doi: 10.56294/saludcyt2024.574
ORIGINAL
Effect of changes in the centre of rotation after hip arthroplasty on knee joint function
Efecto de los cambios en el centro de rotación tras una artroplastia de cadera sobre la función de la articulación de la rodilla
Oleksandr Zubkov1
![]() *, Victor Torchynskyi1
*, Victor Torchynskyi1
![]() *
*
1Clinic of Orthopedics and Traumatology for Adults, Institute of Traumatology and Orthopedics of the National Academy of Medical Sciences of Ukraine. Kyiv, Ukraine.
Cite as: Zubkov O, Torchynskyi V. Effect of changes in the centre of rotation after hip arthroplasty on knee joint function. Salud, Ciencia y Tecnología. 2024; 4:.574. https://doi.org/10.56294/saludcyt2024.574
Submitted: 12-02-2024 Revised: 24-05-2024 Accepted: 17-09-2024 Published: 18-09-2024
Editor: Dr.
William Castillo-González ![]()
Corresponding author: Oleksandr Zubkov *
ABSTRACT
Introduction: a common complication after hip arthroplasty is pain and inflammation in other large joints, especially the knee joint. Displacement of the centre of rotation of the femoral head after endoprosthetics can change the redistribution of force vectors acting on the femur, change its tilt and pressure on the surface of the knee joint.
Objective: the investigation of the effect of displacement of the centre of rotation of the hip joint after arthroplasty on the knee joint.
Methods: using SolidWorks software and the SimulationXpress tool, a 3D model of the lower limb was created that reproduced the interaction between the components of the musculoskeletal system.
Results: as a result, it was found that the displacement of the centre of rotation of the hip joint medially and laterally from the anatomical position leads to a significant increase in pressure on the corresponding tibial condyles. The increase in load is linear and increases from a minimum value of 1,77 N⋅m in anatomical position to 123,79 N⋅m with a medial displacement of up to 8 mm.
Conclusions: this study indicates the need for proper restoration of the centre of rotation of the hip joint after implantation and the possible consequences of changes in knee joint loads. The data may be useful for specialists working in the field of implantology and the development of hip prosthesis systems.
Keywords: Osteoarthritis; Tibial plateau; Prosthesis; Load.
RESUMEN
Introducción: una complicación frecuente tras la artroplastia de cadera es el dolor y la inflamación en otras articulaciones grandes, especialmente la articulación de la rodilla. El desplazamiento del centro de rotación de la cabeza femoral tras la endoprótesis puede modificar la redistribución de los vectores de fuerza que actúan sobre el fémur, cambiar su inclinación y ejercer presión sobre la superficie de la articulación de la rodilla.
Objetivo: investigar el efecto del desplazamiento del centro de rotación de la articulación de la cadera tras la artroplastia sobre la articulación de la rodilla.
Métodos: utilizando el software SolidWorks y la herramienta SimulationXpress, se creó un modelo 3D de la extremidad inferior que reproducía la interacción entre los componentes del sistema musculoesquelético.
Resultados: como resultado, se observó que el desplazamiento del centro de rotación de la articulación de la cadera medial y lateralmente con respecto a la posición anatómica provoca un aumento significativo de lapresión sobre los cóndilos tibiales correspondientes. El aumento de la carga es lineal y aumenta desde un valor mínimo de 1,77 N⋅m en posición anatómica hasta 123,79 N⋅m con un desplazamiento medial de hasta 8 mm.
Conclusiones: este estudio indica la necesidad de restablecer adecuadamente el centro de rotación de la articulación de la cadera tras la implantación y las posibles consecuencias de los cambios en las cargas de la articulación de la rodilla. Los datos pueden ser útiles para los especialistas que trabajan en el campo de la implantología y el desarrollo de sistemas de prótesis de cadera.
Palabras clave: Osteoartritis; Meseta tibial; Prótesis; Carga.
INTRODUCTION
Hip arthroplasty is a common and successful surgical procedure designed to restore limb function and improve the quality of life for patients suffering from osteoarthritis and other degenerative hip joint diseases.(1) About one million hip arthroplasty operations are performed annually worldwide, with 95 % of implants surviving 10 years and 80 % – 25 years.(2) In Ukraine, about 25 thousand patients require hip arthroplasty every year, but only 7-10 thousand receive assistance per year. Modern methods of hip arthroplasty include cement-free implant technology, minimally invasive surgical methods, computer navigation, and more modern and safe materials.(3)
Negative changes in large joints, especially knee joints, are common, so modelling considering mechanical changes can reduce extraneous effects. The optimal position of endoprosthesis components, particularly the center of rotation, is crucial for hip arthroplasty. An incorrect position of the prosthetic head may result in dislocation of the hip.(4) The cause of endoprosthetics is often severe dysplasia and other significant defects of the hip cavity, in which it is difficult to install the acetabular component of the prosthesis in an anatomical position, and degenerative and inflammatory diseases that change the shape of the joint surfaces.(5) Therefore, restoring the anatomical centre of rotation is often problematic.(6)
Studies show that about 50 % of patients have a displacement of the hip rotation center within a few millimeters, making it important to predict how significant this displacement is and how it changes the redistribution of forces acting in the limb joint system.(7-9) The correct location of the rotation center affects the biomechanical conditions of functioning not only of the hip but also of other joints of the lower limb, particularly the knee.(10,11)
There is a need for a detailed study of the effect of changes in the center of rotation on the axis of the lower limb and the knee joint after hip arthroplasty. Among the modern methods that significantly expand the possibilities of prosthetics, modern methods of mathematical and 3D modelling should be distinguished, which allow predicting the results of the intervention.(12,13)
This study’s purpose is to examine the impact of femoral head rotation changes on knee joint load after hip arthroplasty and to develop a mathematical model to determine load changes at different hip joint displacements. This research is crucial for orthopedic doctors to determine optimal prosthesis positions, predict complications, and select the best rehabilitation strategy.
METHODS
A mathematical model and 3D simulation model of the lower limb were created using Solidworks software suite, which included an arthroplasty of hip, femur, tibia, and tibial plateau cartilage, to analyze the impact of rotation center changes on knee joint. The load on the hip arthroplasty (on the centre of rotation) was the body weight acting on the lower limb, respectively shifting the centre of rotation 2, 4, 6, and 8 mm medially and laterally from the starting position. The patient’s knee joint load was determined using solid body mechanics equations and anatomical features of the hip and knee joints while standing with uniform body weight distribution.
Mathematical model. The hypothetical weight of the patient included in the model was 90 kg. The force acting vertically down through the centre of rotation was calculated using equation Ftotal=m * g (1), where: Ftotal is the force acting on the knee joint from the weight of the body; m – patient’s mass; g – gravitational force. According to the law of moments of forces for a system of rigid bodies m= F * d (2): where M – moment of force in the knee joint; F – force acting on the knee joint; d – distance from the centre of rotation of the hip joint to the knee joint.
Calculation of additional load: when the centre of rotation is shifted by Δx, the distance d changes by d+Δx. Therefore, the moment of force in the knee joint will be M’= F* (d + ∆x) (3), where M’ – moment of force when the centre of rotation changes; Δx – lateral displacement of the centre of rotation of the hip joint.
Difference in moments of forces before and after displacement of the centre of rotation: ∆M= M’- M (4), where – difference in the moment of force in the knee joint during displacement.
Additional load on the lateral surface of the knee joint from displacement: P=(∆ M)/d (5), where P – additional load on the lateral and medial surface of the knee joint from displacement.
A parametric model was created, setting dimensional and anatomical parameters, and used to study the biomechanics of hip and knee joints. The main goal was to determine the load on the lateral and medial plateau of the tibia in the knee joint, when the centre of rotation of the hip joint changes after hip arthroplasty by 0, 2, 4, 6, 8 mm, medial and lateral to the initial data. Researchers used a geometric model to study the change in knee joint angle due to hip joint displacement. The lower limb consists of two rigid segments, and the upper segment moves with the hip joint shift. Using trigonometric functions, the change in angle can be determined: Tan(θ)=(Δx/d) (6) and θ=artcatan (Δx/d) (7), where: θ – change in the angle of the knee joint.
It was assumed that d=0,4 m (this is the approximate distance from the hip joint to the knee for an adult). The load experiment was performed in the SolidWorks software suite using the SimulationXpress tool. Type of analysis: static, simulating standing on one leg.
RESULTS
As mentioned above, a change in the hip joint’s center of rotation after complete endoprosthetics can lead to a change in the mechanics of the knee joint and a decrease in its stability. The force acting vertically down through the center of rotation was calculated at 882,9 N for a patient with a 90 kg weight. The patient’s lower limb was modeled using SolidWorks software and SimulationXpress tool, examining the impact of two forces on the prosthesis head (figure 1).

Figure 1. Model of the lower limb with a prosthetic head of the hip joint, the force vectors acting on the prosthesis are indicated
The simulation process involved creating a geometric image and breaking it down into spatial elements, creating a grid. The program determined the dimensions of the elements based on volume, surface area, and geometric features. The model showed that shifting the hip joint center of rotation causes a change in hip angle, affecting the knee joint angle. This can lead to uneven load distribution, stressing the lateral and medial tibial condyles. Figure 2 shows the change in pressure in the knee joint in frontal and axial projections. The number indicates the area that receives the greatest pressure, and other colours indicate the surrounding areas where the load is distributed.
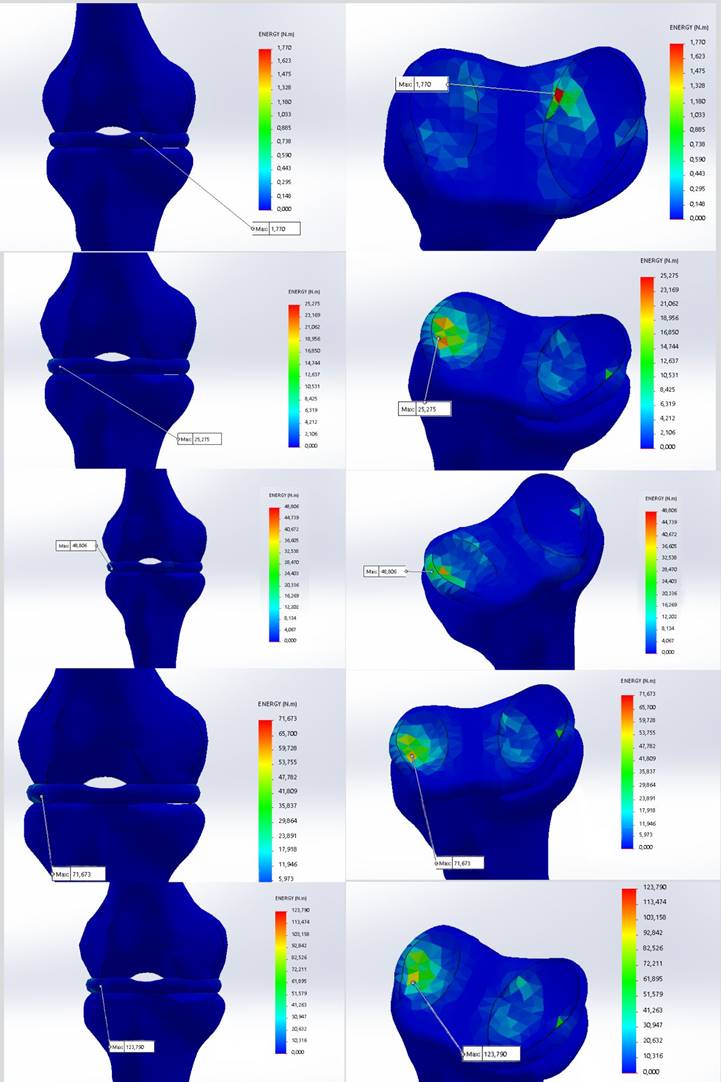
Figure 2. Model of the knee joint that reflects the load on the contact surfaces during medial displacement of the centre of rotation
The model reveals that the maximum pressure in the knee joint is 1,77 N⋅m in the anatomical position of the tibia’s center of rotation. When displaced, this pressure can increase tenfold and move to other positions. The load redistribution leads to increased pressure on areas of the joint surface not physiologically affected. When the hip joint’s center of rotation changes from zero, the angle of inclination changes, causing additional load on the knee joint’s medial surface. The angle change is linear and proportional to the displacement of the center of rotation. The data is listed in table 1.
|
Table 1. Change of angle when the centre of rotation is shifted |
|
|
Rotation centre displacement, mm |
Angle change, degrees |
|
2 |
0,287 |
|
4 |
0,573 |
|
6 |
0,859 |
|
8 |
1,146 |
The angle of inclination of the femur can affect joint movement, muscle and ligament tension, limb length, and uneven pressure on other joints, including the knee. The force acting on the lateral surface of the knee joint increases significantly in proportion to the displacement of the centre of rotation (table 2). Changes in hip tilt affect hip adductor muscles activity, affecting gait biomechanics. This may affect lower limb kinetic parameters and joint pressure vectors, but this aspect is beyond the scope of this study. The shift change is quite significant and can have pronounced effects.
|
Table 2. Force acting on the lateral surface of the joint during medial displacement of the centre of rotation |
||
|
Rotation centre displacement, mm |
Force acting on the lateral surface, N.m |
Displacement force difference, N.m |
|
0 |
1,77 |
0 |
|
2 |
25,275 |
23,505 |
|
4 |
48,806 |
46,836 |
|
6 |
71,673 |
69,903 |
|
8 |
123,79 |
122,02 |
Data on the maximum load on the surface of the knee joint during lateral displacement are shown in Table 3. Load growth is also linear. The table shows data on the additional load that occurs during displacement. As can be seen from Tables 2 and 3, the load on the tibial condyles increases tenfold, so changes in the knee must be considered when planning hip arthroplasty.
|
Table 3. Force acting on the medial surface of the joint during lateral displacement of the centre of rotation |
||
|
Rotation centre displacement, mm |
Force acting on the lateral surface, N.m |
Displacement force difference, N.m |
|
0 |
1,77 |
0 |
|
2 |
21,735 |
19,965 |
|
4 |
44,033 |
42,263 |
|
6 |
69,975 |
68,205 |
|
8 |
120,25 |
118,48 |
The authors also calculated the change in additional load per millimetre in the medial and lateral directions. The calculation results are presented in table 4. It can be seen that the change in load on the lateral surface of the knee joint when the centre of rotation shifts from 0 to 6 mm is approximately the same and averages 11,65±1 N/mm. However, when the centre of rotation is shifted from 6 to 8 mm, there is a significant increase in the load to 26,058 N/mm. A similar situation is observed with medial displacement. From the above data, it can be seen that with a displacement of more than 6 mm, the load on each mm increases by more than 2 times. These data deserve special attention, as such a bias may be critical from a clinical standpoint.
|
Table 4. Additional load on each mm that occurs when the centre of rotation is shifted, N⋅m |
||
|
Displacement, mm |
With lateral displacement of the centre of rotation |
With medialisation of the rotation centre |
|
from 0 to 2 mm |
9,982 |
11,752 |
|
2 to 4 mm |
11,149 |
11,765 |
|
4 to 6 mm |
12,971 |
11,433 |
|
6 to 8 mm |
25,137 |
26,058 |
Increased load on the tibial plateau may cause stress and pressure on knee joint structures so, a displacement of more than 6 mm can be critical for the functioning of the knee joint. The model suggests that altering the hip joint’s rotation during implantation can significantly alter the pressure distribution on the lower limb and knee joint. Comparing simulation data with real-world scenarios is crucial for understanding joint interaction. In the in vivo situation, bones and joints are located in a system connected by the musculoskeletal system, the condition of which will also contribute to load distribution.
DISCUSSION
The study investigates the impact of changes in the center of rotation after hip arthroplasty on knee joint load, highlighting the importance of understanding biomechanical conditions. A study by Bjarnason and Reikeras(6) found that 55 % of patients with total hip arthroplasty experience a change in the center of rotation, potentially leading to femoral displacement and reducing knee joint stability. When the centre of rotation is shifted medially from the normal position, the load on the lateral tibial condyle increases, which coincides with the results of the modelling in this study.
The redistribution of forces in the knee joint can lead to knee pain and osteoarthritis, as incorrect pressure distribution on the joint surface and subchondrial bones is a significant factor.(14-16) In vitro study by Bourne et al.(16) on cartilage tissue culture reveals that supraphysiological increases in hydrostatic pressure lead to changes in gene regulation, activating genes responsible for cellular respiration and suppressing processes like ossification, connective tissue development, and chondrocyte differentiation. This study explains the macro-level degenerative changes in cartilage tissue in response to prolonged pressure increases, particularly in the knee joint.
Studies show unequal displacement of the center of rotation, with medial displacement having less clinical effect and potentially reducing hip joint load on abductor muscles, but understanding these changes’ impact on the knee joint is crucial.(7;18,19) In a survey of 110 hip arthroplasty patients, Nieschk et al.(20) found that displacement of the center of rotation worsens mobility indicators, particularly the Barthel Index, and increases pain. The best indicators for all the studied parameters were provided by the exact anatomical location of the centre of rotation, thus confirming the need to preserve the centre of rotation as accurately as possible. Lerner et al.(21) study on musculoskeletal models found that deviation from tibia and femur alignment changes the peak contact force of the medial division by 51 N, and medial-lateral displacement of contact points by 41 N.
It is important to note that the results of this study are based on a mathematical model that, although tries to reproduce real biomechanical processes, still has its limitations. Additional experimental studies may be needed to confirm these results in a real-world clinical setting. It is also worth considering that other factors, such as the patient’s age, the condition of muscles and tendons, and other anatomical features, can affect the actual load on the knee joint after hip arthroplasty.(22) It should also be noted that the likelihood of complications is additionally due to changes in the overall biomechanics of the musculoskeletal system and forced posture, which may have occurred in the patient as an adaptation to the painful condition in the preoperative period.(23-25) Abolghasemian et al.(26) found that post-total arthroplasty, the joint’s rotation center shifts by 23,4 % and down by 20,8 %, causing a decrease in joint response and weakening hip muscle strength. This change may affect knee joint function in other kinetic positions.
Rajpura et al.(27) found 33 hip arthroplasty patients experienced an average 7mm displacement of the prosthesis head, altering muscle forces and bone tilt, potentially disrupting other joints. The consequence of this can be a change in the vectors of muscle forces and bone tilt, which also disrupts the work of other joints. Van Drongelen et al.’s(28) study reveals hip-knee joint changes after hip arthroplasty, with increased contact between femur and tibia, leading to 39 % increased pressure on the knee joint, suggesting the need for a musculoskeletal model.
The prevalence and clinical consequences of this pathology necessitate the identification of potential surgical causes of displacement and their reduction.(29) Benson et al.(30) study on 894 endoprosthetic patients revealed that the type of operational access significantly impacts the displacement of the hip rotation center. This displacement can have significant clinical consequences, so it is important to consider such aspects when planning surgery. Messer-Hannemann et al.(31) study highlights the importance of acetabular reaming and grinding in hip cup implantation to restore the prosthesis’s anatomical position and balance it with a healthy leg, addressing factors like dysplasia and deformity.
Marsh and Newman’s(32) review highlights the effectiveness of individualisation in hip and knee replacement, increasing implant survival rates to 98,2 % and 96,6 % after 20 years. This reduces complications like dislocation, loosening, and infection, and reduces revision surgery frequency. Computerisation of modelling and manufacturing expands implant use, but technical and economic factors hinder their spread. 3D modelling helps study knee joint biomechanics and joint relationships.(33)
CONCLUSIONS
This paper presents the development of a model of a human lower limb in SolidWorks software suite using the SimulationXpress tool to simulate standing on one leg. The study highlights the critical importance of understanding how changes in the center of rotation after hip arthroplasty impact the load distribution in the knee joint. Despite hip arthroplasty’s high success rate in restoring limb function and quality of life for patients with osteoarthritis and other degenerative hip diseases, it can lead to biomechanical changes in other joints, particularly the knee.
Lateral displacement of the center of rotation increases the load on the medial tibial condyle, while medial displacement increases the load on the lateral tibial condyle. Such changes can exacerbate knee pain and contribute to the development of osteoarthritis. The findings indicate that even minor shifts in the hip’s center of rotation can lead to significant changes in knee joint biomechanics, potentially resulting in uneven load distribution and increased pressure on non-physiological areas. This can cause degenerative changes and affect overall joint stability. It is crucial for orthopedic surgeons to consider the implications of hip rotation center displacement during arthroplasty. Accurate positioning of the prosthesis is essential to minimize adverse effects on the knee joint. The study underscores the value of advanced modeling techniques in predicting these outcomes and guiding surgical planning.
Future research should validate the model by comparing simulation results with real-world clinical data, explore post-arthroplasty hip-knee joint interaction, and investigate patient-specific factors like age, muscle condition, and preoperative biomechanics to improve surgical outcomes.
REFERENCES
1. Ferguson RJ, Palmer AJ, Taylor A, Porter ML, Malchau H, Glyn-Jones S. Hip replacement. Lancet. 2018;392(10158):1662-1671. https://doi.org/10.1016/S0140-6736(18)31777-X
2. Zagra L. Advances in hip arthroplasty surgery: What is justified? EFORT Open Rev. 2017;2(5):171-178. https://doi.org/10.1302/2058-5241.2.170008
3. Babii M. Telerehabilitation model in operated individuals with upper limb and chest trauma due to road traffic accidents. Bull Med Biol Res. 2023;5(4):8-16. https://doi.org/10.61751/bmbr/4.2023.08
4. Zazirnyi IM. Total hip arthroplasty during last 25 years. Trauma. 2020;21(5):32-41. https://doi.org/10.22141/1608-1706.5.21.2020.217088
5. Venher IK, Herasymiuk NI, Kostiv SYa, Loyko II, Khvalyboha DV. Nonspecific dysplasia of the connective tissue – a factor of venous thromboembolic complications in endoprosthetics of hip joints. Int J Med Med Res. 2020;6(1):35-42. https://doi.org/10.11603/ijmmr.2413-6077.2020.1.11047
6. Latka K, Kozlowska K, Waligora M, Kolodziej W, Olbrycht T, Chowaniec J, Hendryk S, Latka M, Latka D. Efficacy of discogel in treatment of degenerative disc disease: A prospective 1-year observation of 67 patients. Brain Sci. 2021;11(11):1434. https://doi.org/10.3390/brainsci11111434
7. Bjarnason JA, Reikeras O. Changes of center of rotation and femoral offset in total hip arthroplasty. Ann Transl Med. 2015;3(22):355.
8. Traina F, De Fine M, Biondi F, Tassinari E, Galvani A, Toni A. The influence of the centre of rotation on implant survival using a modular stem hip prosthesis. Int Orthop. 2009;33(6):1513-1518. https://doi.org/10.1007/s00264-008-0710-0
9. Ugurbas MV. Dupuytren’s contracture treated with collagenase Clostridium histolyticum. International J Med Med Res. 2023;9(1):39-46.
10. Saleeva AD, Avrunin OG, Kabanenko IV, Zaitsev VM, Datsok OM, Boboshko RO, Dondoreva IS, Chugaev AYu, Baev PO, Korneev SV, Lytvynenko OM. Functional anatomy of the musculoskeletal system. Kharkiv: Kharkiv National University of Radio Electronics; 2023.
11. Smahlii ZV. The effect of mechanical skin damage on manifestations of endotoxicosis and immune response under the influence of skeletal trauma complicated by acute blood loss and PRP-therapy effectiveness. Bull Med Biol Res. 2022;4(1):95-102. https://doi.org/10.11603/bmbr.2706-6290.2022.1.12977
12. Diniz KMA, Resende RA, Mascarenhas RO, Silva HJ, Filho RGT, Mendonça LM. Hip passive stiffness is associated with hip kinematics during a single-leg squat. J Bodyw Mov Ther. 2021;28:68-74. https://doi.org/10.1016/j.jbmt.2021.06.008
13. Haiko HV, Haluzynskyi OA, Burburska SV. Using 3D modeling with the manufacture of plastic prototypes in traumatology and orthopedics (clinical examples). Trauma. 2019;20(1):89-97. https://doi.org/10.22141/1608-1706.1.20.2019.158676
14. Sylwander C, Larsson I, Haglund E, Bergman S, Andersson MLE. Pressure pain thresholds in individuals with knee pain: A cross-sectional study. BMC Musculoskeletal Disorders. 2021;22:516. https://doi.org/10.1186/s12891-021-04408-0
15. Navruzov SN, Polatova DSh, Gafoor-Akhunov MA, Gabdikarimov KH. The value of marker proteins p53, bcl-2, Ki-67 in predicting the effectiveness of treatment for osteogenic sarcoma of tubular bones. Vopr Onkol. 2012;58(5):691–693.
16. Polatova DSh, Islamov UF, Davletov RR, Savkin AV, Sharipov MM. Oncologic outcomes of pelvic bone sarcomas surgical. Int J Health Sci. 2021;5(3):252–259. https://doi.org/10.53730/ijhs.v5n3.1467
17. Bourne L, Hesketh A, Sharma A, Bucca G, Bush PG, Staines KA. The effects of physiological and injurious hydrostatic pressure on murine ex vivo articular and growth plate cartilage explants: An RNAseq study. Front Endocrinol. 2023;14(10):3389. https://doi.org/10.3389/fendo.2023.1278596
18. Baghdadi YM, Larson AN, Sierra RJ. Restoration of the hip center during THA performed for protrusio acetabuli is associated with better implant survival. Clin Orthop Relat Res. 2013;471(10):3251-3259. https://doi.org/10.1007/s11999-013-3072-x
19. Pulatova A, Mamedaliyeva N, Omarova G, Urazbayeva G, Veliyeva A. Pelvic floor muscle exercises plus biofeedback versus pelvic floor muscle exercises for patients with stress urinary incontinence: A systematic review and meta-analysis of randomized controlled trials. Electron J Gen Med. 2023;20(5):em520. https://doi.org/10.29333/ejgm/13411
20. Nieschk C, Abelmann-Brockmann J, Lisitano L, Fenwick A, Röttinger H, Ecker M, Mayr E, Röttinger T. Clinical effects of different center of rotation reconstructions in total hip arthroplasty after femoral neck fractures: A cohort study including a follow-up analysis on patient’s mobility and daily living ability. J Orthop Trauma. 2023;24(1):58. https://doi.org/10.1186/s10195-023-00738-y
21. Lerner ZF, DeMers MS, Delp SL, Browning RC. How tibiofemoral alignment and contact locations affect predictions of medial and lateral tibiofemoral contact forces. J Biomech. 2015;48(4):644-650. https://doi.org/10.1016/j.jbiomech.2014.12.049
22. Hrubar YuO, Hrubar MYu. Evaluation of early clinical and functional results after suturing of meniscal ruptures under arthroscopic control with “аll-inside” and “inside-out” techniques. Bull Med Biol Res. 2021;3(2):16-21. https://doi.org/10.11603/bmbr.2706-6290.2021.2.11726
23. Mendis MD, Wilson SJ, Hayes DA, Hides JA. Hip muscle atrophy in patients with acetabular labral joint pathology. Clin Anat. 2020;33(4):538-544. https://doi.org/10.1002/ca.23429
24. Zhang H, Zhou J, Liu Y, Guan J, Ding H, Wang Z, Dong O. Mid-term and long-term results of restoring rotation center in revision hip arthroplasty. J Orthop Surg Res, 2020;15:152. https://doi.org/10.1186/s13018-020-01670-1
25. Latka K, Kolodziej W, Domisiewicz K, Pawus D, Olbrycht T, Niedzwiecki M, Zaczynski A, Latka D. Outpatient spine procedures in Poland: Clinical outcomes, safety, complications, and technical insights into an ambulatory spine surgery center. Healthcare (Switzerland). 2023;11(22):2944. https://doi.org/10.3390/healthcare11222944
26. Abolghasemian M, Samiezadeh S, Jafari D, Bougherara H, Gross AE, Ghazavi MT. Displacement of the hip center of rotation after arthroplasty of Crowe III and IV dysplasia: A radiological and biomechanical study. J Arthroplasty. 2013;28(6):1031-1035. https://doi.org/10.1016/j.arth.2012.07.042
27. Rajpura A, Asle SG, Ait Si Selmi T, Board T. The accuracy of restoration of femoral head centre of rotation in the anteroposterior plane after uncemented total hip arthroplasty: A CT-based study. Bone Joint Res. 2022;11(3):180-188. https://doi.org/10.1302/2046-3758.113.BJR-2021-0378.R2
28. van Drongelen S, Wesseling M, Holder J, Meurer A, Stief F. Knee load distribution in hip osteoarthritis patients after total hip replacement. Front Bioeng Biotechnol. 2020;8:578030. https://doi.org/10.3389/fbioe.2020.578030
29. Shaprynskyi V, Nazarchuk O, Faustova M, Mitiuk B, Dmytriiev D, Dobrovanov O, Kralinsky K, Babina Y. Some aspects of infectious complications in patients with surgical diseases – Multicentr trials. Lek Obzor. 2020;69(7-8):257-260.
30. Benson RJ, Govindarajan M, Muir JM, Lamb IR, Sculco PK. Surgical approach and reaming depth influence the direction and magnitude of acetabular center of rotation changes during total hip arthroplasty. Arthroplast Today. 2020;6(3):414-421. https://doi.org/10.1016/j.artd.2020.04.003
31. Messer-Hannemann P, Bätz J, Lampe F, Klein A, Püschel K, Campbell GM, Morlock M. The influence of cavity preparation and press-fit cup implantation on restoring the hip rotation center. Clin Biomech. 2019;63:185-192. https://doi.org/10.1016/j.clinbiomech.2019.03.006
32. Alvarado MAG. Gentrification and Community Development: An analysis of the main lines of research. Gentrification 2023;1:2–2. https://doi.org/10.62486/gen20232.
33. Auza-Santivañez JC, Apaza-Huanca B, Diaz-Guerrero JL, Vallejos-Rejas DRE, Zelaya-Espinoza Y, Vargas-Gallego I, et al. Relevance of ultrasound detection and assessment of vascular calcifications in chronic kidney disease. Multidisciplinar (Montevideo) 2024;2:77–77. https://doi.org/10.62486/agmu202477.
34. Ayala DP, Falero DML, Pita MM, González IC, Silva JW. Ozone therapy in periodontal disease in type 2 diabetic patients. Odontologia (Montevideo) 2024;2:120–120. https://doi.org/10.62486/agodonto2024120.
Benavidez AMV, Ozeta RJN, Davila CAC, Hernandez OH, Mogollon JAY. Conceptual maps using Cmap Tools and student learning at a National Intercultural University Fabiola Salazar Leguía of Bagua. Multidisciplinar (Montevideo) 2024;2:107–107. https://doi.org/10.62486/agmu2024107.
35. Cano CAG. Education, urbanism, and gentrification: convergence of issues and solutions. Gentrification 2023;1:1–1. https://doi.org/10.62486/gen20231.
36. Cardozo GT. Community development promoted by policies: an analysis from the perspective of gentrification. Gentrification 2023;1:3–3. https://doi.org/10.62486/gen20233.
37. Dinkar AK, Haque MA, Choudhary AK. Enhancing IoT Data Analysis with Machine Learning: A Comprehensive Overview. LatIA 2024;2:9–9. https://doi.org/10.62486/latia20249.
38. Espinoza GYG. Transforming the Salitre campus into a smart campus: proposal of smart initiatives for the Gerardo Barrios University of El Salvador. LatIA 2024;2:102–102. https://doi.org/10.62486/latia2024102.
39. Galván LNO, Ayala DP, Lozano IM, Falero DML, Silva JW. Breastfeeding, Oral Habits, and Malocclusions in Children Aged 3 to 6 Years. Odontologia (Montevideo) 2024;2:101–101. https://odonto.ageditor.uy/index.php/odonto/article/view/101
40. García EA, Curbelo ML, Iglesias MSS, Falero DML, Silva JW. Oral lesions associated with the use and care of dentures in the elderly. Odontologia (Montevideo) 2024;2:100–100. https://doi.org/10.62486/agodonto2024100.
41. González MS, Pérez AG. Proposal of actions to improve accessibility at the Hotel Las Yagrumas, Artemisa. Management (Montevideo) 2024;2:25–25. https://doi.org/10.62486/agma202425.
42. Hernández-Lugo M de la C. Artificial Intelligence as a tool for analysis in Social Sciences: methods and applications. LatIA 2024;2:11–11. https://doi.org/10.62486/latia202411.
43. Iyengar MS, Venkatesh R. A Brief Report on Building Customer Loyalty in Luxury hotels: A Universal Approach. Management (Montevideo) 2024;2:32–32. https://doi.org/10.62486/agma202432.
44. Iyengar MS, Venkatesh R. Customer preferences while booking accommodation in hotels: Customer Behaviour and Hotel Strategies. Management (Montevideo) 2024;2:31–31. https://doi.org/10.62486/agma202431.
45. León MP. The impact of gentrification policies on urban development. Gentrification 2023;1:4–4. https://doi.org/10.62486/gen20234.
46. Lozano IM, Molina YG, Santos IF, Galván LNO, Pérez AP, Becerra CEC. Behavior of Denture Stomatitis in Adults Over 45 Years of Age. Odontologia (Montevideo) 2024;2:102–102. https://doi.org/10.62486/agodonto2024102.
47. Macedo GC, Auza-Santivañez JC, Rejas DREV, Sarmiento RAQ, Canaviri JJF, Laime LHS. Giant multiloculated omental cyst in a pediatric patient. Case report and literature review. Multidisciplinar (Montevideo) 2024;2:88–88. https://doi.org/10.62486/agmu202488.
48. Martinez AME, Warnes CD. English language skills and their influence on the academic performance of high school students in the public schools of Cereté – Córdoba. Multidisciplinar (Montevideo) 2024;2:108–108. https://doi.org/10.62486/agmu2024108.
49. Ramirez GAM, Murillo MYR, Valderrama PJC, Patiño ML, Mora YJR. Analysis of the strategic plan for the Acuña Ventures SAS company in Yopal city, Colombia. Management (Montevideo) 2024;2:29–29. https://doi.org/10.62486/agma202429.
50. Sonal D, Mishra K, Haque A, Uddin F. A Practical Approach to Increase Crop Production Using Wireless Sensor Technology. LatIA 2024;2:10–10. https://doi.org/10.62486/latia202410.
51. Vargas OLT, Agredo IAR. Active packaging technology: cassava starch/orange essential oil for antimicrobial food packaging. Multidisciplinar (Montevideo) 2024;2:102–102. https://doi.org/10.62486/agmu2024102.
52. Marsh M, Newman S. Trends and developments in hip and knee arthroplasty technology. J Rehabil Assist Technol Eng. 2021;8. https://doi.org/10.1177/2055668320952043
53. Siddiqui MF, Alam A, Kalmatov R, Mouna A, Villela R, Mitalipova A, Mrad YN, Rahat SAA, Magarde BK, Muhammad W, Sherbaevna SR, Tashmatova N, Islamovna UG, Abuassi MA, Parween Z. Leveraging healthcare system with nature-inspired computing techniques: An overview and future perspective. Stud Comput Intell. 2023;1066:19–42. https://doi.org/10.1007/978-981-19-6379-7_2
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Oleksandr Zubkov
Data curation: Oleksandr Zubkov, Victor Torchynskyi
Formal analysis: Oleksandr Zubkov, Victor Torchynskyi
Research: Oleksandr Zubkov, Victor Torchynskyi
Methodology: Victor Torchynskyi
Project management: Oleksandr Zubkov
Resources: Victor Torchynskyi
Software: Oleksandr Zubkov, Victor Torchynskyi
Supervision: Oleksandr Zubkov
Validation: Oleksandr Zubkov, Victor Torchynskyi
Display: Oleksandr Zubkov, Victor Torchynskyi
Drafting - original draft: Oleksandr Zubkov, Victor Torchynskyi
Writing - proofreading and editing: Oleksandr Zubkov, Victor Torchynskyi