SYSTEMATIC REVIEW
Cognitive Impairment in the Elderly: A systematic review of the literature
Deterioro cognitivo en adultos mayores: Una revisión sistemática de la literatura
Nubia Hernández-Flórez1 ![]() *, Elisama Beltrán de la Rosa1
*, Elisama Beltrán de la Rosa1 ![]() *, Olena Klimenko2
*, Olena Klimenko2
![]() *, Maria José Orozco Santander1
*, Maria José Orozco Santander1 ![]() *, Francis Araque-Barboza1
*, Francis Araque-Barboza1 ![]() *, Johana Vásquez-Torres1
*, Johana Vásquez-Torres1 ![]() *
*
1Metropolitan University of Barranquilla, Psychology Program. Barranquilla, Colombia.
2University Institute of Envigado, Psychology Program. Envigado, Colombia.
Cite as: Hernández-Flórez N, Beltrán de la Rosa E, Klimenko O, Orozco Santander MJ, Araque-Barboza F, Vásquez-Torres J. Cognitive Impairment in the Elderly: A systematic review of the literature. Salud, Ciencia y Tecnología. 2024; 4:799. https://doi.org/10.56294/saludcyt2024799
Submitted: 09-11-2023 Revised: 03-01-2024 Accepted: 13-02-2024 Published: 14-02-2024
Editor: Dr.
William Castillo-González ![]()
ABSTRACT
This article focuses on the study of cognitive impairment in the elderly. The general objective focuses on the analysis of three variables present in the selected articles which are cognitive impairment and quality of life, which explores the perceptions associated with the well-being and satisfaction of older adults, understanding the dynamics of personal achievement, social relationships, autonomy, and quality of life that impact on the conditions of integral health within the context of integral well-being. A second variable of mood alterations and comorbid pathologies, where it was identified that depression and anxiety are pathologies that cause emotional alterations in older adults and interfere in the development of symptoms associated with pathological comorbidities, and the third variable is lifestyle and neurocognition includes protective elements associated with physical activity, nutrition and socialization processes that promote active and healthy aging. The methodology is of quantitative design with a bibliometric approach under the context of a systematic literature review. Taking into account, the prism methodology that responds to the approach of Boolean equations that were used to perform the analysis and categorization of the documents using variables. Finally, it is concluded the need to make cognitive and behavioral changes in the elderly through a differentiated evaluation for each patient, thus minimizing the effects in the social, family, economic, affective, and emotional spheres
Keywords: Older Adults; Cognitive Impairment; Quality of Life; Comorbid Pathologies; Neuro Cognition.
RESUMEN
Este artículo se centra en el estudio del deterioro cognitivo en las personas mayores. El objetivo general se centra en el análisis de tres variables presentes en los artículos seleccionados que son deterioro cognitivo y calidad de vida, donde se exploran las percepciones asociadas al bienestar y satisfacción de los adultos mayores, comprendiendo las dinámicas de realización personal, relaciones sociales, autonomía y calidad de vida que impactan en las condiciones de salud integral en el contexto del bienestar integral. Una segunda variable de alteraciones del estado de ánimo y patologías comórbidas, donde se identificó que la depresión y la ansiedad son patologías que causan alteraciones emocionales en los adultos mayores e interfieren en el desarrollo de síntomas asociados a comorbilidades patológicas, y la tercera variable es estilo de vida y neurocognición incluye elementos protectores asociados a la actividad física, nutrición y procesos de socialización que promueven un envejecimiento activo y saludable. La metodología es de diseño cuantitativo con un enfoque bibliométrico bajo el contexto de una revisión sistemática de la literatura. Teniendo en cuenta, la metodología prisma que responde al planteamiento de ecuaciones booleanas que se utilizaron para realizar el análisis y categorización de los documentos mediante variables. Finalmente, se concluye la necesidad de realizar cambios cognitivos y conductuales en el adulto mayor a través de una evaluación diferenciada para cada paciente, minimizando así los efectos en las esferas sociales, familiares, económicas, afectivas y emocionales.
Palabras clave: Adultos Mayores; Deterioro Cognitivo; Calidad de Vida; Patologías Comórbidas; Neuro Cognición.
INTRODUCTION
Cognitive impairment in older adults is a relevant topic within the scientific interests in the field of health and psychology because the correlational influence directly impacts the quality of life and well-being of the population. Thus, the approach to aging is one of the most prominent topics of analysis of phenomena during the 21st century.(1) Clinical compromises that are associated with cognitive impairment affect older adults who present in gradual changes due to increasing age and converge in neurocognitive disorders with serious implications in brain functional structures, such as Alzheimer's disease and dementia.(2)
The objective within the context of the present systematic review focused on performing an analysis of the most updated and relevant scientific advances regarding cognitive impairment in the elderly. In this way, a complete and updated understanding of the variables of affectation, risk factors, and main factors involved in the processes of prevention and treatment, which involve elements of quality of life in older adults, is addressed.(3) The current challenges in the field of cognitive impairment involve generating and contributing knowledge from the field of clinical psychology and neurosciences, because this problem is not only limited to the decline of mental abilities but requires an integrative and holistic understanding, which allows to adequately address the main implications that arise in older adults.(4)
Considering the above mentioned, three variables were identified, within the analytical development of the articles, the first one, related to cognitive impairment and quality of life, which explores the perceptions associated with the well-being and satisfaction of older adults, understanding the dynamics of personal achievement, social relationships, autonomy, and quality of life that impact on the conditions of integral health within the context of integral well-being.(5) A second variable determined is mood alterations and comorbid pathologies, where it was identified that depression and anxiety are the main pathologies that cause emotional alterations in older adults and, therefore, interfere in the development of symptoms associated with pathological comorbidities. The third variable analyzed is lifestyle and neurocognition, which includes protective elements associated with physical activity, nutrition and socialization processes that promote active and healthy aging.(3)
Because there is an impact on the life of older adults that causes a detriment in cognitive abilities, since, as these diminish, individuals usually experience greater difficulties in the development of daily tasks, which implies a greater impact on the psychological function that, in turn, generates affectations in the social, family, economic, affective and emotional spheres. Therefore, it is necessary that when identifying cognitive and behavioral changes in older adults, an evaluation process is initiated to intervene on time the pathological symptomatology through appropriate strategies and processes from the field of psychology and neurosciences, which have scientifically demonstrated that, through cognitive stimulation exercises, psychological interventions aimed at lifestyle modifications, have proven to be effective in improving the conditions of aging.(6)
Finally, Figueroa-Varela et al.(7) cognitive deterioration as a normal part of aging requires social and family support, which is essential to preserve the conditions of cognitive functionality of older adults. Support networks provide safe spaces for patients because they can express their emotions, identify stressful situations and receive the comfort that helps to improve their mental health conditions,(4) in this way, the help received, allows them to maintain aspects of autonomy and dignity that may arise in situations of psychosocial vulnerability, additionally, the participation of other family members, benefits the patient, relieves stress and generates better strategies that help maintain a connection between perceived health and emotional well-being.(5)
METHODOLOGY
The methodological approach for this study was oriented under the quantitative design with a bibliometric approach in the context of the systematic literature review.(8) Taking into account the prism methodology that responds to the approach of Boolean equations that were used to perform the analysis and categorization of the documents by variables. In this way, the scientific advances reported by researchers on the subject of cognitive impairment in the elderly were synthesized and evaluated.(9) The PRISMA Method (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) generated a structure that allowed defining the research question, which took as a starting point the following question: What are the risk factors and interventions to prevent cognitive impairment in older adults?
The selection and analysis of the categorization of the documents were carried out utilizing a selection through the open journal system (OJS) that took as a starting point the databases PubMed, Science Direct, and Web of Science, which included the methodological precision centered on the variables denominated: Cognitive deterioration and quality of life; mood alterations and comorbid pathologies and finally lifestyle and neurocognition. The sample unit reported thirty-six articles related to primary research, which focused on the last five years as a study period and in the English language.
Inclusion criteria: primary studies were included, taking into account, observational studies with case-control cohort methodologies where reports were identified only in English studies of the last five years);(10) research advances that reported cognitive impairment as a primary or secondary variable condensing the related information that generates reports within the thematic area of neuropsychology and neurosciences.
Exclusion criteria: Scientific reports generated by gray literature that did not provide specific data about cognitive impairment in older adults were excluded. Likewise, documents that did not contain a reported methodology were excluded and discarded for low quality. Likewise, manuscripts that did not have peer review and those that did not address risk and interventional factors related to quality of life were discarded, except for the PICO system related to the research question.(11)
Search strategies: the exploration of the documents was carried out by means of paid databases available for the research system designed for academic purposes. The relevance and pertinence of the topics of interest raised in the contributions and publications that were developed in the last five years were reviewed, using relevant and controlled search terms that included characteristics associated with language, year of publication, type of study, and target population.(8)
Data collection process: An exhaustive search was carried out in the databases Pubmed, Science Direct, and Web of Science, using search terms that allowed delving into the research processes, and identifying the study variables that had a direct impact on the subject. Taking into account the answers provided by the scientific community, through the contributions made by experts on the subject. A data extraction process was developed that allowed the collection of relevant information from the selected studies. Evaluating the quality by using tools directed through the PRISMA checklist, Cochrane Risk, generating a quantitative analysis that allowed synthesizing the main studies included.(12)
Search terms used: ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Quality of life" OR "well-being") AND ("Cognitive impairment" OR "dementia") ("Prevention" OR "intervention") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Risk factors" OR "predisposing") AND ("Cognitive impairment" OR "dementia") AND ("Prevention" OR "intervention") AND ("Older adults" OR "elderly") older adults" OR "elderly") AND ("risk factors" OR "predisposing factors") AND ("cognitive impairment" OR "dementia") AND ("older adults" OR "elderly") AND ("family impact") AND ("cognitive impairment" OR "dementia") AND ("older adults" OR "elderly") AND ("cognitive impairment" OR "dementia") AND ("older adults" OR "elderly") ("Cognitive Impairment" OR "Dementia") AND ("Older Adults" OR "Elderly")("Neuropsychological Assessment") AND ("Cognitive Impairment" OR "Dementia") AND ("Older Adults" OR "Elderly") AND ("Social Factors") ("Physical Exercise" OR "Physical Activity") AND ("Cognitive Impairment" OR "Dementia") AND ("Neuropsychological Assessment") AND ("Cognitive Impairment" OR "Dementia") AND ("Cognitive physical activity") AND ("Cognitive Impairment" OR "dementia") AND ("Older Adults" OR "elderly") AND ("Nutrition" OR "diet") AND ("Cognitive Impairment" OR "dementia") AND ("Older Adults" OR "elderly") AND ("Cognitive Strategies" OR "cognitive stimulation") AND ("Cognitive Strategies" OR "cognitive cognitive stimulation") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Depression" OR "anxiety") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly")("Primary prevention") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly")("Cognitive training") AND ("Sleep quality") AND ("Cognitive impairment" OR "dementia") AND ("Cognitive training") AND ("Cognitive training") AND ("Sleep quality") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "dementia") AND ("Older adults" OR "elderly") ("Drug therapy" OR "medications") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Education" OR "education level") AND ("Cognitive impairment" OR "dementia") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") AND ("Lifestyle factors") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") AND ("Genetic factors") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly")
|
Table 1. Search equations |
|
|
Pubmed |
("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Quality of life" OR "well-being") AND ("Cognitive impairment" OR "dementia") ("Prevention" OR "intervention") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Risk factors" OR "predisposing factors") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") AND ("Family impact") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") AND ("Neuropsychological assessment") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") AND ("Social factors") AND ("Social factors") |
|
Science Direct, |
("Physical Exercise" OR "Physical Activity") AND ("Cognitive Impairment" OR "Dementia") AND ("Older Adults" OR "Elderly") AND ("Nutrition" OR "Diet") AND ("Cognitive Impairment" OR "Dementia") AND ("Older Adults" OR "Elderly") ("Cognitive Strategies" OR "Cognitive Stimulation") AND ("Cognitive Impairment" OR "Dementia") AND ("Older Adults" OR "Elderly") AND ("Cognitive Strategies" OR "Cognitive Stimulation") AND ("Cognitive Impairment" OR "Dementia") AND ("Older Adults" OR "Elderly") AND ("Cognitive Older adults" OR "elderly") ("Depression" OR "anxiety") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly")("Primary prevention") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly")("Cognitive training") |
|
Web of Science |
("Sleep quality") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Drug therapy" OR "medications") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Education" OR "educational level") AND ("Cognitive impairment" OR "dementia") AND ("Cognitive impairment" OR "dementia") AND ("Lifestyle factors") AND ("Cognitive impairment" OR "dementia") AND ("Cognitive cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") AND ("Lifestyle factors") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Genetic factors") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") |
|
Table 2. Cross-referencing of data terms |
||||||
|
Equation |
Databases |
Unfiltered |
No access |
Reviews/ incomplete/ duplicates |
Do not comply Criteria |
Selection |
|
("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Quality of life" OR well-being) |
Pubmed Science Direct Web of Science |
4345 |
3481 |
2813 |
1012 |
17 |
|
("Physical exercise" OR "physical activity") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") AND ("Nutrition" OR "diet") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") AND ("Nutrition" OR "diet") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") |
Pubmed Science Direct Web of Science |
2345 |
1278 |
923 |
624 |
11 |
|
("Quality of sleep") AND ("Cognitive impairment" OR "dementia") AND ("Older adults" OR "elderly") ("Drug therapy" OR "medications") AND ("Cognitive impairment" OR "dementia") |
Pubmed Science Direct Web of Science |
1367 |
923 |
532 |
247 |
8 |
|
Total |
|
8057 |
5682 |
4268 |
1883 |
36 |

Figure 1. Flowchart
In line with the results obtained, a word map developed in VOSviewer is presented below, which facilitates the visualization and organization of the information obtained from the results clearly and concisely. This facilitates the analysis of the data intuitively and strategically as shown below:
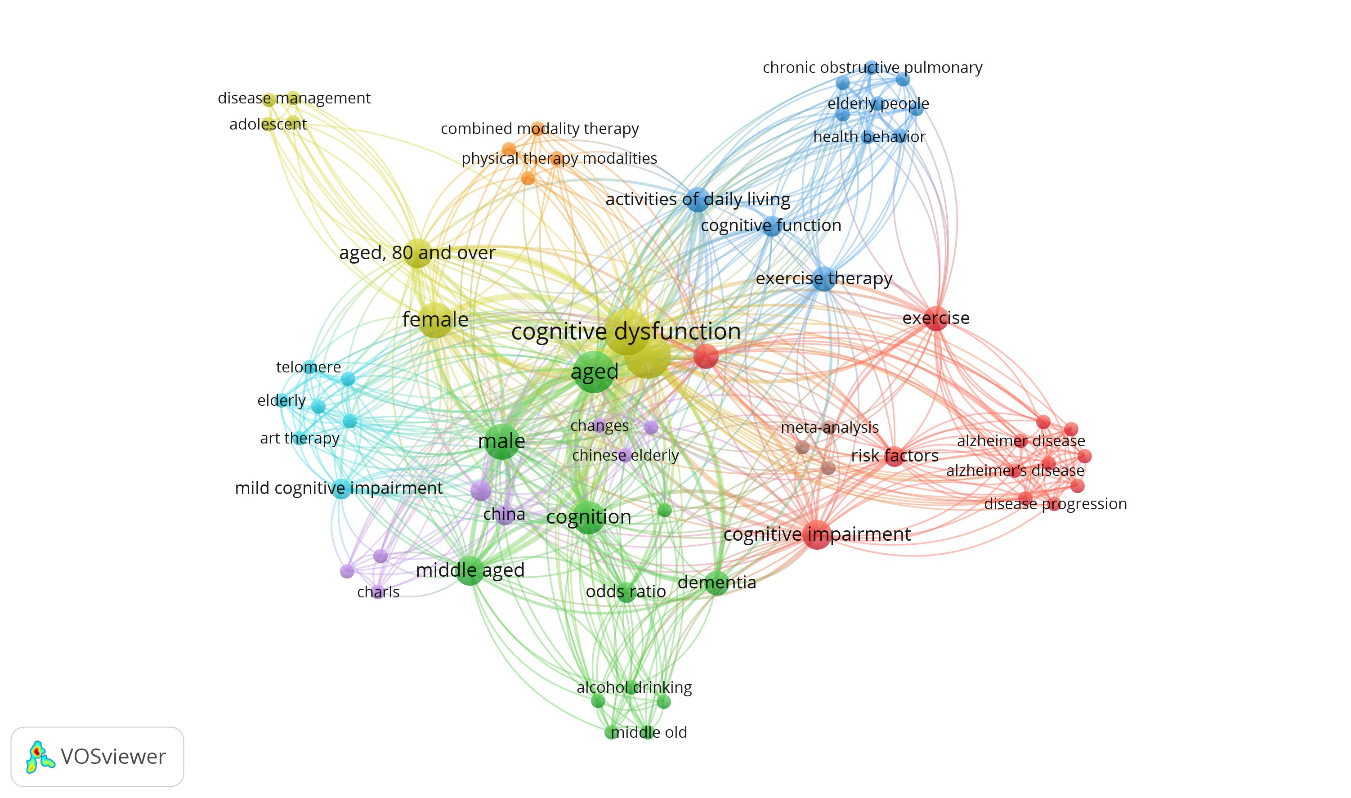
Figure 2. Word map
|
Table 3. Results |
||||||
|
N |
Variable crossings/Keywords |
Authors. year |
DOI |
Methodology |
Results found |
Country/city |
|
1
|
Mood disorders and comorbid conditions |
(13) (2021) (13) |
Quantitative with statistical approach. Data obtained using the Longitudinal Study of Aging in India (LASI) Wave 1 (2017-18). Cognitive impairment measured by modules from the Health and Retirement (HRS), and major depression measured by the CIDI-SF (Composite International Diagnostic Interview- Short. |
Older adults have a greater tendency to cognitive impairment and perceive their health as poor, manifesting difficulties in performing ADLs and a marked tendency to suffer from depression. |
Mumbai, Maharashtra, India |
|
|
2
|
Mood disorders and comorbid conditions |
(14) (2019) |
http://dx.doi.org/10.3390/ijerph16162877
|
Quantitative longitudinal, using the Chinese Longitudinal Healthy Longevity Survey (CLHLS). Cognitive function was measured using the adapted version of the Mini-Mental State Examination (MMSE). |
Loneliness was related to cognitive impairment, age, educational level, employment status, baseline cognitive function, marital status and disability for activities of daily living. |
China |
|
3
|
Lifestyle and Neuro cognition |
(15) (2019) |
Quantitative descriptive type. The Trail Making Test (TMT), Stroop test, forward and backward digit span subtest of the Wechsler scale were used for the evaluation of cognitive functions; Duke-Wake Forst graded maximal exercise test was used to measure physical and aerobic capacity.Duke-Wake Forst para medir la capacidad física y aeróbica. Los hábitos alimenticios se evaluaron mediante el Block Food Frequency Questionnaire. |
Eating habits were assessed using the Block Food Frequency Questionnaire. The results demonstrate that a 6-month aerobic exercise program significantly improved executive functioning in older adults with CVD risk factors. |
North Carolina, USA |
|
|
4
|
Lifestyle and Neuro cognition |
(16) (2020) (16) |
Quantitative Registry for Alzheimer 's Disease Assessment Packet (CERAD), an intervention of a total of 24 sessions of VR-based cognitive training is performed. Tests used: Mini-Mental Examination-Dementia screening test (MMSE-DS), the Trail Tracing Test (TMT) A and B, and the Symbol Digit Substitution Test (SDT). |
Intervention with VR games is one way to improve. Cognitive and frontal brain function in patients with MCI. There are no significant differences in parameters between the intervention and control groups at baseline |
Busan, South Korea |
|
|
5
|
Cognitive impairment and quality of life |
(17) (2019) |
Secondary analysis of data collected using the Resident Assessment Instrument for Home Care (RAI-HC). The RAI-HC |
20,5 % were classified with ISD, 8,5 % had a diagnosis of Alzheimer's disease, and 19,6 % had other types of dementia. The highest prevalence rates were found in adults over 80 years of age. |
Ontario, Canadá |
|
|
6
|
Mood disorders and comorbid conditions |
(18) (2019) |
Quantitative, an intervention is conducted to compare intervention outcomes with the effects of a health education control program for older adults with MCI. Single-blind RCT randomized controlled trial. Measurement tools such as the Geriatric Depression Scale (GDS) and (AFMV) for physical activity are used. |
Primary outcomes were changes in multiple domains of in multiple domains of cognitive function, identified by NCGG-FAT assessments. Secondary outcomes were post-intervention changes in grip strength, gait speed, and depressive symptoms. |
Tahoma, Aichi - Japan |
|
|
7
|
Lifestyle and Neuro cognition |
(19) (2019) |
Exploratory study. This study was a blinded randomized controlled trial. Subjects in the VR group participated in a 60-minute physical and cognitive workout three times a week for 12 weeks. Those in the CPC group participated in a combined physical and cognitive training of 60 minutes at each visit, three times per week for 12 weeks. |
Significant improvements in executive function (SCWT), single-task gait performance, and dual-task motor gait performance are present in both groups. However, only the VR group showed improvements in cognitive dual-task gait performance and cadence DTC after training. |
Taipei, Taiwan Tai |
|
|
8
|
Mood disorders and comorbid conditions |
(20) (2019) |
This is a single-center, randomized, double-blind, double-blind, 2-year, randomized controlled intervention trial. The UKU Side Effects Scale and cerebrospinal fluid sample collection were used; randomization to experimental (lithium) or comparison (placebo) groups was performed. |
Patients in the lithium group remained cognitively and functionally stable over 24 months, while patients in the placebo group showed mild but statistically significant cognitive and functional impairment. Lithium treatment was beneficial. |
São Paulo, Brazil |
|
|
9
|
Mood disorders and comorbid conditions |
(21) (2019) |
Quantitative Longitudinal cut-off.Data are collected annually from the Alzheimer's Disease Centers (ADC) in the United States. To perform a classification of apathy and depression using the Neuropsychiatric Questionnaire-Inventory-Questionnaire (NPI-Q), an AD diagnostic classification is performed. |
This analysis included 4 932 participants Mini-Mental State Examination. Of these participants, 8 % had only apathy, 31 % had only depression, 14 % had apathy and depression, and 48 % had no NPS. |
United States |
|
|
10
|
Lifestyle and Neuro cognition |
(22) (2019) |
Quantitative of explanatory scope. Two groups were divided for comparison: Exercise (EG, n=19) or control (CG, n=19). A full battery of neuropsychological tests of cognitive function was performed at baseline and after the 3-month intervention; MMSE instrument, MoCA Beijing version, WMS-R LM are used.. |
Between-group differences revealed that the 3-month WMS-R LM change in the GE was significantly greater than in the CG (P<0.05). The GE group demonstrated a significant increase in ALFF in bilateral frontotemporal, entorhinal, anterior cingulate, and parahippocampal cortex; whereas no significant differences were identified in the CG. |
Nanjing China |
|
|
11
|
Lifestyle and Neuro cognition |
(23) (2020) |
Quantitative Longitudinal The GEM study was originally designed as a randomized, controlled, double-blind trial, using the Clinical Dementia Rating (CDR) scale27, the Modified Mini-Mental State Mental Examination (3MSE)28 and the cognitive subscale of the Alzheimer's Disease Assessment Scale (ADAS-Cog)29 to assess cognitive function. |
Participants with DSI tended to be older, were more likely to be male and to have more comorbidities, smoke earlier and consume more alcohol.
|
United States |
|
|
12
|
Mood disorders and comorbid conditions |
(24) (2018) |
Quantitative longitudinal For this study, measures of visual function and cognition were assessed. The Mini-Mental State Examination (3MS) was used, current visual acuity was measured with a high-contrast Bailey-Lovie, contrast sensitivity was measured with a Pelli-Robson chart. |
Participants with impaired visual acuity, contrast sensitivity and stereo acuity had an increased risk of cognitive impairment. Poorer visual acuity and contrast sensitivity were also associated with an increased risk of incident cognitive impairment. |
United States |
|
|
13
|
Mood disorders and comorbid conditions |
(25) (2020) |
Qualitative with cross-sectional cohort analysis. A pragmatic intervention with patient/family components was performed. Patients' Attitudes Towards Deprescribing version is used for cognitive impairment. |
The study achieves optimal and appropriate medication use through cessation and dose reduction of inappropriate medications, focusing on safety and avoiding harm from chronic use. |
Colorado, USA |
|
|
14
|
Cognitive impairment and quality of life |
(26) (2021) |
The trial used a double-blind sham-controlled design with 3 intervention groups. tDCS sham (tDCS + CT sham group) or CT only (CT group). The Montreal Test of Cognitive Assessment (MoCA) was used. |
Significant main effects of time were found for all groups on MoCA after the intervention on everyday memory, especially in the tDCS + CT group. The tDCS + CT group.. |
Hong Kong. China |
|
|
15
|
Lifestyle and Neuro cognition |
(27) (2019) |
https://doi.org/10.1186/s13195-019-0480-5
|
Longitudinal study. A questionnaire of activities of daily living (IADL), National Center for Geriatrics and Gerontology-Functional Assessment Tool (NCGG-FAT) was used to measure cognitive functions. |
Participants were more likely to reverse if they began driving a car, reading books or newspapers, participated in cultural classes, attended community meetings, engaged in hobbies or sports, and did yard work or gardening. |
Japan |
|
16
|
Lifestyle and Neuro cognition |
(28) (2019) |
The Ascertain Dementia 8 (AD8) instrument is used to assess early memory loss, temporal orientation, judgment and function. It is classified into two models, model 1 estimated the main effects of marital status and model 2 added the interaction terms of status categories gender. |
The prevalence of dementia was higher among widowed, never married and divorced respondents than among married respondents. The prevalence of executive function and memory impairment was higher among the divorced and widowed than among the married. |
United States |
|
|
17
|
Cognitive impairment and quality of life |
(29) (2019)
|
Quantitative Participants' cognitive function was measured using the Chinese version of the MMSE along with characterization of sociodemographic factors. |
Cognitive ability was lower than in females, showing that the cognitive function of elderly women declined faster than in elderly males; cognitive scores were higher than in individuals aged 76 to 85 years and 64 to 75 years. |
China |
|
|
18
|
Cognitive impairment and quality of life |
(30) (2021) |
Survival analyses using multivariable Cox proportional hazards regression model and a Cox regression model with censored data were performed to assess the effect of hearing aid use on the risk of conversion from MCI to dementia. |
Participants with MCI who used hearing aids had a significantly lower risk of developing all-cause dementia compared with those who did not. No association was observed between hearing aid use and risk of death. |
Fujian, China |
|
|
19
|
Cognitive impairment and quality of life |
(31) (2021) |
Longitudinal study. The MoCA- which evaluates aspects of memory, executive function, attention, concentration, language, abstract reasoning and orientation; The Geriatric Depression Scale (GDS, abbreviated form) is used. It is applied to detect depressive symptoms. The Wechsler Adult Intelligence Scale, Third Edition WAIS III is also used. |
Scores on the MoCA-22 and the T-MoCA were significantly associated with education with education, race/ethnicity, depressive symptoms. |
Bronx County, New York |
|
|
20
|
Lifestyle and Neuro cognition |
(32) (2019) |
Multicenter longitudinal cohort study. Cognitive function was assessed using the Korean version of the Consortium to Establish Alzheimer (CERAD-K), Mini-Mental State Examination (MMSE-KC), CERAD battery to distinguish between normal patients and those with mild or moderate dementia. |
Sarcopenic individuals were more likely to have low physical function, consequently, sarcopenic individuals showed significantly lower MMSE scores and low cognitive test scores than non-sarcopenic individuals. |
Urban and rural regions, South Korea. |
|
|
21
|
Lifestyle and Neuro cognition |
(33) (2019) |
Cognitive function was assessed using a MMSE, Physical frailty was assessed using the modified version of Fried's criteria, and physical frailty was assessed using the modified version of Fried's criteria. |
Robust adults, both frail and pre-frail were older, had lower BMI, walked more slowly and performed worse in ADLs and IADLs. |
China |
|
|
22
|
Mood disorders and comorbid conditions |
(34) (2019) |
https://doi.org/10.14740/jocmr3894
|
Qualitative methodology using a cross-sectional study. The initial data collection was carried out by means of a sociodemographic and clinical interview, the IG (Graffar), MMSE; to evaluate anxiety and depression we used the psychological measure: Hospital Anxiety and Depression Scale (HADS) |
The results indicate that most of the patients were in the overweight and obese categories. According to the MMSE assessment, they were cognitively impaired. In relation to psychological variables, they had depression and anxiety, according to HADS scores |
Oporto, Portugal |
|
23
|
Mood disorders and comorbid conditions |
(35) (2019) |
The qualitative material was analyzed according to Mayring's summative content analysis approach. |
Participants noted that auditory, visual, and cognitive assessments were not appropriate for the complex needs of PWD and the complex sensory comorbidity of PWD. |
Breisgau, Germany |
|
|
24
|
Cognitive impairment and quality of life |
(36) (2018) |
Data from the HRS, a nationally representative cohort of US adults aged 50 years and older, were used. |
Physical frailty is a predictor of incidents of disability and death. because together physical frailty. CIND best identifies vulnerable older adults, risk assessment includes measures of cognitive function |
San Francisco California, United States. |
|
|
25
|
Mood disorders and comorbid conditions |
(37) (2022) |
Quantitative methodology with eognitive status interview 16-item questionnaire and questionnaire on cognitive impairment in older adults. |
Older adults with childhood adversity experience were more likely to be male, racial and ethnic minorities, and current smokers. They had lower educational attainment and wealth and a higher rate of elevated depressive symptoms and more chronic physical conditions. |
New York, Estados Unidos |
|
|
26
|
Cognitive impairment and quality of life |
(38) (2021) |
Cross-sectional analysis. Chinese versions of the MMSE and MoCA |
The overall prevalence of MCI was 28,6 % for the MMSE and 36,2 % for the MoCA. Both tools identify modifiable factors for mild cognitive impairment, which provide important evidence for establishing intervention measures |
Beijing, China |
|
|
27
|
Mood disorders and comorbid conditions |
(39) (2020) |
Randomized, double-blind, crossover, single-center pilot trial. Participants were randomly assigned to a modified Mediterranean-style ketogenic diet (MMKD), Beta diversity of the microbiome was assessed using the BrayCurtis dissimilarity index |
MCI patients have a significantly higher proportion of fungal families Sclerotiniaceae, Phaffomyceteceae, Trichocomaceae, Cystofilobasidiaceae, Togniniaceae and Botrytis genera, Kazachstania, Phaeoacremonium and Cladosporium while having lower proportions of the family Cladosporiaceae and the genus Meyerozyma. |
Winston-Salem, North Carolina |
|
|
28
|
Lifestyle and Neuro cognition |
(40) (2020) |
Quantitative. We used the Mini-Mental State Examination (MMSE) in Runnymede, the Montreal Cognitive Assessment (MoCA) in Baycrest, and the in Baycrest, and the Cognitive Performance Scale (CPS) in Kensington. Kensington |
Participants interacted with the virtual environment by moving and looking around during the exposure despite their physical impairments. The intervention was well tolerated by people with various sensory, cognitive, and physical limitations. |
Toronto, Canadá |
|
|
29
|
Mood disorders and comorbid conditions |
(41) (2019) |
Clinical trials. Stool sample Lumbar puncture, CSF biomarker assays and ApoE ε-4 genotyping. |
The results suggest that certain bacterial groups show ICM-specific Profile and, therefore, can be used as additional and corroborative biomarkers for ICM detection. |
Winston-Salem, USA |
|
|
30
|
Cognitive impairment and quality of life |
(29) (2019) |
Cognitive evaluations were performed by neuropsychologists according to standardized methods, including the MMSE and the Alzheimer's Disease standardized methods, including the MMSE and the Alzheimer's Disease Rating Scale. |
The combined 24-week intervention improved cognitive function and physical function in MCI patients relative to controls. Encouraging participants to perform an additional 10 minutes of supervised moderate physical activity during the ongoing intervention may be more beneficial in preventing cognitive decline. |
Busan, Korea |
|
|
31
|
Lifestyle and Neuro cognition |
(42) (2019)
|
Electronic databases were searched to identify studies using an experimental design to investigate the outcomes of VR intervention in patients with MCI or dementia. |
Virtual reality interventions, particularly those of a semi-immersive type, are useful for people with mild cognitive impairment or dementia. These results should contribute to the establishment of practical guidelines for virtual reality interventions for patients with cognitive impairment. |
Seoul, South Korea. |
|
|
32
|
Mood disorders and comorbid conditions |
(43) (2020) |
Combined cognitive classification model and EEG (using the Mini-Mental State Examination; MMSE). |
SMRI outperformed resting-state EEG, However, both EEG and sMRI were only moderately good at distinguishing aMCI from healthy aging and neither method achieved a sensitivity greater than 70 %. |
Dublin, Ireland.. |
|
|
33
|
Lifestyle and Neuro cognition |
(44) (2018) |
Blinded randomized controlled trial (blind to the investigator, but not to the subject) Physical exercise, Combined physical exercise and cognitive training intervention. |
Cognitive performance on all four tasks in the combined training group improved significantly after the intervention. Changes in cognitive performance were greater in the combined intervention group than in the physical exercise group. |
Shanghai, China. |
|
|
34
|
Cognitive impairment and quality of life |
(45) (2020) |
Qualitative through critical overview of the literature regarding the emerging trajectories and correlates of cognitive functioning in Bipolar Disorder. |
The evidence regarding the progressive nature of cognitive impairment is contradictory, as there is no consensus among the different cross-sectional data and is inconsistent with the results of the limited longitudinal studies available. |
Australia |
|
|
35 |
Cognitive impairment and quality of life |
(46) (2020) |
The Cache County Study on Memory in Aging. Neuropsychiatric Inventory (NPI). |
Basal NPI total score was associated with a faster rate of decline in word list memory, praxis recall, and animal fluency. Likewise increased baseline anxiety was associated with impairment in symbolic digit modality. |
Baltimore United States. |
|
Analysis of variables
Cognitive impairment and quality of life: cognitive impairment in older adults is a topic of relevance in the area of neuroscience and psychology because neural processes involve changes that are reflected in cognitive functions, including aspects related to memory, attention, and abstract thinking; changes that demand attention from specialized health professionals,(29) cognitive changes with age are expected within the aging process and evolutionary course of the human being.(44) It is worth mentioning that many older adults maintain and preserve a high level of cognitive functioning; however, from the opposite perspective, many of them may suffer a significant cognitive deterioration generating a condition of greater affectation, such as dementia, and with it, the elements of daily life are significantly affected, causing a detriment and impact that requires early intervention when necessary.(47)
It is worth mentioning that in this variable, according to the findings identified in the analysis matrix, it was evidenced that cognitive impairment in older adults, presents different precipitating and risk factors, which include on the one hand, genetic and environmental factors, such as lifestyle, including physical activity, healthy diet, mental health promotion strategies and generation of socialization spaces, which are controlled by the patient, under the clinical guidance of mental health professionals.(30) In this sense, the application of intervention strategies mainly uses cognitive-behavioral therapies, as well as neurostimulation exercises that are aimed at reducing clinically significant distress, with the objective of preserving the patient's autonomy, and thus improving quality of life indicators.(26)
Lifestyle and neurocognition: quality of life in late adulthood is measured by multiple factors that directly intervene in the relationship between lifestyle and neurocognition. Taking into account that scientific advances have shown that the adoption of healthy lifestyles tends to have a significant impact on the older adult population.(48) A relevant aspect of healthy cognitive function is the performance of physical activities, which, in the first place, help to improve mental health conditions, which are linked to an optimization of attention and memory and which, in turn, denotes the greater speed of cognitive processing, thus implying that the brain is active and protected against cognitive impairment.(19)
Another fundamental element in the protection of cognitive impairment is adequate nutrition, which establishes a balance in maintaining a healthy brain in the aging process.(49) Health professionals and especially psychologists indicate the importance of maintaining a balanced diet with essential nutrients, antioxidants, and healthy fats that help prevent dementia-related aspects in older adults. On the other hand, it is essential to maintain brain activity through stimulation, making cognitive acuity a challenge within which reading, development of games, crossword puzzles, word search, and other recreational activities that involve brain work that requires cognitive training, which leads to improved quality of life.(15)
Mood disorders and comorbid pathologies: The most common mood disorders in older adults are related to depression and anxiety, which generate a significant impact on comorbidity as coexisting pathologies within neurocognition because these reflect highly complex alterations that represent clinically significant compromises in the states of psychological well-being of older adults.(50) According to the reports of the research advances it has been shown that with depression at this age,(36) there is an increased risk of cognitive impairment and dementia, which is demonstrated with the fulfillment of diagnostic criteria related to decreased energy, lack of motivation, cognitive impairments including concentration and memory problems, leading to changes within the nervous system.(48)
It is important to note that excessive concern about mental health indicates that the higher the level of anxiety symptoms, the greater the negative impact on cognitive functioning and detriment to quality of life.(15) Psychological interventions are needed to improve the mental health and general functioning of older adults, as they may have chronic diseases and associated comorbidities, which have a significant impact on mood. This generates that neurocognition is intrinsically linked to interrelational conditions that imply an improvement in the quality of life, which leads to an increase in the emotional and cognitive levels of older adults.(51)
DISCUSSION
The impact of quality of life on the cognitive functioning of older adults is associated with genetic and environmental factors,(36) which are identified as a mental health problem that, to a large part of the population, due to risk factors such as the presence of chronic diseases, alcohol consumption, physical inactivity, inadequate emotional management, determine to a large extent, a multifactorial context that requires interventions and strategies that promote healthy habits focused on healthy aging and with greater skills to adapt to the new stage. In this same sense,(35) indicate that The understanding of this clinical condition requires studies with traceability that allow analyzing the progression of the disease, so that, other factors associated with the environment can be identified, which promote quality of life and psychological well-being.(52)
On the other hand, indicate that another relevant factor within the research process is directly related to coping with loneliness and its link with mood alterations that have a great impact on the most frequent pathologies in older adults such as depression and anxiety, in which the intervention with physical exercise and cognitive stimulation had a greater impact.(53) Regarding risk factors, it can be evidenced that poor eating habits have a great impact on the elderly, predisposing them not only to physical risk but also to a passive role in aging in terms of cognitive development.(39)
State that the relationship between mood and quality of life in older adults hurts the health and well-being of the population studied.(37) Aging requires an in-depth study that relates the effects on daily life, and the impact on the family system and society, since the related problems affect the autonomy and independence of those who suffer from these cognitive alterations. Observed that it is limiting for individuals to carry out daily activities, fluctuation in social relationships, the ability to make decisions, and psychosocial alterations that generate an effect on the manifestation of clinical symptoms associated with mental problems such as; anxious pictures, stressful situations, family affectations, and decreased self-esteem, among others.(27)
Indicate the prevalence of risk factors that affect the loss of cognitive abilities,(17) due to the experimentation of psychological alterations that require a growth of scientific contributions related to the promotion of neuroplasticity, the increase of physical activity, neurocognitive stimulation exercises that should be linked to a balanced diet, rich in nutrients and vitamins that allow increasing the conditions of well-being through an exploration and interventive development directed towards the understanding of the underlying mechanisms, this being a priority aspect that leads to a greater assimilation of the subject matter addressed.(13)
Stated that brain aging was identified as a gradual and evolutionary process in the order of development,(26) which can affect brain health and function due to the components that influence adverse factors that cause cognitive detriment in old age. The challenges of intervention are focused on relating lifestyle conditions and aging because contributions from different disciplines converge in the promotion of a healthy lifestyle that allows preserving brain health in old age. This generates significant opportunities that increase the conditions of well-being that lead to successful aging.(15)
The challenges posed by scientific advances in cognitive impairment in older adults involve the emergence of serious neurodegenerative disorders such as Alzheimer's disease and other types of dementia, which affect the functionality of older adults including a negative emotional impact that results in anxiety and depression mainly.(31) The challenges faced by health professionals especially psychologists, lead to early detection that allows managing the emotional distress of patients through processes of interventions and person-centered strategies with an occupational approach; which facilitates the implementation of non-pharmacological therapies, if not focused on preventive aspects and improvement of lifestyles, through a personalized treatment for the patient and his family.(54)
CONCLUSIONS
Cognitive impairment is a mental pathology that generates a significant concern in the population of older adults, due to the demographic and sociocultural contexts, presenting a high incidence of occurrence of symptoms associated with pathological comorbidities, especially those related to depressive and anxiety disorders.(18) The duality of pathologies generates a great impact on the condition of cognitive impairment because, the intensification of symptoms can cause an acceleration in the loss of neurocognitive functions, exacerbating memory dysfunction and progressing to dementia or Alzheimer's disease. The impairment of autonomy and independence, and the detriment of family relationships generate a negative impact on the quality of life of older adults.(6)
Early detection of cognitive impairment is essential to provide adequate care that allows an effective patient-centered intervention with a cognitive-behavioral approach that reduces the symptoms of impairment and generates a comprehensive interdisciplinary care approach by health professionals, thus ensuring adequate support and emotional support that helps to understand the symptomatic manifestation of the disease and the sequelae that result from it. The identification of modifiable factors in the subjects, such as the brain stimulation technique, nutritional diet, and physical activity, is beneficial in the intervention process for the patient, his family, and support network.(47)
The emotional burden raised in patients with cognitive impairment generates a significant impact on patients because clinical conditions related to anxiety and stress that lead to the onset of depression may appear. This is why cognitive therapies with brain stimulation can help improve cognitive functions and quality of life in older adults.(46) A fundamental aspect is the proportion of well-being generated by caregivers who help to slow down in some cases the deterioration and health conditions, which is why it is necessary that the care process is provided in a multidisciplinary manner since the contributions of each discipline will allow offering the necessary support in the interventional process of the disease.
REFERENCES
1. Cardona-Arango D, Segura-Cardona A, Garzón-Duque M, Segura-Cardona A, Cano-Sierra S. Estado de salud mental del adulto mayor de Antioquia, Colombia. Rev Bras Geriatr e Gerontol [Internet]. 2016;19:71–86. Available from: http://www.scielo.br/pdf/rbgg/v19n1/es_1809-9823-rbgg-19-01-00071.pdf
2. Rojas-Zepeda C, López-Espinoza M, Cabezas-Araneda B, Castillo-Fuentes J, Márquez-Prado M, Toro-Pedreros S, et al. Factores de riesgo sociodemográficos mórbidos asociados a deterioro cognitivo leve en adultos amyores. Cuad Neuropsicol. 2021;15:43–56.
3. Parada-Muñoz K, Guapizaca-Juca J, Bueno-Pacheco G. Deterioro cognitivo y depresión en adultos mayores : una revisión sistemática de los últimos 5 años. Uisrael Rev científica. 2022;77–93.
4. Patnode C, Perdue L, Rossom R, Rushkin M, Redmond N, Thomas R, et al. Screening for Cognitive Impairment in Older Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA - J Am Med Assoc. 2020;323(8):764–85.
5. Suárez L, Gross R. Estimulación cognitiva y apoyo familiar hacia adulto mayor con deterioro cognitivo. Rev Inf Científica [Internet]. 2019;98(1):88–97. Available from: http://scielo.sld.cu/pdf/ric/v98n1/1028-9933-ric-98-01-88.pdf
6. Farhang M, Miranda-Castillo C, Rubio M, Furtado G. Impact of mind-body interventions in older adults with mild cognitive impairment: A systematic review. Int Psychogeriatrics. 2019;31(5):643–66.
7. Figueroa-Varela M, Aguirre-Ojeda D, Hernández-Pacheco R. Asociación del deterioro cognitivo, depresión, redes sociales de apoyo, miedo y ansiedad a la muerte en adultos mayores. Psicumex. 2021;11:1–29.
8. Bravo-Toledo R. La declaración PRISMA 2020: una guía actualizada para la publicación de revisiones sistemáticas. PLoS Med. 2021;1–15.
9. Urrútia G, Bonfill X. Declaración PRISMA: una propuesta para mejorar la publicaicón de resiviones sistemáticas y metaanálisis. In: Medicina Clínica. 2010. p. 507–11.
10. Barrios-Serna K, Orozco-Núñez D, Pérez-Navas E, Conde-Cardona G. Nuevas recomendaciones de la versión PRISMA 2020 para revisiones sistemáticas y metaanálisis. Acta Neurológica Colomb. 2021;37(2):105–6.
11. Page P, Simpson A, Reynolds L. Bearing witness and being bounded: The experiences of nurses in adult critical care in relation to the survivorship needs of patients and families. J Clin Nurs. 2019;28(17–18):3210–21.
12. Haddaway NR, Page MJ, Pritchard CC, Mcguinness LA. PRISMA2020 : An R package and Shiny app for producing PRISMA 2020 ‐ compliant flow diagrams , with interactivity for optimised digital transparency and Open Synthesis. Campbell Wiley. 2022;1–12.
13. Muhammad T, Meher T. Association of late-life depression with cognitive impairment: evidence from a cross-sectional study among older adults in India. BMC Geriatr. 2021;21(1):1–13.
14. Zhou Z, Mao F, Zhang W, Towne SD, Wang P, Fang Y. The association between loneliness and cognitive impairment among older men and women in China: A nationwide longitudinal study. Int J Environ Res Public Health. 2019;16(16).
15. Hernández-Flórez N. Breaking stereotypes: “a philosophical reflection on women criminals from a gender perspective". AG Salud 2023;1:17-17.
16. Quiroz FJR, Oncoy AWE. Resiliencia y satisfacción con la vida en universitarios migrantes residentes en Lima. AG Salud 2023;1:09-09.
17. Blumenthal JA, Smith PJ, Mabe S, Hinderliter A, Lin PH, Liao L, et al. Lifestyle and neurocognition in older adults with cognitive impairments: A randomized trial. Neurology. 2019;92(3):E212–23.
18. Thapa N, Park HJ, Yang JG, Son H, Jang M, Lee J, et al. The effect of a virtual reality-based intervention program on cognition in older adults with mild cognitive impairment: A randomized control trial. J Clin Med. 2020;9(5).
19. Davidson JGS, Guthrie DM. Older adults with a combination of vision and hearing impairment experience higher rates of cognitive impairment, functional dependence, and worse outcomes across a Set of quality indicators. J Aging Health. 2019;31(1):85–108.
20. Bae S, Lee S, Lee S, Jung S, Makino K, Harada K, et al. The effect of a multicomponent intervention to promote community activity on cognitive function in older adults with mild cognitive impairment: A randomized controlled trial. Complement Ther Med [Internet]. 2019;42:164–9. Available from: https://doi.org/10.1016/j.ctim.2018.11.011
21. Liao Y, Chen H, Lin Y, Chen Y, Hsu W. Effects of virtual reality-based physical and cognitive training on executive function and dual-task gait performance in older adults with mild cognitive impairment: A randomized control trial. Front Aging Neurosci. 2019;10(JUL):1–10.
22. Forlenza O V., Radanovic M, Talib LL, Gattaz WF. Clinical and biological effects of long-term lithium treatment in older adults with amnestic mild cognitive impairment: Randomised clinical trial. Br J Psychiatry. 2019;215(5):668–74.
23. Quinn C, Nelis SM, Martyr A, Victor C, Morris RG, Clare L. Influence of positive and negative dimensions of dementia caregiving on caregiver well-being and satisfaction with life: findings from the ideal study. Am J Geriatr Psychiatry [Internet]. 2019;27(8):838–48. Available from: https://doi.org/10.1016/j.jagp.2019.02.005
24. Auza-Santivañez JC, Lopez-Quispe AG, Carías A, Huanca BA, Remón AS, Condo-Gutierrez AR, et al. Improvements in functionality and quality of life after aquatic therapy in stroke survivors. AG Salud 2023;1:15-15.
25. Castillo-González W. Kinesthetic treatment on stiffness, quality of life and functional independence in patients with rheumatoid arthritis. AG Salud 2023;1:20-20.
26. Qi M, Zhu YI, Zhang L, Wu T, Wang JIE. The effect of aerobic dance intervention on brain spontaneous activity in older adults with mild cognitive impairment : A resting ‑ state functional MRI study. Exp Ther Med. 2019;715–22.
27. Hwang PH, Longstreth WT, Brenowitz WD, Thielke SM, Lopez OL, Francis CE, et al. Dual sensory impairment in older adults and risk of dementia from the GEM Study. Diagnosis, Assess Dis Monit. 2020;12(1):1–9.
28. Swenor B, Wang J, Varadaraj V, Rosano C, Yaffe K, Albert M, et al. Vision Impairment and Cognitive Outcomes in Older Adults: The Health ABC Study Bonnielin. Oxford Univ Press. 2018;(January):2010–7.
29. Bayliss E, Bayliss E, Shetterly S, Drace M, Norton J, Green A, et al. The optimize patient- And family-centered, primary care-based deprescribing intervention for older adults with dementia or mild cognitive impairment and multiple chronic conditions: Study protocol for a pragmatic cluster randomized controlled trial. Trials. 2020;21(1):1–13.
30. Cruz-González P, Fong K, Brown T. Transcranial direct current stimulation as an adjunct to cognitive training for older adults with mild cognitive impairment: A randomized controlled trial. Ann Phys Rehabil Med [Internet]. 2021;64(5):101536. Available from: https://doi.org/10.1016/j.rehab.2021.101536
31. Shimada H, Doi T, Lee S, Makizako H. Reversible predictors of reversion from mild cognitive impairment to normal cognition : a 4-year longitudinal study. Alzheimers Res Ther. 2019;5:1–9.
32. Liu H, Zhang Y, Burgard S, Needham B. Marital status and cognitive impairment in the United States: evidence from the National Health and Aging Trends Study. Ann Epidemiol [Internet]. 2019;38:28-34.e2. Available from: https://doi.org/10.1016/j.annepidem.2019.08.007
33. Zhang Q, Wu Y, Han T, Liu E. Changes in Cognitive Function and Risk Factors for Cognitive Impairment of the Elderly in China : 2005 – 2014. Int jorunal Environmetal Res public Heal. 2019;16.
34. Bucholc M, Ding X, Mcclean P, Ye Q, Bauermeister S, Todd S, et al. Association of the use of hearing aids with the conversion from mild cognitive impairment to dementia and progression of dementia : A longitudinal retrospective study. Transl Res Clin Interv. 2021;(February):1–11.
35. Katz MJ, Wang C, Nester CO, Derby CA, Rabin LA, Zimmerman ME, et al. T-MoCA : A valid phone screen for cognitive impairment in diverse community samples. Diagnosis, Assess Dis Monit. 2021;1–11.
36. Li Y, Akkus C, Yu X, Joyner A, Kmet J, Sweat D, et al. Heatwave events and mortality outcomes in memphis, tennessee: Testing effect modification by socioeconomic status and urbanicity. Int J Environ Res Public Health. 2019;16(22):1–14.
37. Ma L, Zhang L, Sun F, Li Y, Tang Z. Cognitive function in Prefrail and frail community-dwelling older adults in China. BMC Geriatr. 2019;19(1):1–7.
38. Mendes R, Martins S, Fernandes L. Adherence to Medication , Physical Activity and Diet in Older Adults With Diabetes : Its Association With Cognition , Anxiety and Depression. Clin Med Res Elmer Press IncTM. 2019;11(8):583–92.
39. Wolski L, Leroi I, Regan J, Dawes P, Charalambous AP, Thodi C, et al. The need for improved cognitive , hearing and vision assessments for older people with cognitive impairment : a qualitative study. BMC Geriatr. 2019;19:1–12.
40. Aliberti MJR, Cenzer IS, Smith AK, Lee SJ, Yaffe K, Covinsky KE. Assessing Risk for Adverse Outcomes in Older Adults : The Need to Include Both Physical Frailty and Cognition. J Am Geriatr Soc. 2018;3:1–7.
41. Xiang X, Cho J, Sun Y. Childhood adversity and cognitive impairment in later life. Front Psychol. 2022;1–12.
42. Jia X, Wang Z, Huang F, Su C, Du W, Jiang H, et al. A comparison of the Mini-Mental State Examination (MMSE) with the Montreal Cognitive Assessment (MoCA) for mild cognitive impairment screening in Chinese middle-aged and older population: a cross-sectional study. BMC Psychiatry. 2021;21(1):1–13.
43. Nagpal R, Neth B, Wang S, Mishra S, Craft S, Yadav H. Gut mycobiome and its interaction with diet, gut bacteria and alzheimer’s disease markers in subjects with mild cognitive impairment: A pilot study. EBioMedicine [Internet]. 2020;59:102950. Available from: https://doi.org/10.1016/j.ebiom.2020.102950
44. Appel L, Appel E, Bogler O, Wiseman M, Cohen L, Ein N, et al. Older Adults With Cognitive and/or Physical Impairments Can Benefit From Immersive Virtual Reality Experiences: A Feasibility Study. Front Med. 2020;6(January).
45. Nagpal R, Neth BJ, Wang S, Craft S, Yadav H. Modified Mediterranean-ketogenic diet modulates gut microbiome and short-chain fatty acids in association with Alzheimer’s disease markers in subjects with mild cognitive impairment. EBioMedicine [Internet]. 2019;47:529–42. Available from: https://doi.org/10.1016/j.ebiom.2019.08.032
46. Kim O, Pang Y, Kim J. The effectiveness of virtual reality for people with mild cognitive impairment or dementia : a meta-analysis. BMC Psychiatry. 2019;19:1–10.
47. Farina F, Emek-Savaş D, Rueda-Delgado L, Boyle R, Kiiski H, Yener G, et al. A comparison of resting state EEG and structural MRI for classifying Alzheimer’s disease and mild cognitive impairment. Neuroimage. 2020;215(April).
48. Bo W, Lei M, Tao S, Jie LT, Qian L, Lin FQ, et al. Effects of combined intervention of physical exercise and cognitive training on cognitive function in stroke survivors with vascular cognitive impairment : a randomized controlled trial. Clin Rehabil. 2018;1–10.
49. Van-Rheenen T, Lewandowski K, Bauer I, Kapczinski F, Miskowiak K, Burdick KE, et al. Current understandings of the trajectory and emerging correlates of cognitive impairment in bipolar disorder: An overview of evidence. Bipolar Disord. 2020;22(1):13–27.
50. Burhanullah MH, Tschanz J, Peters M, Leoutsakos J, Matyi J, Lyketsos C, et al. Neuropsychiatric Symptoms as Risk Factors for Cognitive Decline in Clinically Normal Older Adults: The Cache County Study. Am J Geriatr Psychiatry [Internet]. 2020;28(1):64–71. Available from: https://doi.org/10.1016/j.jagp.2019.03.023
51. Golomb J, Kluger A, Ferris SH. Mild cognitive impairment: Historical development and summary of research. Dialogues Clin Neurosci. 2022;6(4):351–67.
52. Guarino A, Forte G, Giovannoli J, Casagrande M. Executive functions in the elderly with mild cognitive impairment: a systematic review on motor and cognitive inhibition, conflict control and cognitive flexibility. Aging Ment Heal [Internet]. 2020;24(7):1028–45. Available from: https://doi.org/10.1080/13607863.2019.1584785
53. Schikowski T, Altuğ H. The role of air pollution in cognitive impairment and decline. Neurochem Int [Internet]. 2020;136(November 2019):104708. Available from: https://doi.org/10.1016/j.neuint.2020.104708
54. Naef N, Schlosser L, Brugger P, Greutmann M, Oxenius A, Wehrle F, et al. Brain volumes in adults with congenital heart disease correlate with executive function abilities. Brain Imaging Behav. 2021;15(5):2308–16.
55. Drew DA, Weiner DE, Sarnak MJ. Cognitive Impairment in CKD: Pathophysiology, Management, and Prevention. Am J Kidney Dis [Internet]. 2019;74(6):782–90. Available from: https://doi.org/10.1053/j.ajkd.2019.05.017
56. Gutíérrez Cobo M, Cabello R, Fernández Berrocal P. Inteligencia emocional, control cognitivo y el estatus socioeconómico de los padres como factores protectores de la conducta agresiva en la niñez y la adolescencia. Intel Emoc Control Cogn y estatus socioeconómico los padres como factores Prot la Conduct agresiva en la niñez y la Adolesc. 2017;31(88):39–52.
57. Kosonogov V, Vorobyeva E, Kovsh E, Pavel E. A review of neurophysiological and genetic correlates of emotional intelligence. Int J Cogn Res Sci Eng Educ. 2019;7(1):137–42.
58. Strzelczyk A, Schubert-Bast S. Psychobehavioural and Cognitive Adverse Events of Anti-Seizure Medications for the Treatment of Developmental and Epileptic Encephalopathies [Internet]. Vol. 36, CNS Drugs. Springer International Publishing; 2022. 1079–1111 p. Available from: https://doi.org/10.1007/s40263-022-00955-9
FINANCING
The research was carried out with the researchers' own resources.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Elisama Beltrán de la Rosa; Francis Araque-Barboza.
Data curation: Johana Vásquez-Torres; María José Orozco Santander.
Formal analysis: Nubia Hernández-Flórez; Olena Klimenko.
Acquisition of funds: Francis Araque-Barboza.
Research: Elisama Beltrán de la Rosa; María José Orozco Santander.
Methodology: Nubia Hernández-Flórez; Olena Klimenko.
Project management: Nubia Hernández-Flórez; Olena Klimenko.
Resources: Francis Araque-Barboza; Johana Vásquez-Torres; María José Orozco Santander.
Software: Nubia Hernández-Flórez; Olena Klimenko.
Supervision: Nubia Hernández-Flórez; Olena Klimenko.
Validation: Nubia Hernández-Flórez; Olena Klimenko.
Display: Elisama Beltrán de la Rosa; María José Orozco Santander.
Drafting - original draft: Nubia Hernández-Flórez; Olena Klimenko.
Writing - proofreading and editing: Nubia Hernández-Flórez; Olena Klimenko.