research, authorship and/or publication of this article.
AUTHORSHIP CONTRIBUTION
Conceptualization: Sergii Karpeniuk, Anatoliy Bedenyuk.
Data curation: Petro Bodnar.
Formal analysis: Tetiana Bodnar.
Research: Anatoliy Bedenyuk, Petro Bodnar.
Methodology: Sergii Karpeniuk, Tetiana Bodnar.
Project management: Sergii Karpeniuk.
Resources: Anatoliy Bedenyuk.
Software: Petro Bodnar.
Supervision: Tetiana Bodnar.
Validation: Sergii Karpeniuk.
Display: Petro Bodnar.
Drafting - original draft: Sergii Karpeniuk.
Writing - proofreading and editing: Tetiana Bodnar.