doi: 10.56294/saludcyt2024.928
ORIGINAL
Treating Post-Stroke Aphasia: Psychological Wellness Approaches
Tratamiento de la afasia post-ictus: Enfoques de Bienestar Psicológico
Astha Jaiswal1 ![]() *, Abhishek Shukla MD2
*, Abhishek Shukla MD2 ![]() *, Anupsinh H Chhasatia3
*, Anupsinh H Chhasatia3 ![]() *, Sonia Sharma4
*, Sonia Sharma4 ![]() *, Prakriti Kapoor5
*, Prakriti Kapoor5 ![]() *,
Devraj Singh Chouhan6
*,
Devraj Singh Chouhan6 ![]() *
*
1Manipal University, Centre for Distance and Online Education. Jaipur, India.
2Aastha Centre for Geriatric Medicine Palliative Care Hospital & Hospice, Department of Medical Director. Lucknow, India.
3Dr Kiran C. Patel Medical College and research institute (veer narmad south gujarat university), Department of Psychiatry, Gujarat, India.
4Noida International University, School of Allied Health Sciences, Noida, India.
5Chitkara University, Centre of Research Impact and Outcome, Punjab, India.
6Parul University, Faculty of Nursing, Vadodara, India.
Cite as: Jaiswal A, Shukla MD A, Chhasatia AH, Sharma S, Kapoor P, Singh Chouhan D. Treating Post-Stroke Aphasia: Psychological Wellness Approaches. Salud, Ciencia y Tecnología. 2024; 4:.928. https://doi.org/10.56294/saludcyt2024.928
Submitted: 28-12-2023 Revised: 20-04-2024 Accepted: 21-08-2024 Published: 22-08-2024
Editor: Dr.
William Castillo-González ![]()
ABSTRACT
One of the most difficult conditions to treat while dealing with post-stroke aphasia and depression is related. To help stroke survivors manage their depression symptoms, stroke medical professionals are essential. In light of stroke specialists’ opinions about post-stroke aphasia, this study intends to investigate current methods of treating depression. In five semi-structured focus groups, thirty-nine stroke healthcare professionals from various phases of stroke therapy took part. A thorough transcript analysis of these focus group talks was conducted using the interpretive description approach. After the transcripts were analyzed, several themes emerged, including the difficulties associated with treating depression and aphasia at the same time in stroke rehabilitation, the undervaluing of mood disorders in clinical practice, the use of ad hoc methods for diagnosis and treatment, and the attempts of stroke doctors to fill in the gaps in psychological care. This study emphasizes how difficult it is for doctors to treat depression in patients who have had a stroke-related aphasia. For better patient care, evidence-based therapies are crucial, as is the inclusion of mental health services in stroke rehabilitation. Policies that promote mental health should be developed, leaders should take the lead in putting comprehensive treatment plans into practice, and healthcare professionals should get specialized training. These initiatives have a critical role in enhancing the results and standard of life for those coping with the co-occurring conditions of depression and aphasia after stroke.
Keywords: Depressive; Stroke Medical Specialist; Interpretive Description; Post-Stroke Aphasia.
RESUMEN
Una de las afecciones más difíciles de tratar cuando se trata de afasia y depresión tras un ictus está relacionada. Para ayudar a los supervivientes de ictus a controlar sus síntomas de depresión, los profesionales médicos especializados en ictus son esenciales. A la luz de las opiniones de los especialistas en ictus sobre la afasia posterior al ictus, este estudio pretende investigar los métodos actuales de tratamiento de la depresión. En cinco grupos focales semiestructurados, participaron treinta y nueve profesionales sanitarios especializados en accidentes cerebrovasculares de diversas fases de la terapia del accidente cerebrovascular. Se realizó un análisis exhaustivo de la transcripción de las conversaciones de estos grupos focales utilizando el enfoque de descripción interpretativa. Una vez analizadas las transcripciones, surgieron varios temas, entre ellos las dificultades asociadas al tratamiento de la depresión y la afasia al mismo tiempo en la rehabilitación del ictus, la infravaloración de los trastornos del estado de ánimo en la práctica clínica, el uso de métodos ad hoc para el diagnóstico y el tratamiento, y los intentos de los médicos especialistas en ictus de llenar las lagunas de la atención psicológica. Este estudio pone de relieve lo difícil que resulta para los médicos tratar la depresión en pacientes que han sufrido una afasia relacionada con un ictus. Para mejorar la atención al paciente, son cruciales las terapias basadas en la evidencia, así como la inclusión de servicios de salud mental en la rehabilitación del ictus. Deben desarrollarse políticas que promuevan la salud mental, los líderes deben tomar la iniciativa de poner en práctica planes de tratamiento integrales y los profesionales sanitarios deben recibir formación especializada. Estas iniciativas tienen un papel fundamental en la mejora de los resultados y el nivel de vida de quienes se enfrentan a las afecciones concurrentes de depresión y afasia tras un ictus.
Palabras clave: Depresión; Especialista Médico En Ictus; Descripción Interpretativa; Afasia Post-Ictus.
INTRODUCTION
Aphasia, a language impediment usually occurs after a stroke. Speaking reading, comprehension, and writing skills could all be affected.(1) The use of visual aids or other communication devices is only one example of how CBT can be utilized to teach coping mechanisms to those who have trouble communicating.(2) Additionally, mindfulness might benefit those with aphasia who might have trouble focusing their attention and paying attention to details.(3) Additionally, social support might offer an opportunity for aphasia sufferers to hone their communication abilities in a comforting setting.(4) As aphasia sufferers and their families manage the adjustments and difficulties that the disease brings, counseling treatments can offer them emotional support and direction (5). These methods can help aphasia sufferers and their families enhance their general psychological health and quality of life.(6) Aphasia, an acquired communication problem that impairs one’s capacity to communicate, comprehend, read, and write, affects about 30 % of stroke survivors.(7,8)
Psychological monitoring and proof that psychological treatment is beneficial in treating the social aspects of depression are lacking, regardless of how sadness is diagnosed in a medical environment, and the emotional, and communication requirements of people with aphasia.(9) Psychiatrists in the field of mental health report having little trust in their ability to identify sadness from medical observations and interviews of aphasic individuals.(10) To investigate contemporary approaches for treating depression following position-caress aphasia considering the viewpoint of stroke medical practitioners.
Contributions
· The study used to learn more about the treatment of depression in stroke survivors who have post-stroke aphasia.
· According to the study, managing depression following post-stroke aphasia presents considerable hurdles for stroke experts.
· The essential need to incorporate mental health care into stroke rehabilitation programs is highlighted by this study.
· To find out more about managing depression after a stroke, the research conducted interviews with 39 stroke healthcare professionals and examined their exchanges.
Group therapy has been demonstrated to help those who suffer from aphasia regain their language skills, the results from 26 suffering from aphasia were examined in phase 1.(11) There was little evidence for improving practice, and there are differences in how speech pathologists formulate and present aphasia prognoses.(12) They created a learning curriculum. In the 5-week follow-up, participants’ counseling self-worth and evaluated themselves competency were evaluated.(13) Speech and Language Therapy (SLT) efficacy may be improved by pharmaceutical and non-invasive brain stimulation (NIBS) methods.(14) Speech therapists strive to improve communication and lessen the emotional and social toll that aphasia patients’ communication handicap has on them, for people with aphasia.(15) Aphasia sufferers run the danger of feeling lonely and unhappy. Focus groups were held in facilities that provide stroke care.(16) It has been discovered that the therapeutic relationship was a crucial part of treatment delivery.(17) The use of touching by language and speech pathologists working with patients who have aphasia as a result of a stroke was the topic of the study.(18) An evaluation was done on a group therapy method including grownup aphasics and their life partners.(19) The research was guided by the critical disability theory approach.(20)
METHOD
Research plan
The study utilized an interpret description approach to gather opinions on self-management after a stroke among health professionals, adhering to Consolidated criteria for Reporting Qualitative research (COREQ) standards and ensuring reliability and trustworthiness.
Participants
A study involving 65 healthcare workers, including 40 stroke specialists, examined the proportion of aphasia cases and professional discipline. The participants had varying experiences, with some not attending due to health-related or educational commitments, rotations, or illness. Table 1 contains specifics about the sites and users that are taking part. Figure 1 and 2 shows the proportion of aphasia caseload and Professional discipline.
|
Table 1. Details about locations and participation |
||||||
|
Focus group |
Regional |
Gender discrimination (n) |
Years of medical experience |
Standard deviation SD |
(Range) |
|
|
Female |
Male |
|||||
|
1 |
Acute |
8 |
0 |
9 |
11,44 |
(26-34) |
|
2 |
Inpatient rehab |
2 |
4 |
17,62 |
8,87 |
(6-30) |
|
3 |
Inpatient rehab 1 |
8 |
2 |
9,81 |
|
(1-23) |
|
4 |
Inpatient rehab 2 |
9 |
1 |
15,96 |
15,33 |
(1,9-40) |
|
5 |
Community Service |
6 |
0 |
14,6 |
12,96 |
(3–30) |
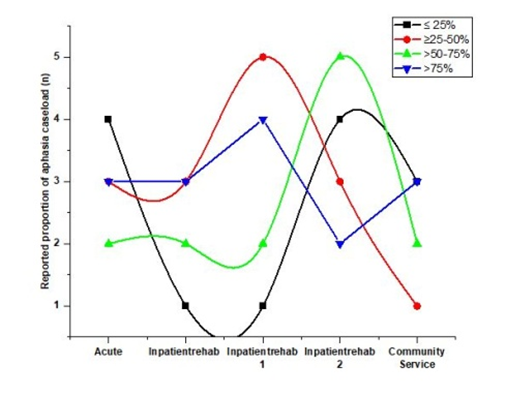
Figure 1. The proportion of aphasia caseload
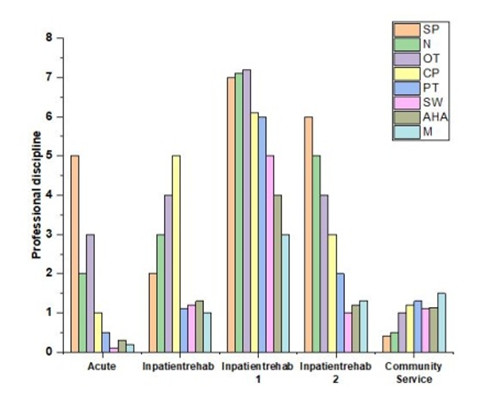
Figure 2. Professional discipline
Selection standards
Those who could take part in an English-language focus group and who were medical specialists who currently handled a caseload of stroke victims and had prior experience managing at least one patient with aphasia after a stroke were suitable for the study. If participants were student clinicians or volunteers, they were not eligible.
Statistical analysis
The version of SPSS 27.0 was utilized for analyzing the data. To depict qualitative information, frequency, and percentage were utilized.
Method of sampling
The study gathered experiences from individuals in various hospital and community settings using purposive sampling techniques. Metro or regional services, clinical psychologist support, and post-stroke treatment phases these sites were chosen. Stroke medical experts
were required to meet clinical experience, professional discipline, and aphasia case volume.
Transcripts of focus groups
Table 2 describes the steps involved in data analysis utilizing an interpretive description. NVivo 11’s qualitative analysis software was used throughout, along with handwritten notes and concept diagrams, to conduct the entire analysis. An “iterative” approach to analysis and note writing was employed at each level to ensure that “new” emergent themes matched recordings that could have been the subject of prior research.
|
Table 2. Data analysis techniques using interpretive description |
|
|
Process description |
Process summary |
|
Initially “open” coding |
Using open coding, concepts, and categories were found in all the data, exposing basic ideas such as identifying a mood problem as a central concept. |
|
Early exposure to data |
Listening to audio recordings for background on talks and interactions, and often reviewing records to take notes and comprehend information. |
|
Verifying and extending |
Thinking within to grasp the findings’ deeper meaning and applicability, and conversing with those present about the general idea outcomes. |
|
Critical self-reflection and introspection |
Finding newly undiscovered themes involves identifying outliers and abnormalities, evaluating available material, and considering the opinions of clinical specialists. |
|
Developing discoveries |
Organizing findings into a hierarchy and describing the whole thematically. |
|
Ongoing coding in axial |
By linking and combining codes inside open sections, axial coding facilitates connection analysis and verifies the applicability of concepts. |
|
Recognizing relationship |
Finding parallels, contrasts, and contradictions among notions, and extending them to create themes and sub-themes. |
|
Persistent active interpretation and analysis |
It outlines emerging topics, illustrative quotes, codes, and interpretations, emphasizing thorough analysis and addressing personal and interpretive biases. |
RESULTS
The study identified four main themes; ad hoc assessment techniques, challenging rehabilitation for aphasia and depressive moments post-stroke, undervaluing anxiety and sadness, and bridging emotional healthcare needs with available resources. Each theme had three to four sub-themes, reflecting diverse experiences and behaviors.
Aphasia and depression in stroke survivors can be difficult to treat
The following points are made in this order: (a) Aphasia therapy’s role in interdisciplinary depression care is unclear (b) seeking methods to collaborate (c) Recognizing the need for training and (d) Depression affects stroke rehabilitation participation. Each one of these subdivisions is discussed in greater depth below.
Aphasia therapy’s role in interdisciplinary depression care
Aphasia is a specialty work area due to the expertise necessary to evaluate and assist language and communication. Stroke care professionals often view aphasia, depression, and mood disorders as separate functional conditions requiring separate treatment. Some believe language is a complementary issue to stroke, while others lack knowledge and skills in aphasia and communication assistance techniques.
Methods to encourage one another because the work is so emotionally taxing
Stroke health professionals, from new graduates to veterans, often feel hopeless and unconfident when dealing with communication impairment and post-stroke aphasia followed by depression. To support these individuals and their families, healthcare professionals, particularly those in neighborhood and rehabilitation facilities, employ methods like co-therapy, debriefing, and collaborative clinical decision-making.
Recognizing the need for training
Healthcare providers for stroke victims emphasized the need for specific training to understand stroke, encourage interactions, detect stroke-related aphasia and depression, conduct state-of-mind tracking, and provide targeted strategies and therapies to enhance the prognosis of mental disorders.
Depression affects stroke rehabilitation participation
Stroke health professionals are working together to overcome barriers to therapeutic engagement for patients with aphasia and depression, particularly those with severe aphasia and depression. They are attempting to contact psychiatrists or other mental health experts, but patients often prefer to remain in their regions, avoid contact, and receive fewer visits.
Depression and mood problems are frequently ignored in stroke victims’ treatment
This major problem was broken down into some segments; (a)emphasis differs depending on the care situation (b)Consider other limitations and functions and (c)Obstacles to handling depression and disorders.
The emphasis differs depending on the care situation
Acute stroke health providers prioritize mood disorders and depression over acute cases, emphasizing patient care’s security and physical well-being. Speech therapists prioritize communication deficits and swallowing issues, while rehabilitation and community health professionals prioritize mood disorders and depression over acute cases, emphasizing emotional handling for therapy participation.
Consider other limitations and functions
Stroke medical professionals and focus groups view rehabilitation objectives as conflicting with depression prevention and management, with a focus on physical gains over emotional benefits. They also report a lack of knowledge about aphasia’s impact on individuals and families.
Obstacles to handling depression and disorders
The focus on hospital release for stroke patients, including those with aphasia, and the need to provide interdisciplinary care for depression and mood disorders in hospital and rehabilitation settings, along with staffing shortages and indirect clinical duties, pose significant challenges.
Ad hoc assessments and treatment regimens are common
The following sub-themes were identified through analysis of this central theme: (A) inconsistent techniques for identifying disorders of mood and identifying depression (B) attempt at differentiated diagnosis (C) inconsistent treatments depending on the circumstance and (D) inconsistent medical handoff and liaison.
Different approaches to the diagnosis of mood disorders and depression
The mood assessment process for stroke patients lacks structure and routine, with many stroke unfamiliar health professionals with assessments of mood in aphasia. Unofficial observation and incident reporting are more common, making it difficult to inquire about patients’ feelings.
Efforts to monitor mood and provide diagnostics during hospital-to-community
Stroke health professionals, including medical psychologists, social workers, nurses, and physiotherapists, recognize the difference between typical emotional responses and depression after a stroke. They collaborate to identify underlying causes and support emotional issues among stroke patients.
Varying interventions in different contexts
The effectiveness of interventions to alleviate mood disorders or treat depression varied between contexts and depended on the availability of individual or group therapy sessions as well as the availability of psychological services within healthcare networks. There appears to be a dearth of persons with aphasia and depression receiving regular, evidence-based psychological therapy.
Clinical transfer and coordination
Stroke health professionals discussed clinical handoff and communication issues, highlighting mood concerns in hospitals for stroke rehabilitation. Communication was challenging for post-stroke aphasia patients, and psychological conditions were not typically included in handover documents. Contemporary practice sub-themes include identifying effective practices, fostering relationships, and seeking external assistance.
Overview
Healthcare professionals tailor post-stroke aphasia therapy based on the patient’s interests and background, including pastoral support, gardening clubs, music, and art therapy, among other things. While acute staff takes care of examinations and information, stroke care teams concentrate on customized therapy.
CONCLUSIONS
According to the study, it can be difficult for medical personnel to treat concurrent aphasia and depression following a stroke. However, in stroke rehabilitation, issues with mood and depression are rarely prioritized, which results in ad hoc solutions. To prevent this at-risk group of stroke survivors should receive treatment for depression, policy creation, specialized instruction, and the use of frameworks based on science for assessing mood and treatment can be incorporated into post-stroke aphasia rehabilitation. Research is required to determine, whether psychological wellness and psychological care are effective following stroke aphasia. The use of such frameworks in more studies and clinical innovation will help to (1) clarify professional roles and responsibilities, (2) clarify communication and mood disorders management skills for stroke health professionals, and (3) provide guidance for multidisciplinary teamwork.
REFERENCES
1. Giachero, A., et al. “Conversational Therapy through Semi‐Immersive Virtual Reality Environments for Language Recovery and Psychological Well‐Being in Post Stroke Aphasia.” Behavioural Neurology 2020.1 (2020): 2846046.
2. Sekhon, Jasvinder K., et al. “Counselling training for speech–language therapists working with people affected by post‐stroke aphasia: a systematic review.” International journal of language & communication disorders 54.3 (2019): 321-346.
3. Flöel, Agnes. “Computerised speech and language therapy in post-stroke aphasia.” The Lancet Neurology 18.9 (2019): 806-807.
4. Sekhon, Jasvinder, K., et al. “Counselling education for speech-language pathology students in Australia: a survey of education in post-stroke aphasia.” Aphasiology 36.12 (2022): 1417-1446.
5. Wallace, Sarah J., et al. “A core outcome set for aphasia treatment research: The ROMA consensus statement.” International journal of stroke 14.2 (2019): 180-185.
6. Northcott, Sarah, et al. “Solution Focused brief therapy In post-stroke Aphasia (SOFIA Trial): protocol for a feasibility randomised controlled trial.” AMRC Open Research 1 (2019): 11.
7. Cheng, Bonnie BY, et al. “Prognostication in post‐stroke aphasia: How do speech pathologists formulate and deliver information about recovery?.” International Journal of Language & Communication Disorders 55.4 (2020): 520-536.
8. Baker, Caroline, et al. “A systematic review of rehabilitation interventions to prevent and treat depression in post-stroke aphasia.” Disability and rehabilitation 40.16 (2018): 1870-1892.
9. Baker, Caroline, et al. “Stroke health professionals’ management of depression after post-stroke aphasia: a qualitative study.” Disability and Rehabilitation 43.2 (2021): 217-228.
10. Stahl, Benjamin, et al. “Transcranial direct current stimulation to enhance training effectiveness in chronic post-stroke aphasia: a randomized controlled trial protocol.” Frontiers in Neurology 10 (2019): 1089.
11. Ribeiro Lima, Roxele, et al. “Socio-demographic factors associated with quality of life after a multicomponent aphasia group therapy in people with sub-acute and chronic post-stroke aphasia.” Aphasiology 35.5 (2021): 642-657.
12. Cheng, Bonnie BY, et al. “Prognostication in post-stroke aphasia: Speech pathologists’ clinical insights on formulating and delivering information about recovery.” Disability and Rehabilitation 44.18 (2022): 5046-5059.
13. Sekhon, Jasvinder K., et al. “A phase II randomised controlled trial evaluating the feasibility and preliminary efficacy of an education program on speech-language pathologist’self-efficacy, and self-rated competency for counselling to support psychological wellbeing in people with post-stroke aphasia.” Topics in stroke rehabilitation 30.8 (2023): 842-864.
14. Saxena, Sadhvi, and Argye E. Hillis. “An update on medications and noninvasive brain stimulation to augment language rehabilitation in post-stroke aphasia.” Expert review of neurotherapeutics 17.11 (2017): 1091-1107.
15. Ryan, Brooke, et al. “The aphasia action, success, and knowledge programme: results from an Australian phase I trial of a speech-pathology-led intervention for people with aphasia early post stroke.” Brain Impairment 18.3 (2017): 284-298.
16. Northcott, Sarah, et al. “Supporting people with aphasia to ‘settle into a new way to be’: speech and language therapists’ views on providing psychosocial support.” International Journal of Language & Communication Disorders 53.1 (2018): 16-29.
17. Lawton, Michelle, et al. “People with aphasia’s perception of the therapeutic alliance in aphasia rehabilitation post stroke: a thematic analysis.” Aphasiology 32.12 (2018): 1397-1417.
18. Merlino, Sara. “Professional touch in speech and language therapy for the treatment of post-stroke aphasia.” Touch in social interaction. Routledge, 2020. 197-223.
19. Rasmus, Anna, and Edyta Orłowska. “Marriage and post-stroke aphasia: the long-time effects of group therapy of fluent and non-fluent aphasic patients and their spouses.” Frontiers in Psychology 11 (2020): 1574.
20. Kristo, Isabella, and Jane Mowll. “Voicing the perspectives of stroke survivors with aphasia: a rapid evidence review of post‐stroke mental health, screening practices and lived experiences.” Health & social care in the community 30.4 (2022): 898-e908.
FINANCING
None.
CONFLICT OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Astha Jaiswal, Abhishek Shukla MD, Anupsinh H Chhasatia, Sonia Sharma, Prakriti Kapoor, Devraj Singh Chouhan.
Data curation: Astha Jaiswal, Abhishek Shukla MD, Anupsinh H Chhasatia, Sonia Sharma, Prakriti Kapoor, Devraj Singh Chouhan.
Formal analysis: Astha Jaiswal, Abhishek Shukla MD, Anupsinh H Chhasatia, Sonia Sharma, Prakriti Kapoor, Devraj Singh Chouhan.
Drafting - original draft: Astha Jaiswal, Abhishek Shukla MD, Anupsinh H Chhasatia, Sonia Sharma, Prakriti Kapoor, Devraj Singh Chouhan.
Writing - proofreading and editing: Astha Jaiswal, Abhishek Shukla MD, Anupsinh H Chhasatia, Sonia Sharma, Prakriti Kapoor, Devraj Singh Chouhan.