doi: 10.56294/saludcyt2024.899
ORIGINAL
Clinical and Antimicrobial Profile of Acinetobacter Species in Critical Care Setting- An Emerging Nosocomial Bug
Perfil clínico y antimicrobiano de las especies de Acinetobacter en el entorno de cuidados críticos: un microbio nosocomial emergente
Fathima Nilofar1 ![]() *, Mariraj.I2
*, Mariraj.I2 ![]() *, Saranya Palanisamy1
*, Saranya Palanisamy1 ![]() *, Nitesh Babu R1
*, Nitesh Babu R1 ![]() *
*
1Department of General Medicine, Saveetha Medical College Hospital, Thandalam, Chennai, Tamil nadu, India.
2Saveetha Medical College Hospital, Thandalam, Chennai, Tamil nadu, India.
Cite as: S Nilofar F, Mariraj.I, Palanisamy S, Nitesh Babu R. Clinical and Antimicrobial Profile of Acinetobacter Species in Critical Care Setting- An Emerging Nosocomial Bug. Salud, Ciencia y Tecnología. 2024; 4:.899. https://doi.org/10.56294/saludcyt2024.899
Submitted: 03-02-2024 Revised: 08-04-2024 Accepted: 27-08-2024 Published: 28-04-2024
Editor: Dr.
William Castillo-González ![]()
Corresponding author: Fathima Nilofar *
ABSTRACT
Background: the increasing prevalence of multidrug-resistant bacterial infections, particularly within healthcare-associated settings, poses a global public health threat. Among these pathogens, Acinetobacter species, notably Acinetobacter baumannii, have gained recognition as opportunistic nosocomial pathogens with a concerning propensity for antimicrobial resistance. Understanding their clinical and antimicrobial profile is crucial for addressing the challenges posed by these infections.
Objectives: to assess the prevalence of Acinetobacter species in distinct clinical samples. To analyze Acinetobacter species’ clinical profiles and patterns of antibiotic sensitivity using a range of clinical samples.
Method: a cross-sectional study was conducted in a tertiary care hospital in South India, approved by the Institutional Ethics Committee. Patients with confirmed Acinetobacter infections were included, and clinical samples were collected from the critical care unit. Demographics, comorbidities, clinical presentations, and outcomes were recorded. Laboratory processing included standard protocols for sample analysis, with confirmation through advanced methods such as PCR.
Results: out of 82 participants, 48,78 % showed positive cultures for Acinetobacter species. Prevalence varied by sample type, with urine samples exhibiting the highest positivity (50 %). Clinical analysis of 40 infected patients revealed a mean age of 43,72 ± 17,34 years. Musculoskeletal symptoms (17,5 %) and obstetric complications (17,5 %) were prominent clinical presentations. Antibiotic sensitivity analysis demonstrated that 51 % of isolates were multidrug-resistant, with high resistance to key antibiotics. Commonly resistant antibiotics included Cefepime, Piperacillin, Levofloxacin, Imipenem, Meropenem, and Amikacin.
Conclusion: this study adds to the growing understanding of Acinetobacter infections, emphasizing the need for awareness, infection control, and judicious antibiotic use. The multidisciplinary clinical presentations and high resistance rates underscore the complexity of managing Acinetobacter infections, requiring a holistic approach in healthcare settings. The findings inform strategies for infection prevention, surveillance, and therapeutic approaches in the global effort to combat antimicrobial resistance.
Keywords: Acinetobacter Species; Multidrug-Resistant Infections; Nosocomial Infections; Antimicrobial Resistance; Antibiotic Sensitivity Patterns.
RESUMEN
Antecedentes: la creciente prevalencia de infecciones bacterianas multirresistentes, sobre todo en entornos sanitarios, supone una amenaza para la salud pública mundial. Entre estos patógenos, las especies de Acinetobacter, sobre todo Acinetobacter baumannii, han ganado reconocimiento como patógenos nosocomiales oportunistas con una preocupante propensión a la resistencia a los antimicrobianos. Comprender su perfil clínico y antimicrobiano es crucial para abordar los desafíos que plantean estas infecciones.
Objetivos: evaluar la prevalencia de las especies de Acinetobacter en distintas muestras clínicas.
Analizar los perfiles clínicos de las especies de Acinetobacter y los patrones de sensibilidad a los antibióticos utilizando una serie de muestras clínicas.
Método: se realizó un estudio transversal en un hospital de atención terciaria del sur de la India, aprobado por el Comité de Ética Institucional. Se incluyeron pacientes con infecciones confirmadas por Acinetobacter y se recogieron muestras clínicas de la unidad de cuidados críticos. Se registraron datos demográficos, comorbilidades, presentaciones clínicas y resultados. El procesamiento de laboratorio incluyó protocolos estándar para el análisis de muestras, con confirmación mediante métodos avanzados como la PCR.
Resultados: de los 82 participantes, el 48,78 % presentaron cultivos positivos para especies de Acinetobacter. La prevalencia varió según el tipo de muestra, siendo las muestras de orina las que mostraron la mayor positividad (50 %). El análisis clínico de 40 pacientes infectados reveló una edad media de 43,72 ± 17,34 años. Las principales manifestaciones clínicas fueron síntomas musculoesqueléticos (17,5 %) y complicaciones obstétricas (17,5 %). El análisis de sensibilidad a los antibióticos demostró que el 51 % de los aislados eran multirresistentes, con una elevada resistencia a antibióticos clave. Entre los antibióticos más resistentes se encontraban la cefepima, la piperacilina, la levofloxacina, el imipenem, el meropenem y la amikacina.
Conclusiones: este estudio se suma a la creciente comprensión de las infecciones por Acinetobacter, enfatizando la necesidad de concientización, control de infecciones y uso juicioso de antibióticos. Las presentaciones clínicas multidisciplinares y las elevadas tasas de resistencia subrayan la complejidad del tratamiento de las infecciones por Acinetobacter, que requiere un enfoque holístico en los centros sanitarios. Los resultados de este estudio sirven de base a estrategias de prevención de infecciones, vigilancia y enfoques terapéuticos en el marco de la lucha mundial contra la resistencia a los antimicrobianos.
Palabras clave: Especies de Acinetobacter; Infecciones Multirresistentes; Infecciones Nosocomiales; Resistencia a los Antimicrobianos; Patrones de Sensibilidad a los Antibióticos.
INTRODUCTION
The increasing prevalence of multidrug-resistant bacterial infections poses a significant threat to global public health, particularly in the context of healthcare-associated infections (HAIs). Among the various pathogens implicated in nosocomial infections, Acinetobacter species have emerged as notable contributors, demonstrating a propensity for antimicrobial resistance and persistence in healthcare environments.(1)
Acinetobacter species, especially Acinetobacter baumannii, have gained recognition as opportunistic pathogens causing a spectrum of infections, including bloodstream infections, pneumonia, wound infections and urinary tract infections. The prevalence of Acinetobacter infections has shown an upward trend, particularly in critical care settings where patients are often immunocompromised, subjected to invasive procedures, and exposed to broad-spectrum antibiotics. Acinetobacter species are notorious for their ability to develop resistance to multiple classes of antibiotics, limiting treatment options and complicating therapeutic interventions.(2) Understanding the resistance mechanisms and patterns is crucial for implementing effective antibiotic stewardship programs and tailoring treatment strategies.
The nosocomial nature of Acinetobacter infections raises concerns about transmission dynamics within healthcare facilities. Investigation into the modes of transmission and potential sources is essential for implementing infection control measures. Limited data are available regarding the clinical outcomes associated with Acinetobacter infections in critical care settings.(3,4) Exploring the relationship between Acinetobacter infections and patient outcomes, including morbidity and mortality, will provide valuable insights for clinicians.
Investigating the antimicrobial and clinical features of Acinetobacter species has broader implications for public health.(5) This study aims to investigate the antimicrobial and clinical profile of Acinetobacter species in a critical care setting, shedding light on the evolving nature of this pathogen as a nosocomial threat. Insights gained from this study can inform strategies for infection prevention, surveillance, and the development of new therapeutic approaches. The findings of this study can guide healthcare practitioners in optimizing patient care, implementing effective infection control measures, and contributing to the global effort to combat antimicrobial resistance.
Aim
1. To assess the prevalence of Acinetobacter species in distinct clinical samples.
2. To analyze Acinetobacter species’ clinical profiles and patterns of antibiotic sensitivity using a range of clinical samples.
Method
Study Design
This cross-sectional study was conducted in a tertiary care hospital in South India after approval from the Institutional Ethics Committee before the commencement of the study. This study adhered to ethical guidelines, and all patient data were anonymized to ensure confidentiality.
Procedure
Patients with confirmed Acinetobacter infections based on laboratory results during the study period were included in the study. A systematic random sampling approach was employed to collect clinical samples from the critical care unit. Patient demographics, comorbidities, clinical presentation, and outcomes were collected. Body samples like blood, wound swabs, respiratory secretions, urine, and other relevant specimens were collected. All collected samples were processed in the microbiology laboratory following standard protocols. Identification of Acinetobacter species will be performed using biochemical tests, and confirmation will be done using advanced methods such as PCR.
Data Analysis
The prevalence of Acinetobacter species was calculated as the percentage of positive samples among the total samples collected. Subgroup analyses may be conducted based on sample type, patient demographics, and clinical departments.
Statistical Analysis
Descriptive statistics is used to summarize the clinical profile of patients infected with Acinetobacter species. Antibiotic sensitivity patterns were analyzed to determine the prevalence of multidrug-resistant strains. Subgroup analyses have been performed based on patient characteristics and infection types.
Results
In this study, a total of 82 patients from various clinical departments were included to determine the prevalence of Acinetobacter species in different clinical samples. The study participants’ baseline characteristics are displayed in table 1.
|
Table 1. Baseline Characteristics of the study participants |
|
|
Parameter |
Total no. of participants n=82 (%) |
|
Age in years (mean ± SD) |
47,53 ± 17,34 |
|
Gender Male Female |
32 (39) 50 (61) |
|
Type of Fluid for c/s Blood Urine Others |
4 (4,8) 30 (36,5) 48 (58,7) |
Overall Prevalence
Out of the 82 patients, 40 (48,78 %) were found to have positive cultures for Acinetobacter species as seen in figure 1.
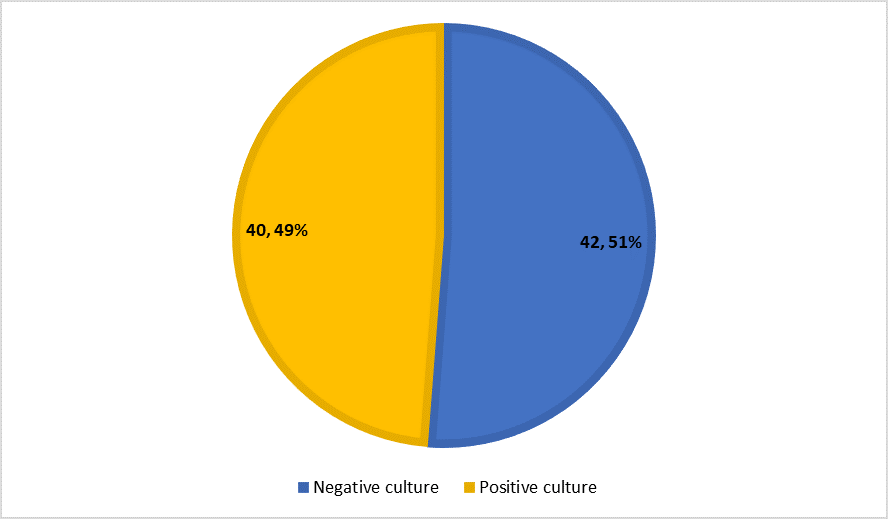
Figure 1. Prevalence of Acinetobacter species
Figure 2 shows the prevalence by sample Type where the urine sample was the highest with 50 %, followed by other samples (45 %) and blood (5 %).

Figure 2. Prevalence by sample type
For the 40 patients with confirmed Acinetobacter infections, the study examined their clinical profiles and antibiotic sensitivity patterns.
Clinical Profile: The mean age of infected patients was 43,72 ± 17,34.
Musculoskeletal symptoms (17,5 %), obstetrics (17,5 %), respiratory symptoms (10 %), and infections (10 %) were the most common clinical presentations as seen in figure 3.

Figure 3. Clinical presentation in culture-sensitive patients
Antibiotic Sensitivity Pattern: 51 % of Acinetobacter isolates were identified as multidrug-resistant, revealing at least three distinct antibiotic classes of resistance.
Commonly Resistant Antibiotics are Cefepime, Piperacillin, and Levofloxacin 100 % resistant each, and Imipenem, Meropenem, and Amikacin 92,80 % resistance each. (figure 4)

Figure 4. Resistant pattern of Acinetobacter isolates
Discussion
The present study aimed to investigate the prevalence of Acinetobacter species in various clinical samples, along with an evaluation of the antibiotic and clinical profile sensitivity patterns in infected patients. The findings provide valuable insights into the epidemiology and characteristics of Acinetobacter infections within the studied patient population.
Prevalence of Acinetobacter Species
The overall prevalence of Acinetobacter species among the 82 study participants was 48,78 %, indicating a substantial presence of this pathogen in the clinical setting. This prevalence aligns with the emerging concern of Acinetobacter as a nosocomial pathogen. The high prevalence underscores the importance of continued surveillance and infection control measures in healthcare settings. The prevalence varied by sample type, with urine samples exhibiting the highest positivity (50 %), followed by other samples (45 %) and blood samples (5 %). This distribution highlights the diversity in the sites of infection and suggests that Acinetobacter has the potential to colonize various anatomical locations within the human body. In a study conducted in a pediatric hospital, the prevalence of Acinetobacter species was found to be 30 % among children with respiratory infections.(6) A multicenter study across diverse geographical regions reported an overall prevalence of 25 % in patients admitted to intensive care units (ICUs) with Acinetobacter infections.(7) The comparative analysis reveals variations in Acinetobacter prevalence based on patient demographics, healthcare settings, and the type of infections studied. This information could help identify high-risk populations and tailor preventive strategies accordingly.
Clinical Profiles of Acinetobacter Infections:
In the subset of 40 patients with confirmed Acinetobacter infections, the clinical profile analysis revealed a mean age of 43,72 ± 17,34 years. This suggests that Acinetobacter infections are not limited to specific age groups, emphasizing the importance of considering this pathogen across various demographics. Musculoskeletal symptoms (17,5 %) and obstetric complications (17,5 %) emerged as notable clinical presentations. This diverse range of clinical manifestations underscores the opportunistic nature of Acinetobacter infections, affecting patients across different medical disciplines. Additionally, respiratory symptoms (10 %) and general infections (10 %) were observed, highlighting the versatility of Acinetobacter in causing varied clinical syndromes. Analyzing the clinical profiles of elderly patients, Tunay et al.(8) found that Acinetobacter infections were significantly associated with prolonged hospital stays and the presence of comorbidities. Conducted in a surgical department, another study identified a higher incidence of Acinetobacter infections in patients who underwent invasive procedures.(9) Comparing these studies might reveal different risk factors associated with Acinetobacter infections in specific patient groups. This information could guide targeted interventions for at-risk populations.
Antibiotic Sensitivity Patterns
The antibiotic sensitivity analysis revealed that 51 % of Acinetobacter isolates were multidrug-resistant, exhibiting antibiotic resistance to at least three different classes. This finding accentuates the challenging nature of Acinetobacter infections and emphasizes the urgency of implementing stringent antibiotic stewardship programs. The high resistance rates observed for Cefepime, Piperacillin, Levofloxacin, Imipenem, Meropenem, and Amikacin underscore the limited treatment options for Acinetobacter infections, warranting a careful selection of antimicrobial agents based on susceptibility testing. Focused on a community-based setting, Maziz et al reported lower rates of multidrug resistance in Acinetobacter isolates, with higher susceptibility to common antibiotics.(10) Contrasting these studies could highlight variations in antibiotic resistance patterns across different healthcare settings. Understanding regional differences in resistance profiles is crucial for effective empiric therapy.
Conclusion
This study aimed to comprehensively investigate the prevalence, clinical profiles, and antibiotic sensitivity patterns of Acinetobacter species in a diverse cohort of 82 patients across various clinical departments. The findings of this study shed light on several key aspects that contribute to our understanding of Acinetobacter infections in this specific healthcare setting. The results of this study contribute to the growing body of knowledge on Acinetobacter infections, emphasizing the need for heightened awareness, infection control measures, and judicious use of antibiotics in clinical practice. The multidisciplinary clinical presentations and high antibiotic resistance rates underscore the complexity of managing Acinetobacter infections, necessitating a holistic and collaborative approach in healthcare settings.
The insights gained from this study have several implications for public health and clinical practice. The high prevalence and multidrug resistance observed necessitate a multifaceted approach to infection prevention and control, including rigorous adherence to hygiene protocols, targeted surveillance, and the promotion of antimicrobial stewardship. Additionally, the diverse clinical presentations underscore the importance of maintaining a high index of suspicion for Acinetobacter infections across different medical specialties.
BIBLIOGRAPHIC REFERENCES
1. Joly-Guillou M-L, Brun-Buisson C. Epidemiology of acinetobacter spp.: Surveillance and management of outbreaks. Acinetobacter. 2020;71–100. doi: 10.1201/9781003069263-4
2. Awour SO. Monitoring the battlefield: Antimicrobial resistance, antibiofilm patterns and virulence factors ofacinetobacter baumanniiisolates from hospital system. 2022; doi: 10.1101/2022.12.14.520451
3. Boral B, Unaldi Ö, Ergin A, Durmaz R, Eser ÖK. A prospective multicenter study on the evaluation of antimicrobial resistance and molecular epidemiology of multidrug-resistant Acinetobacter baumannii infections in intensive care units with clinical and environmental features. Annals of Clinical Microbiology and Antimicrobials. 2019;18(1). doi: 10.1186/s12941-019-0319-8
4. Aljamaan F, Altawil E, Temsah M-H, Almeman A. Multi-drug resistant gram-negative infections among critically ill patients: Analysis of baseline characteristics and factors associated with mortality. 2020; doi: 10.21203/rs.3.rs-129355/v1
5. Bennett B, Iredell J. Global health governance and antimicrobial resistance. Ethics and Drug Resistance: Collective Responsibility for Global Public Health. 2020;389–99. doi: 10.1007/978-3-030-27874-8_24
6. A prevalence of infections with antibiotic-resistant acinetobacter baumannii in different clinical samples from hospitals in Erbil. ZANCO JOURNAL OF PURE AND APPLIED SCIENCES. 2020;32(3). doi: 10.21271/zjpas.32.3.11
7. Boral B, Unaldi Ö, Ergin A, Durmaz R, Eser ÖK. A prospective multicenter study on the evaluation of antimicrobial resistance and molecular epidemiology of multidrug-resistant Acinetobacter baumannii infections in intensive care units with clinical and environmental features. Annals of Clinical Microbiology and Antimicrobials. 2019;18(1). doi: 10.1186/s12941-019-0319-8
8. TÜNAY H, DEMİRDAL T, DEMİRTÜRK N. Risk factors for nosocomial pan drug resistant Acinetobacter baumannii infections. Acta Medica Alanya. 2019;3(3):254–60. doi: 10.30565/medalanya.543371
9. Arunkumar C, Chinnapan R. A clinical study of risk factors and the management of surgical site infections in general surgical cases at Tertiary Care Center: A two-year observational study. Albanian Journal of Trauma and Emergency Surgery. 2022;6(1):915–21. doi: 10.32391/ajtes.v6i1.248
10. Maziz MNH, Hussaini J, Khan MFK. Antibiotic susceptibility profiles of clinical isolates of Acinetobacter species isolated from Selayang Hospital, Malaysia. International Journal of Infectious Diseases. 2012;16. doi: 10.1016/j.ijid.2012.05.589
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The author declares that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Fathima Nilofar, Mariraj, Saranya Palanisamy, Nitesh Babu R.
Data curation: Fathima Nilofar, Mariraj.
Format Analysis: Fathima Nilofar, Mariraj.
Research: Fathima Nilofar, Mariraj.
Methodology: Fathima Nilofar, Mariraj.
Project Management: Fathima Nilofar, Mariraj.
Resources: Fathima Nilofar, Mariraj, Saranya Palanisamy, Nitesh Babu R.
Software: Fathima Nilofar, Mariraj.
Supervision: Fathima Nilofar, Mariraj, Saranya Palanisamy, Nitesh Babu R.
Validation: Fathima Nilofar, Mariraj, Saranya Palanisamy, Nitesh Babu R.
Display: Fathima Nilofar, Mariraj, Saranya Palanisamy, Nitesh Babu R.
Drafting: original draft: Fathima Nilofar, Mariraj, Saranya Palanisamy, Nitesh Babu R.
Writing, proof reading and editing: Fathima Nilofar, Mariraj, Saranya Palanisamy, Nitesh Babu R.