doi: 10.56294/saludcyt20241315
REVIEW
Improving Organizational Medical Care for Patients with Idiopathic Macular Hole: Impact on Quality of Life and Effectiveness of Modern Treatment Protocols
Mejora de la organización de la atención médica a pacientes con agujero macular idiopático: impacto en la calidad de vida y eficacia de los protocolos modernos de tratamiento
Dastan Kyrykbayev1,2 ![]() *, Marfuga Amanzhanovna Oteulieva1,2
*, Marfuga Amanzhanovna Oteulieva1,2 ![]() *, Ardak Mukhamedzhanovna Auezova1
*, Ardak Mukhamedzhanovna Auezova1 ![]() *, Gulnar Kairatovna Zhurgumbayeva2
*, Gulnar Kairatovna Zhurgumbayeva2 ![]() *
*
1Kazakhstan Medical University «Higher School of Public Health», Almaty, Kazakhstan.
2Kazakh Scientific Research Institute of Eye Diseases, Almaty, Kazakhstan.
Cite as: Kyrykbayev D, Amanzhanovna Oteulieva M, Mukhamedzhanovna Auezova A, Kairatovna Zhurgumbayeva G. Improving Organizational Medical Care for Patients with Idiopathic Macular Hole: Impact on Quality of Life and Effectiveness of Modern Treatment Protocols. Salud, Ciencia y Tecnología. 2024; 4:1315. https://doi.org/10.56294/saludcyt20241315
Submitted: 26-02-2024 Revised: 01-06-2024 Accepted: 11-07-2024 Published: 12-07-2024
Editor: Dr.
William Castillo-González ![]()
ABSTRACT
Introduction: IMH causes loss of central vision and it restricts the activities of a patient, therefore posing a threat to the patient’s quality of life. Modern developments in surgical interventions as well as the organization of medical care enhance the effectiveness of treatment while a detailed analysis of it is needed.
Objective: consequently, the purpose of this particular research is to examine organizational medical care among the specified population of patients with IMH, in regard to their quality of life and the efficacy of contemporary treatment regimens.
Method: to accomplish this, the current study applied narrative synthesis strategies and reviewed literature on IMH diagnosis, management for surgical solutions, and patient outcomes. This assessment encompassed previous and current therapy methods together with patient enlightenment and follow-up with impact on vision clarity and general quotient.
Results: from the current review, it was evident that surgeons are now using facilities such as small-gauge vitrectomy and pharmaceutical substances including ocriplasmin, which enhance macular hole closure rates and near visual acuity levels. Teaching has been done to patients/clients and organized follow-ups as part of the organizational care to improve quality of life as perceived by patients from follow-up questionnaires representing a significant improvement in visual function and activities.
Conclusion: this paper outlines that patients with IMH require a structured and coordinated, cross-professional approach to its management in conjunction with contemporary surgery revealing drastic enhancements to visual acuity levels and the overall wellbeing of a patient.
Keywords: Idiopathic Macular Hole; Organizational Medical Care; Visual Acuity; Quality of Life; Vitrectomy; Patient Education; Multidisciplinary Approach; Modern Surgical Techniques.
RESUMEN
Introducción: la HMI causa pérdida de visión central y limita las actividades del paciente, por lo que supone una amenaza para su calidad de vida. Los avances modernos en las intervenciones quirúrgicas, así como la organización de la atención médica, mejoran la eficacia del tratamiento, aunque es necesario un análisis detallado del mismo.
Objetivo: en consecuencia, el propósito de esta investigación en particular es examinar la organización de la atención médica entre la población especificada de pacientes con IMH, en lo que respecta a su calidad de vida y la eficacia de los regímenes de tratamiento contemporáneos.
Método: para lograr esto, el estudio actual aplicó estrategias de síntesis narrativa y revisó la literatura sobre el diagnóstico de IMH, el manejo para soluciones quirúrgicas y los resultados de los pacientes. Esta evaluación abarcó los métodos terapéuticos anteriores y actuales, junto con la iluminación y el seguimiento de los pacientes con impacto en la claridad de la visión y el cociente general.
Resultados: de la revisión actual se desprende que los cirujanos utilizan ahora medios como la vitrectomía de pequeño calibre y sustancias farmacéuticas como la ocriplasmina, que mejoran las tasas de cierre del agujero macular y los niveles de agudeza visual cercana. Se ha enseñado a los pacientes/clientes y se han organizado seguimientos como parte de la atención organizativa para mejorar la calidad de vida, tal y como perciben los pacientes a partir de los cuestionarios de seguimiento que representan una mejora significativa de la función visual y las actividades.
Conclusiones: en este artículo se expone que los pacientes con HIM requieren un enfoque interprofesional estructurado y coordinado para su tratamiento junto con la cirugía contemporánea, lo que revela mejoras drásticas en los niveles de agudeza visual y en el bienestar general del paciente.
Palabras clave: Agujero Macular Idiopático; Atención Médica Organizativa; Agudeza Visual; Calidad de Vida; Vitrectomía; Educación del Paciente; Enfoque Multidisciplinar; Técnicas Quirúrgicas Modernas.
INTRODUCTION
It is important that medical care organization for patients diagnosed with IMH be enhanced to improve the overall and/or final patient result and quality of life of patients diagnosed with this particular disease.(1) The idiopathic macular hole is a condition pathologically seen in the retina that results in a full-thickness loss of the central vision of the retina, termed the macula. IMH commonly manifests in the elderly, significantly more in the female gender, and leads to profound impairments of visually demanding tasks such as reading or driving.(2,3) The exact pathophysiology of IMH depends on the vitreomacular interface, in which the vitreal gel located in the posterior portion of the eyeballs tends to pull away from the macular region forming a hole known as IMH. It is crucial to determine what an enhanced organization of treatment measures and innovative approaches means in relation to this disease to be able to cope with it successfully.(4) The clinical manifestation and the degree of visual dysfunction evolved in four distinct stages that delineate the IMH development. A shallow detachment of the foveal area without a full-thickness hole constitutes the characteristic features of the initial stage (Stage 1) and can manifest as a small yellow spot or a ring.(5,6) Advanced to stage 2 a full-thickness hole less than 400 micrometers in diameter occurs.(7) In Stage 3 the diameter of the hole is larger than 400 microns but without posterior vitreous separation and in Stage 4 there is posterior vitreous detachment (PVD) and full thickness of a macular hole. Some of the complications of IMH include if left untreated foresight vision volatility all these are reasons why treatment has to be effective and timely.(8,9,10,11)
Organizational medical management involves the systematic coordination of healthcare because it is important to make sure that patients get their treatment at the right time, at a single visit if possible.(12) As applied to IMH, this incorporates the coordination of transdisciplinary teams of care providers, patient empowerment, efficient diagnosis protocols, and real-time surveillance. The need for enhanced organizational care can be explained in the following ways.(13) We know that early detection of IMH is very crucial to prevent vision loss in patients. Imaging technologies like optical coherence tomography played a decisive role in the stages of macular hole development and in determining the approach to the treatment.(14) As mentioned above, comprehensive management of IMH may involve input from ophthalmologists, retinal specialists, optometrists, nurses, and many other healthcare workers.(15) This concept of care delivery also minimizes the risks of missing some signs that an isolated doctor might fail to observe and thus leads to an effective treatment having considered that all other specialties involved in the care of this patient are also represented in this team.(16,17,18,19)
It is crucial to raise patient awareness of their circumstances, the range of available therapies, and the need to follow an identified treatment regimen.(20) The educated patient commonly adheres to medical prescriptions/ advice alongside follow-up statements hence better results. Such changes as obtained through the implementation process therefore enhance the care map leading to fewer episodes of treatment prolongation.(21) For instance, techniques such as direct admission and referral as well as systemized scheduling in a shorter time can increase patients’ access to specialists and operations. Such a consequence becomes a concern for patients and physicians alike because the quality of life of patients with IMH gets compromised due to central vision loss.(22) To lose central vision means to experience difficulties with such activities as reading, driving a car, and many others, thus increasing dependence on the help of other people and having a bad impact on mental state. These impacts can be avoided by well-managed medical care in organizations where patients receive proper treatment at the right time which plays the role of preventing or reducing poor eyesight or vision impairment. Patient-reported outcome measures (PROMs) are widely applied to evaluate the quality of life of patients and the effectiveness of the treatments in improving the quality of the life of a patient by measuring the quality of visual function, psychological, and social functioning domains. In particular, IMH treatment has come a long way as of today, and modern treatment protocols reflect the improvement.(23,24) The management of IMH remains to be the vitrectomy because it allows the removal of the gelatinous material, vitreous, which tugs the macula. Changes in the method of surgery, new gel breakdown techniques and new intraocular gases or heavy liquids have enhanced the results of anatomical hole closure and improved vision. Substances like ocriplasmin can help to break the connection between vitreous and retina and encourage hole closure for some sufferers thus avoiding surgery.(25) Modern treatments can therefore be related to having fewer complications and shorter recovery times, which leads to enhanced patient satisfaction.
Literature Review
Current Understanding of Idiopathic Macular Hole
Clinical Presentation and Diagnosis
IMH is a condition that particularly affects the macular region of the eyes leading to vision impairments and it is most common among the elderly. Usually, the change occurs slowly with reduced vision mainly in the central area of the field of vision. Loss in this central vision can hinder the ability to read, recognize faces, and engage in any task that requires high resolution or detail.(28) One of the table signs is metamorphopsia, in which straight lines seem to be bent or curved making simple tasks even more challenging.(29) The initial symptoms of IMH could be mild and may not present initial manifestations or a mere vision complaint, which is why it takes some time before it is diagnosed.(30) As it becomes bigger, the central vision is further blurred and there may be only a grey or black centre of the visual field, whereas peripheral vision is often retained.(31)
Diagnosis of IMH is a bit challenging, and it is mostly done through imaging studies such as CT scans and MRIs. Morphologically, OCT is the most reliable noninvasive imaging modality in diagnosing and staging macular holes.(32) The advantages of OCT include high-resolution imaging in cross-sectional view of the retina in demonstration of the macular hole and its size. This imaging method can differentiate even minor structural alterations in the retina, which makes them very useful for diagnosis and tracking development. OCT and fundus photography can be employed to provide detailed characterizations of the macula and track evolution over time. Indirect ophthalmoscopy, but less frequently used, fluorescein angiography can be useful in the evaluation of the retinal blood flow and for the detection of additional abnormalities in the retina, which could pose a threat to the patient in the presence of the condition. Altogether, these diagnosis tools help quantify and categorize IMH accurately, which proves valuable in the management of the disease.(33)
Natural History and Progression
IMH progresses through four distinct stages, each characterized by different anatomical and clinical features: IMH progresses through four distinct stages, each characterized by different anatomical and clinical features(34,35) (table 1). Table 1 shows encapsulate the stages of IMH, providing a clear overview of the anatomical and symptomatic progression of the condition.
|
Table 1. The stages of Idiopathic Macular Hole |
|||
|
Stage |
Description |
Clinical Features |
Symptoms |
|
Stage 1 |
Impending Macular Hole |
Foveal detachment, small yellow spot or ring |
Mild visual disturbances may be asymptomatic |
|
Stage 2 |
Small Full-Thickness Macular Hole |
Full-thickness retinal hole < 400 microns in diameter |
Noticeable decrease in central vision |
|
Stage 3 |
Full-thickness macular Hole with Partial Posterior Vitreous Detachment |
Hole > 400 microns, vitreous partially attached to the macula |
Worsening central vision loss |
|
Stage 4 |
Full-thickness macular Hole with Complete Posterior Vitreous Detachment |
Large full-thickness hole, complete vitreous detachment |
Severe central vision impairment |
METHOD
Study Design
This narrative systematic review will provide a summary of current literature to evaluate the impact of organizational medical care in IMH patients, concerning their quality of life, as well as addressing modern treatments. The review of literature was done in according to guidelines for narrative reviews to ensure that literature was sufficient and systematically reviewed.
Eligibility criteria
To ensure a thorough and relevant review, we established the following inclusion and exclusion criteria: To ensure a thorough and relevant review, we established the following inclusion and exclusion criteria:
Inclusion Criteria
Studies published in peer-reviewed journals.
Research focusing on the organizational medical care of IMH patients.
Articles discussing the impact on quality of life and effectiveness of treatment protocols.
Studies employing various designs, including randomized controlled trials (RCTs), observational studies, case series, and qualitative research.
Publications in English.
Exclusion Criteria
Studies not specifically addressing IMH.
Articles focused on other retinal conditions or non-idiopathic macular holes.
Publications in languages other than English.
Abstracts, letters, and non-peer-reviewed articles.
Search Strategy
An extensive search was made in an electronic bibliographic database like PubMed, MEDLINE, EMBASE, and the Cochrane Library. “Idiopathic macular hole”, “Organizational medical care”, “Quality of life”, “Treatment protocols”, “Visual function”, “Patient outcomes”. This search was restricted to articles published between January 2015 and December 2023 to focus on the more recent and therefore possibly more relevant articles.
Study Selection
The first step of the screening was done based on the titles and abstracts of the research papers found during the initial search. The Pub Med interface was used to identify possibly related articles, their full texts obtained, and eligibility reviewed. The authors also performed the filtering and inclusion of the studies independently to reduce the chances of bias and enhance the study’s comprehensiveness. In cases where there were disagreements on what constituted high-quality work, the reviewers discussed the matter with the view of arriving at a consensus or consulting with a third reviewer.
Data Synthesis and statistical analysis
Due to the review’s narrative structure, it possessed a remarkable content quality, and as such, a qualitative synthesis approach was used. Qualitative data collected from the participants were analyzed and summarized according to perceived themes such as quality of life influenced by the organizational medical care, effectiveness of disease treatment interventions, and the patients’ experiences. The narrative synthesis will entail ‘mapping’ the current state of knowledge, identifying the proliferation of gaps in the literature and suggesting possibilities for the next course of action.
RESULTS
A systematic search employing a specific search strategy yielded 800 articles initially. Subsequent screening based on titles and abstracts narrowed down the selection to 150 articles for full-text evaluation. Upon thorough assessment, 40 articles were deemed relevant and subsequently utilized to inform and construct this review (figure 1).
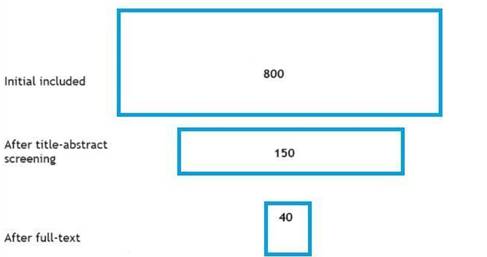
Figure 2. Summary of included studies
DISCUSSION
In this narrative review, we explored the impact of organizational medical care on patients with idiopathic macular hole (IMH), focusing on quality of life and the effectiveness of modern treatment protocols. Our review underscores the importance of a multidisciplinary approach, patient education, and rigorous follow-up in managing IMH effectively. IMH presents with central vision loss and metamorphopsia, significantly impairing daily activities. Diagnostic techniques such as OCT play a critical role in the identification and staging of the condition and enable timely management. IMH evolves through four stages, starting with stage 1a, impending macular hole, to stage 4, full-thickness macular hole with PVD. If left untreated, the outcome is poor and frequently leads to a patient’s irreversible loss of central vision. Hypertension otherwise known as high blood pressure is one of the leading causes of blindness and therefore early screening and follow-up are important so that the disease does not progress. Previous management, mainly involving vitrectomy with gas tamponade and positioning face down, has been regarded as highly effective for macular hole closure and restoration of vision. Innovations such as small-gauge vitrectomy and enzyme-protein drug ocriplasmin provide less invasive and faster recovery alternatives to traditional macular surgery. The advancements within post-operative care including position versatility also increase patients’ comfort and improvement. In managing IMH, various stakeholders such as ophthalmologists, retinal specialists, nurses, and other supportive staff should come together to ensure that appropriate care is provided. Complete patient education enables compliance with prescribed treatment modalities and an understanding of treatment procedures. Their follow-up examination should be scheduled to routinely check for any signs of complications and to evaluate the rate of healing.
Thus, IMH treatment reveals better visual function and quality of life in patients. This study discovered that patients’ perceived benefits of their vision recovery are related to functional well-being, psychological well-being, and quality of life. Standardized questionnaires for example the VFQ-25 help capture these improvements and are indicative of the overall patient benefits from proper IMH management. As such, the review highlights that better organization and systematization in the medical care process with the use of advanced treatment protocols results in better outcomes among IMH patients. A combination of reconstructive and microsurgical procedures, informed patients, and, finally, thorough follow-up facilitate not only strictly anatomical success but also a better quality of life in many patients. These results also indicate possibilities for future studies that must consider the cumulative effects of such approaches on patients and develop more effective approaches to delivering IMH interventions.
Hirneiss et al.(54) assessed the outcomes of macular hole surgery in terms of functional results and patients’ quality of life to determine its success rate and the factors affecting it. The study sample comprised fifty-nine patients with idiopathic macular holes who underwent pars plana vitrectomy. The patients underwent subsequent visits at predetermined durations subjected to clinical examination, optical coherence tomographic findings, and visual acuity. Furthermore, patients were asked to fill in the National Eye Institute 25-item Visual Function Questionnaire (VFQ-25) before surgery three months, and 12 months after the surgery for quality of visual function. Closed macular holes were observed in 97 % of the patients in the study; 57 of the 59 patients were successfully treated. Multimodal BCVA had also increased from a mean of 20 / 100 preoperatively to a mean of 20/ 34 at one-year follow-up (p = 0,02). This was despite good visual acuity in the fellow eye which was 20/27 and even though the overall VF–Q composite score improves from 75,9 ± 14,4 to 81,5 ± 14,2 one year after surgery revealed a significant improvement (p < 0,001). Surprisingly, it was not possible to compare overall visual quality of life with vision acuity. However, patients who had low initial visual acuity and those with poorer VFQ-25 scores had the highest benefit gained from the surgery.
A recent meta-analysis(62) investigated a modern model for macular hole management. They compared the inverted internal limiting membrane (ILM) flap technique with that of ILM peeling for the treatment of small and medium-sized macular holes (MHs). The literature search was conducted in PubMed, Web of Science, Embase, and the Cochrane Library up to January 2023 and limited to experimental-based studies. Three RCTs involving 212 eyes and two non-RCTs involving 57 eyes were evaluated. The findings revealed no significant difference in the MH closure rate between the two techniques (OR = 0,29, 95 % CI: 0,04-1,96, p = 0,33). Furthermore, there was no statistically significant difference in the visual acuity or the external limiting membrane (ELM) and ellipsoid zone (EZ) at three months (ELM OR = 0,88, EZ OR = 0,85) and twelve months post-operation (ELM OR = 0,0) Finally, both the inverted ILM flap technique and the standard ILM peeling have similar results in terms of improvement in visual acuity and anatomical restoration of MHs less than 400 μm.
A previous review analyses(63) the available surgical interventions for refractory and atypical MH and outlines an approach in complex cases. This implies that small MHs, new, small MHs that are ≤200 μm and new MHs that are small, and inferior can be effectively treated through pars plana vitrectomy, while the large MHs that are intermediate, 200-300 μm as well as large MHs that are superior and posterior ought to have their internal limiting membrane peeled. With significant risk factors suggesting the possibility of surgical failure in MHs of 400 micrometers or more, the primary treatment plan should be to develop an ILM flap and different techniques of flap creation are described. For very large MHs greater than or equal to 700 μm or in incredibly tough cases, auto-RPE transplants and other new treatments are advised. Overall, while peer MH usually has excellent surgical outcomes, atypical and refractory MHs need more intensive intraoperative and postoperative management for the best outcomes and improved visual acuity. Thus, the identification of the best techniques is essential, which, with the various methods offered, has to be combined with the proper choice of patients. Eight studies were selected of which had assigned 509 eyes (500 patients). Also, there were different times of positioning carefully in the prone position five trials using 10 days of prone position, two trials using five days, and two trials using only three days. One to six months after the surgery anatomical hole closure was the primary outcome and it was achieved in 95 of every 100 eyes of participants who were advised to be facedown for at least three days after surgery out of 709 total eyes from eight studies, with low heterogeneity (I² = 44 %). In the 327 eyes with macular hole equal to or greater than 400 μm, among participants recommended to position, face-down, hole closure was achieved 94/100 and among those not recommended 84/100 (RR 1,08; 95 % CI: 0,93– 1,26; five studies; I² = 62 %). The sample included 129 eyes of patients with macular hole of less than 400μm diameter; the hole closure was noted in face down positioning advised group being 100 of 100 eyes and in face down positioning not advise group being 96 of 100 eyes, (RR = 1,03; 95 % CI 0,97- 1,11, 4 trials, I² = 0 %). There remained moderate uncertainty in these results: imprecision was downgraded with AOR CIs including value = 1.
CONCLUSION
The organisational medical care of the patient with IMH shows that a systematic and collaborative management model is highly effective in delivering positive outcomes for the diagnosis. Epidemiologically easier access to health care, better diagnostic methods, minimal invasive surgery, patient understanding of ailment and aggressive follow up yields better visual acuity and disease life. Conventional present-day definitive care in macular hole include vitrectomy with gas tamponade and the new technologies involves in small gauge vitrectomy and pharmacologic agents exhibits vivid success rate in hole closure and increases vision acuity. Integration of patient-reported outcomes demonstrates that clinicians need to improve not only the clinical management of the disorder but also the quality of life of the patients they are treating. Subsequent studies should try to further enhance these approaches, with the aim of monitoring and measuring more extensive effects and making adjustments in the organisation of patients’ treatment in order to achieve stronger, longer outcomes for this specific complication.
Recommendations and Future Research
To improve Idiopathic Macular Hole (IMH) management, a multidisciplinary team approach is recommended, emphasizing the use of OCT for accurate staging and prognosis. Adolescents should receive specialized care, and innovative treatments like small-gauge vitrectomy and ocriplasmin should be incorporated to enhance recovery. Patient education and support are also crucial.
Future research should focus on long-term outcomes of current interventions, individualized treatment plans, the use of non-invasive treatments, and continuous improvement of post-surgery care and interventions.
REFERENCES
1. Bikbova G, Oshitari T, Baba T, Yamamoto S, Mori K. Pathogenesis and Management of Macular Hole: Review of Current Advances. J Ophthalmol [Internet]. 2019 May 2;2019:1–7. Available from: https://www.hindawi.com/journals/joph/2019/3467381/
2. Fallico M, Jackson TL, Chronopoulos A, Hattenbach L, Longo A, Bonfiglio V, et al. Factors predicting normal visual acuity following anatomically successful macular hole surgery. Acta Ophthalmol [Internet]. 2021 May 24;99(3). Available from: https://onlinelibrary.wiley.com/doi/10.1111/aos.14575
3. Rezende FA, Ferreira BG, Rampakakis E, Steel DH, Koss MJ, Nawrocka ZA, et al. Surgical classification for large macular hole: based on different surgical techniques results: the CLOSE study group. Int J Retin Vitr [Internet]. 2023 Jan 30;9(1):4. Available from: https://journalretinavitreous.biomedcentral.com/articles/10.1186/s40942-022-00439-4
4. Gonzalez-Cortes JH, Bilgic A, De Los Santos Polanco J, Treviño-Herrera AB, Sudhalkar A, Gonzalez-Cantu JE, et al. Spontaneous closure of an idiopathic macular hole after epiretinal membrane development. Am J Ophthalmol Case Reports [Internet]. 2023 Mar;29:101767. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2451993622005138
5. Rizak G, Maltsev D, Karkimbayeva G, Vivsyannuk V, Barabanchyk O. European and National measurements of Molecular and Immunological aspects of Diagnosis, Prevention, and Treatment of Coronavirus infection. Res J Pharm Technol [Internet]. 2023 Aug 31;3929–35. Available from: https://rjptonline.org/AbstractView.aspx?PID=2023-16-8-66
6. Boyarchuk O, Komorovsky R, Kovalchuk T, Denefil O. Socio-demographic and medical predictors of rheumatic heart disease in a low-risk population. Pediatr Pol [Internet]. 2018;93(4):325–30. Available from: https://www.termedia.pl/doi/10.5114/polp.2018.77998
7. Watanabe M, Yokota H, Aso H, Hanazaki H, Hanaguri J, Yamagami S, et al. Development of Stage 4 Macular Hole after Spontaneous Closure in a Patient with Stage 2 Macular Hole and a Lamellar Macular Hole-Associated Epiretinal Proliferation. Case Rep Ophthalmol [Internet]. 2021 Jun 8;12(2):481–4. Available from: https://karger.com/COP/article/doi/10.1159/000513132
8. Chun JW, Kim CH, Kim JY, Oh HS, Kim SH, Kwon OW, et al. Prevalence and Progression of Stage 0 Macular Hole in Fellow Eyes of Patients with Idiopathic Full-thickness Macular Hole. Korean J Ophthalmol [Internet]. 2021 Apr 5;35(2):107–11. Available from: http://ekjo.org/journal/view.php?doi=10.3341/kjo.2020.0078
9. Bentaleb Machkour Z, Garweg JG, Bandello F, Denis P, Kodjikian L. Differences in the presentation of stage 1 macular holes illustration by optical coherence tomography. Eur J Ophthalmol [Internet]. 2021 May 11;31(3):NP29–34. Available from: http://journals.sagepub.com/doi/10.1177/1120672120904661
10. CHAN A, DUKER J, SCHUMAN J, FUJIMOTO J. Stage 0 macular holesObservations by optical coherence tomography. Ophthalmology [Internet]. 2004 Nov;111(11):2027–32. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0161642004009352
11. Uemura A, Miyake S, Funatsu R, Yamakiri K. CLINICAL CHARACTERISTICS AND SURGICAL OUTCOMES IN STAGE 4 MACULAR HOLE WITH EPIRETINAL PROLIFERATION. Retina [Internet]. 2023 Sep;43(9):1550–6. Available from: https://journals.lww.com/10.1097/IAE.0000000000003848
12. Gupta M, Shah HR, Taber K. MEDICAL MANAGEMENT OF FULL-THICKNESS MACULAR HOLES: Topical therapy may be a good option for a subset of patients. Retin Today. 2022;
13. Tieger MG, Kim LA, Vavvas DG. SPONTANEOUS CLOSURE AND RECURRENT OPENING TIMES TWO OF A MACULAR HOLE IN A SURGICALLY NAIVE EYE. Retin Cases Brief Rep [Internet]. 2023 Sep;17(5):581–3. Available from: https://journals.lww.com/10.1097/ICB.0000000000001244
14. Elyashiv S, Fogel Levin M, Zloto O, Neimark E, Najjar R, Moisseiev J, et al. Epidemiology of Pars Plana Vitrectomy in the Elderly: A Retrospective 10-Year Survey of 592 Cases. Clin Interv Aging [Internet]. 2021 Jun;Volume 16:1007–12. Available from: https://www.dovepress.com/epidemiology-of-pars-plana-vitrectomy-in-the-elderly-a-retrospective-1-peer-reviewed-fulltext-article-CIA
15. Alsarhani W, Saifaldein A, Abu El-Asrar A. A novel mechanism of macular holes in patients with Behçet’s uveitis. Saudi J Ophthalmol [Internet]. 2022;36(4):394. Available from: https://journals.lww.com/10.4103/sjopt.sjopt_102_21
16. The Future of Mortgage Financing in the Era of Fintech: A Systematic Review. Futur Econ [Internet]. 2024 Apr 2;31–47. Available from: https://www.futurity-econlaw.com/index.php/FEL/article/view/223
17. Analysis of Methods and Tools for Visualising Anatomy in the Professional Training of Future Design Teachers. Futur Soc Sci [Internet]. 2023 Jun 20;59–70. Available from: https://futurity-social.com/index.php/journal/article/view/15
18. Yuryk O, Barabanchyk O, Malets M. Innovations in medicine: modern challenges, future definitions: A narrative review. Futur Med. 2022 Jun;23–30.
19. Alimukhamedov U. Acute renal failure in newborns in the practice of a pediatrician of the future. Futur Med [Internet]. 2022 Dec 30 [cited 2023 Dec 9];1(4):17–24. Available from: https://futurity-medicine.com/index.php/fm/article/view/17
20. Riaz S, Mirza UT, Iqbal K, Tariq Khan M, Mirza KA, Hanif J. The Common Indications of Pars plana vitrectomy (PPV) for posterior Segment Ocular diseases in patients from a Private Retina Clinic. Pakistan J Med Heal Sci [Internet]. 2021 Oct 30;15(10):2759–62. Available from: https://pjmhsonline.com/published-issues/2021/october/102759
21. Singh A, Sengupta S, Rasheed MA, Jayakumar V, Lakshminarayanan V. Uncertainty aware and explainable diagnosis of retinal disease. 2021 Jan 26; Available from: http://arxiv.org/abs/2101.12041
22. Danielescu C, Stanca HT, Balta F. The Management of Lamellar Macular Holes: A Review. J Ophthalmol [Internet]. 2020 Feb 21;2020:1–10. Available from: https://www.hindawi.com/journals/joph/2020/3526316/
23. Taylor DJ, Jones L, Edwards L, Crabb DP. Patient-reported outcome measures in ophthalmology: too difficult to read? BMJ Open Ophthalmol [Internet]. 2021 Jun 15;6(1):e000693. Available from: https://bmjophth.bmj.com/lookup/doi/10.1136/bmjophth-2020-000693
24. Braithwaite T, Calvert M, Gray A, Pesudovs K, Denniston A. The use of patient-reported outcome research in modern ophthalmology: impact on clinical trials and routine clinical practice. Patient Relat Outcome Meas [Internet]. 2019 Jan;Volume 10:9–24. Available from: https://www.dovepress.com/the-use-of-patient-reported-outcome-research-in-modern-ophthalmology-i-peer-reviewed-article-PROM
25. Chen X, Li M, You R, Wang W, Wang Y. Efficacy and Safety of Ocriplasmin Use for Vitreomacular Adhesion and Its Predictive Factors: A Systematic Review and Meta-Analysis. Front Med [Internet]. 2022 Jan 13;8. Available from: https://www.frontiersin.org/articles/10.3389/fmed.2021.759311/full
26. Caporossi T, Ripa M, Governatori L, Scampoli A, Gambini G, Rizzo C, et al. The current surgical management of refractory full-thickness macular holes. Expert Rev Ophthalmol [Internet]. 2022 Jan 2;17(1):25–36. Available from: https://www.tandfonline.com/doi/full/10.1080/17469899.2022.2045951
27. Ittarat M, Somkijrungroj H, Chansangpetch S, Pongsachareonnont P. Literature Review of Surgical Treatment in Idiopathic Full-Thickness Macular Hole. Clin Ophthalmol [Internet]. 2020 Jul;Volume 14:2171–83. Available from: https://www.dovepress.com/literature-review-of-surgical-treatment-in-idiopathic-full-thickness-m-peer-reviewed-article-OPTH
28. Premi E, Donati S, Azzi L, Porta G, Metrangolo C, Fontanel L, et al. Macular Holes: Main Clinical Presentations, Diagnosis, and Therapies. Forlini M, editor. J Ophthalmol [Internet]. 2022 Apr 11;2022:1–10. Available from: https://www.hindawi.com/journals/joph/2022/2270861/
29. Xia F, Lyu J, Fei P, Zhao P. Diagnosis of complicated FEVR preoperatively and intra−/post-operatively: characteristics and risk factors for diagnostic timing. BMC Ophthalmol [Internet]. 2019 Dec 8;19(1):126. Available from: https://bmcophthalmol.biomedcentral.com/articles/10.1186/s12886-019-1128-8
30. Orozco-Gómez LP, Martínez-Almada J, Moreno-Ferreyra LG, Hernández-Salazar L, Orozco-Moguel A, Dávila-Bárcena A, et al. Ocular repercussions of suspected abusive head trauma. Rev Mex Oftalmol (English Ed [Internet]. 2021 Jan 25;95(1). Available from: http://www.rmo.com.mx/frame_eng.php?id=225
31. Bier C, Kampik A, Gandorfer A, Ehrt O, Rudolph G. Ablatio retinae bei Kindern und Jugendlichen. Spezifische Befundmerkmale. Der Ophthalmol [Internet]. 2020 Feb 18;117(2):132–9. Available from: http://link.springer.com/10.1007/s00347-019-0937-8
32. Azzolini C. Macular Hole: From Diagnosis to Therapy. J Ophthalmol [Internet]. 2020 Mar 23;2020:1–2. Available from: https://www.hindawi.com/journals/joph/2020/1473763/
33. Dong Z, Pan Q, Zhang Z, Zhang Z. A case of von Hippel‑Lindau syndrome with optic disc pit and macular hole. Chinese J Ophthalmol. 2023;
34. Terasaki H, Yamashita T, Funatsu R, Nomoto S, Fujiwara K, Shiihara H, et al. Effect of the macular shape on hole findings in idiopathic macular hole differs depending on the stage of the macular hole. Sci Rep [Internet]. 2023 Sep 16;13(1):15367. Available from: https://www.nature.com/articles/s41598-023-42509-z
35. Dhami A, Dhami NB, Dhami GS. Spontaneous closure of stage 2 macular hole after cataract surgery. Adv Ophthalmol Vis Syst [Internet]. 2020 Apr 23;10(2):45–6. Available from: https://medcraveonline.com/AOVS/spontaneous-closure-of-stage-2-macular-hole-after-cataract-surgery.html
36. Jain M, Narayanan R, Gopal L, Padhi TR, Behera UC, Panda KG, et al. Post-vitrectomy secondary macular holes: Risk factors, clinical features, and multivariate analysis of outcome predictors. Indian J Ophthalmol [Internet]. 2023 May;71(5):2053–60. Available from: https://journals.lww.com/10.4103/ijo.IJO_1749_22
37. Zhao X, Li Y, Ma W, Lian P, Yu X, Chen S, et al. Macular buckling versus vitrectomy on macular hole associated macular detachment in eyes with high myopia: a randomised trial. Br J Ophthalmol [Internet]. 2022 Apr;106(4):582–6. Available from: https://bjo.bmj.com/lookup/doi/10.1136/bjophthalmol-2020-317800
38. Kim DY, Jo YJ, Kim JY, Chae JB, Cho IH, Kim HD, et al. Surgical Outcomes of Vitrectomy for Macular Hole-induced Retinal Detachment According To Various Surgical Methods: A Multicenter Retrospective Study. Semin Ophthalmol [Internet]. 2021 Nov 17;36(8):728–33. Available from: https://www.tandfonline.com/doi/full/10.1080/08820538.2021.1900288
39. Thompson JT. Advantages and Limitations of Small Gauge Vitrectomy. Surv Ophthalmol [Internet]. 2011 Mar;56(2):162–72. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0039625710001530
40. Pei M, Zhao X, Wan G. A Systematic Review and Meta-Analysis of Clinical Outcomes of Small Gauge Vitrectomy with or without Intravitreal Anti-Vascular Endothelial Growth Factor Agents Pretreatment for Proliferative Diabetic Retinopathy. Ophthalmic Res. 2023;
41. Khanani AM, Constantine RN, Blot KH, Lescrauwaet B, Szurman P. Effectiveness of ocriplasmin in real‐world settings: A systematic literature review, meta‐analysis, and comparison with randomized trials. Acta Ophthalmol [Internet]. 2021 Sep 26;99(6). Available from: https://onlinelibrary.wiley.com/doi/10.1111/aos.14686
42. Stalmans P, Benz MS, Gandorfer A, Kampik A, Girach A, Pakola S, et al. Enzymatic Vitreolysis with Ocriplasmin for Vitreomacular Traction and Macular Holes. N Engl J Med [Internet]. 2012 Aug 16;367(7):606–15. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMoa1110823
43. Khan MA, Haller JA. Ocriplasmin for Treatment of Vitreomacular Traction: An Update. Ophthalmol Ther [Internet]. 2016 Dec 12;5(2):147–59. Available from: http://link.springer.com/10.1007/s40123-016-0062-6
44. Mirshahi A, Fadakar K, Mirshahi R, Khalili Pour E, Ebrahimiadib N, Ghassemi F, et al. Alterations in choroidal vascular parameters following panretinal photocoagulation using enhanced-depth imaging optical coherence tomography in diabetic retinopathy. Graefe’s Arch Clin Exp Ophthalmol [Internet]. 2022 Feb 1;260(2):459–69. Available from: https://link.springer.com/10.1007/s00417-021-05401-y
45. Youn S, Loshusan B, Armstrong JJ, Fraser JA, Hamann S, Bursztyn LLCD. A Comparison of Diagnostic Accuracy of Imaging Modalities to Detect Optic Disc Drusen: The Age of Enhanced Depth Imaging Optical Coherence Tomography. Am J Ophthalmol [Internet]. 2023 Apr;248:137–44. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0002939422004858
46. Schmoele-Thoma B, Zareba AM, Jiang Q, Maddur MS, Danaf R, Mann A, et al. Vaccine Efficacy in Adults in a Respiratory Syncytial Virus Challenge Study. N Engl J Med [Internet]. 2022 Jun 23 [cited 2023 Oct 26];386(25):2377–86. Available from: https://pubmed.ncbi.nlm.nih.gov/35731653/
47. Dagnelie G. Retinal implants. Curr Opin Neurol [Internet]. 2012 Feb;25(1):67–75. Available from: http://journals.lww.com/00019052-201202000-00012
48. Patrini D, Lawrence D, Lampridis S, Minervini F, Giorgi L, Palermo R, et al. The role of a multidisciplinary team in chest wall trauma management. J Vis Surg [Internet]. 2020 Apr;6:19–19. Available from: http://jovs.amegroups.com/article/view/33651/html
49. Mahan M, Purt B. Ocular Trauma Prevention Strategies and Patient Counseling [Internet]. StatPearls. 2024. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19789585
50. Shelswell NL. Perioperative Patient Education for Retinal Surgery. AORN J [Internet]. 2002 Apr;75(4):801–7. Available from: https://aornjournal.onlinelibrary.wiley.com/doi/10.1016/S0001-2092%2806%2961636-0
51. AlHilali S, AlMuammar A, AlKahtani E, Khandekar R, AlJasser A. Preferred method of education among patients in ophthalmic care in Saudi Arabia. Middle East Afr J Ophthalmol [Internet]. 2016;23(2):168. Available from: https://journals.lww.com/10.4103/0974-9233.171780
52. Kang HK, Luff AJ. Management of retinal detachment: a guide for non-ophthalmologists. BMJ [Internet]. 2008 May 31;336(7655):1235–40. Available from: https://www.bmj.com/lookup/doi/10.1136/bmj.39581.525532.47
53. Hirneiss C, Neubauer AS, Gass CA, Reiniger IW, Priglinger SG, Kampik A, et al. Visual quality of life after macular hole surgery: outcome and predictive factors. Br J Ophthalmol [Internet]. 2007 Apr 1;91(4):481–4. Available from: https://bjo.bmj.com/lookup/doi/10.1136/bjo.2006.102376
54. Hirneiss C, Neubauer AS, Gass CA, Reiniger IW, Priglinger SG, Kampik A, et al. Visual quality of life after macular hole surgery: outcome and predictive factors. Br J Ophthalmol [Internet]. 2007 Apr 1;91(4):481–4. Available from: https://bjo.bmj.com/lookup/doi/10.1136/bjo.2006.102376
55. Tyler SL, Maltby J, Paterson KB, Hutchinson C V. Reduced Vision-Related Quality of Life in Dementia: A Preliminary Report. J Alzheimer’s Dis [Internet]. 2022 May 3;87(1):239–46. Available from: https://www.medra.org/servlet/aliasResolver?alias=iospress&doi=10.3233/JAD-215435
56. Lešin Gaćina D, Škegro B, Jandroković S, Škegro I, Bešlić I, Bukvić M. Psychometric properties of the Croatian version of the 25-item National Eye Institute Visual Function Questionnaire (NEI VFQ-25). Int Ophthalmol [Internet]. 2021 Dec 26;41(12):4025–36. Available from: https://link.springer.com/10.1007/s10792-021-01975-y
57. Jelin E, Wisløff T, Moe MC, Heiberg T. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ 25) in a Norwegian population of patients with neovascular age-related macular degeneration compared to a control population. Health Qual Life Outcomes [Internet]. 2019 Dec 14;17(1):140. Available from: https://hqlo.biomedcentral.com/articles/10.1186/s12955-019-1203-0
58. Shanbhag SS, Tahboub MA, Chodosh J, Saeed HN. Visual function and quality of life in patients with Stevens-Johnson syndrome who received acute protocol-based ocular care. Front Toxicol [Internet]. 2022 Nov 2;4. Available from: https://www.frontiersin.org/articles/10.3389/ftox.2022.992696/full
59. Márquez-Vergara IS, Ríos-Nequis GJ, Pita-Ortíz IY, Pérez-Cano HJ, Somilleda-Ventura SA. Vision-related quality of life after surgery for vitreoretinal disorders in a Mexican population: an observational study. Sci Rep [Internet]. 2023 Mar 25;13(1):4885. Available from: https://www.nature.com/articles/s41598-023-32152-z
60. Montesinos GM, Rojas Alvarez E, Cabrera STG, Márquez Marchán AC, Urias NP. Clinical-surgical Characteristics of Patients with Macular Hole. Exilaser Ophthalmological Center. Cuenca, Ecuador. 2015-2019. Open Ophthalmol J [Internet]. 2023 Jun 22;17(1). Available from: https://openophthalmologyjournal.com/VOLUME/17/ELOCATOR/e187436412305120/
61. Wang Y, Liang X, Gao M, Liu J, Liu L, Liu W. Vision-related quality of life after pars plana vitrectomy with or without combined cataract surgery for idiopathic macular hole patients. Int Ophthalmol [Internet]. 2019 Dec 29;39(12):2775–83. Available from: http://link.springer.com/10.1007/s10792-019-01124-6
62. Li P, Li L, Wu J. Inverted Internal Limiting Membrane Flap versus Internal Limiting Membrane Peeling for &lt;400 μm Macular Hole: A Meta-Analysis and Systematic Review. Ophthalmic Res [Internet]. 2023;66(1):1342–52. Available from: https://karger.com/ORE/article/doi/10.1159/000534873
63. Marlow E, Mahmoud T. Current management strategies for atypical macular holes. Taiwan J Ophthalmol [Internet]. 2021;11(3):221. Available from: https://journals.lww.com/10.4103/tjo.tjo_26_20
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest
AUTHORSHIP CONTRIBUTION
Conceptualization: Dastan Kyrykbayev, Marfuga Amanzhanovna Oteulieva, Ardak Mukhamedzhanovna Auezova, Gulnar Kairatovna Zhurgumbayeva.
Formal analysis: Dastan Kyrykbayev, Marfuga Amanzhanovna Oteulieva, Ardak Mukhamedzhanovna Auezova, Gulnar Kairatovna Zhurgumbayeva.
Research: Dastan Kyrykbayev, Marfuga Amanzhanovna Oteulieva, Ardak Mukhamedzhanovna Auezova, Gulnar Kairatovna Zhurgumbayeva.
Drafting - original draft: Dastan Kyrykbayev, Marfuga Amanzhanovna Oteulieva, Ardak Mukhamedzhanovna Auezova, Gulnar Kairatovna Zhurgumbayeva.
Writing - proofreading and editing: Dastan Kyrykbayev, Marfuga Amanzhanovna Oteulieva, Ardak Mukhamedzhanovna Auezova, Gulnar Kairatovna Zhurgumbayeva.