doi: 10.56294/saludcyt2024.549
REVIEW
Duplex ultrasonography for screening and monitoring of carotid artery stenosis for risk stratification of ischemic stroke
Ultrasonografía dúplex para el cribado y la monitorización de la estenosis de la arteria carótida para la estratificación del riesgo de ictus isquémico
Almas Saduakas1 ![]() *, Kuralbay Kurakbayev2
*, Kuralbay Kurakbayev2 ![]() , Yenglik Askar3
, Yenglik Askar3 ![]() , Mairash Baimuratova3
, Mairash Baimuratova3 ![]()
1National Scientific Center of Surgery, Department of Vascular Surgery. Almaty, Kazakhstan.
2Kazakhstans Medical University “KSPH”, Department of Public Health and Social Sciences. Almaty, Kazakhstan.
3International Clinic of Reproductive Health “PERSONA”, Department of IVF. Almaty, Kazakhstan.
Cite as: Saduakas A, Kurakbayev K, Askar Y, Baimuratova M. Duplex ultrasonography for screening and monitoring of carotid artery stenosis for risk stratification of ischemic stroke. Salud, Ciencia y Tecnología . 2024; 4:.549. https://doi.org/10.56294/saludcyt2024.549
Submitted: 15-01-2024 Revised: 17-05-2024 Accepted: 11-10-2024 Published: 12-10-2024
Editor:
Dr.
William Castillo-González ![]()
Corresponding Author: Almas Saduakas *
ABSTRACT
Objetive: to evaluate the efficiency of Duplex Ultrasonography (DUS) for monitoring and screening of Carotid Artery Stenosis (CAS).
Method: PubMed, Web of Science, Cochrane, and SCOPUS were searched for relevant articles. The quality assessment of the included studies was conducted according to the Cochrane Risk of Bias Tool.
Results: our meta-analysis included six articles. We found that carotid DUS could detect mild CAS in 25 %, moderate CAS in 13 %, severe CAS in 14,5 % of the examined vessels, detection of carotid artery plaques in 36,5 % of the examined vessels, and abnormal intima thickness in 21,5 % of the examined vessels.
Conclusion: DUS is an important exam in the identification of patients with symptomatic CAS. It can improve clinical practice and provide cost-effective management for CAS. Carotid DUS showed high specificity and sensitivity in the diagnosis of CAS, especially a severe degree of stenosis.
Keywords: Duplex Ultrasonography; Ischemic Stroke; Meta-Analysis; Carotid Artery Stenosis; Diagnostic Imaging.
RESUMEN
Objetivo: evaluar la eficacia de la ultrasonografía dúplex (EDD) para la monitorización y el cribado de la estenosis de la arteria carótida (EAC).
Método: se realizaron búsquedas de artículos relevantes en PubMed, Web of Science, Cochrane y SCOPUS. La evaluación de la calidad de los estudios incluidos se realizó según la Herramienta Cochrane de Riesgo de Sesgo (Cochrane Risk of Bias Tool).
Resultados: nuestro metaanálisis incluyó seis artículos. Se observó que la EUS carotídea podía detectar una EAC leve en el 25 %, una EAC moderada en el 13 % y una EAC grave en el 14,5 % de los vasos examinados, la detección de placas en la arteria carótida en el 36,5 % de los vasos examinados y un grosor anormal de la íntima en el 21,5 % de los vasos examinados.
Conclusiones: la EUS es un examen importante en la identificación de pacientes con EAC sintomática. Puede mejorar la práctica clínica y proporcionar un tratamiento rentable de la EAC. La EUS carotídea mostró una elevada especificidad y sensibilidad en el diagnóstico de la EAC, especialmente en el caso de un grado grave de estenosis.
Palabras clave: Ecografía Dúplex; Ictus Isquémico; Meta-Análisis; Estenosis de la Arteria Carótida; Diagnóstico por Imagen.
INTRODUCTION
Research Problem
Begin by clearly defining the research problem within the first or second paragraph. Highlight the gap in current knowledge or practice that your study aims to address. For instance, Despite the known impact of CAS on stroke risk, there remains uncertainty regarding the most effective methods for its screening and monitoring.
Research Aim and Questions
While the manuscript eventually states an aim, the transition from background to the study's purpose lacks clarity, and research questions are not explicitly stated.
Clearly articulate the aim of the study at the end of the introduction. Following the statement of aim, present specific research questions that the study seeks to answer. This could be structured as follows:
The aim of study is to evaluate the efficiency of duplex ultrasonography in the monitoring and screening of carotid artery stenosis. Specifically, we seek to answer the following research questions:
1. How effective is Duplex U/S compared to other imaging modalities such as magnetic resonance angiography or computed tomography angiography in diagnosing and predicting the course of the carotid artery stenosis for ischemic stroke?
2. How many errors does Duplex Ultrasonography of the carotid arteries have in identifying stenosis in relation with different patients who are in various age groups, are different sexes, or are with other diseases like hypertension or diabetes?
3. What are the best practices and criteria to be used in performing Duplex Ultrasonography both in screening and in the periodical check-up for the evaluation of carotid artery stenosis as a risk marker of ischemic stroke, and how do they relate to the accuracy and authenticity of the diagnostic findings?
Worldwide, cerebrovascular stroke is ranked as the third most common cause of death, and most likely the primary factor contributing to long-term disability.(1) Ischemic and hemorrhagic strokes are the two primary types. Ischemic strokes account for about 87 % of all strokes, with carotid artery stenosis (CAS), hypertension, and cardiac arrhythmias being the primary causes.(2,3) About 8 % of all strokes are caused by CAS. Prior studies have demonstrated that in patients with transient ischemic attack (TIA) or minor ischemic stroke, CAS is linked to an increased risk of recurrence.(4) The opportunity to proceed with carotid artery revascularization in order to stop a new ischemic episode that could result in a stroke or death is the main reason for identifying people with CAS.(5,6)
Carotid revascularization could be accomplished through conventional or endovascular surgical treatment.(7) The idea is to restore enough blood flow. Strong evidence suggests that, within two weeks of the neurologic episode, a carotid endarterectomy should be carried out.(8) The degree of CAS continues to be the primary consideration in determining the best course of treatment. Clinically, there are four categories for extracranial CAS: mild (<50 %), moderate (50–69 %), severe (70–99 %), and blockage (100 %).(9) Every threshold affects the patient's options for treatment. The simplicity, reproducibility, and noninvasiveness of carotid duplex ultrasonography (DUS) have led to its global adoption. Risk stratification for future cerebrovascular and cerebral events is the primary motivation for assessing the severity of atherosclerosis.(10,11) Atherosclerosis can be detected and tracked with carotid DUS, which uses carotid intima-media thickness (IMT) as a surrogate measure.(14)
Understanding the thresholds of carotid IMT associated with higher risk is essential for guiding interventions in carotid artery stenosis and ischemic stroke risk. DUS measures IMT to assess atherosclerosis and vascular damage, aiding risk stratification. IMT values, alongside other risk indicators, inform treatment decisions like closer monitoring, risk factor modification, or interventions, thus improving ischemic stroke prevention.(13)
Numerous studies have demonstrated the value of carotid IMT measures in assessing the incidence and risk of cardiovascular and cerebral diseases. Evaluation of carotid plaque and its morphology using DUS are also essential for predicting the occurrence of an ischemic stroke.(14) Comprehensive DUS interpretation is crucial for everyday clinical settings, even though it is still debatable whether screening for asymptomatic CAS or routine carotid IMT measurement should be done on a general population basis.(15)
DUS has been compared to other imaging techniques like CT angiography (CTA), MR angiography (MRA), and digital subtraction angiography (DSA) regarding sensitivity, specificity, patient safety, and cost-effectiveness in evaluating carotid artery stenosis. While CTA and MRA offer similar diagnostic accuracy to DUS, they involve risks such as radiation exposure and contrast agent use. DSA, although highly accurate, is invasive and costly. DUS, on the other hand, is non-invasive, safer, and more cost-effective. However, it may have limitations in severe stenosis assessment. The choice of imaging modality depends on clinical needs, patient factors, and resource availability.(16,17)
Our study aimed to evaluate the efficiency of duplex ultrasonography for monitoring and screening of carotid artery stenosis.
METHOD
We utilized the criteria of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) to conduct our study.(18)
Search strategy
The following search strategy was employed to search several databases: (“Duplex Ultrasonography” OR “Ultrasonography”) AND (“Carotid Artery Stenosis” OR “Carotid Artery Disease” OR “Carotid Artery Occlusion”) AND (“Stroke” OR “Ischemic Stroke”).
Study Selection
The following processes were used to carry out the screening: First, using EndNote Software(19) we exported the articles from research databases into a Microsoft Excel(20) sheet. Next, we checked the article titles and abstracts that were included in the Excel sheet. The full-text screening of the involved studies from the second step constituted the last step.
The criteria used to select studies for inclusion were:
1. Study design (we included non-randomized or randomized clinical trials (RCTs) and observational studies).
2. Participants (patients suffering from CAS).
3. Intervention (screening and monitoring of CAS using DUS).
4. Outcomes (mild artery occlusion (less than 50 %), moderate artery occlusion (50–69 %), severe artery occlusion (70–99 %), abnormal intima-media thickness, and detection of carotid artery plaques).
Inclusion criteria
1. Recent studies above 2010. Because incorporating recent studies dated from 2010 onwards ensures relevance to current medical practices, reflecting advancements in technology, treatment strategies, and understanding of diseases. It enhances the validity and applicability of findings, providing up-to-date evidence to inform clinical decision-making and improve patient care.
2. Studies that included both males and females.
3. We included retrospective and prospective studies.
Inclusion criteria
· Study Design: Original research studies (including RCTs, cohort studies, case-control studies, and cross-sectional studies), systematic reviews, and meta-analyses published in peer-reviewed journals.
· Population: Adults diagnosed with or at risk of carotid artery stenosis, with or without a history of ischemic stroke.
· Intervention/Exposure: Studies utilizing duplex ultrasonography for screening, monitoring, or risk stratification of carotid artery stenosis.
· Comparator/Control: Studies comparing duplex ultrasonography with other imaging modalities or clinical assessments for detecting carotid artery stenosis or comparing different duplex ultrasonography protocols.
Outcome Measures
· Primary outcome: Detection and quantification of carotid artery stenosis. Secondary outcomes: Incidence of ischemic stroke or other cerebrovascular events, diagnostic performance metrics of duplex ultrasonography, and related adverse events.
· Language and Time Frame: English-language publications with no restrictions on publication date.
Exclusion criteria
1. Reviews, surveys, abstracts, and meta-analyses.
2. studies in which there was an unreasonably lengthy interval (more than four weeks) between the reference and index tests because the patient's stenosis changed and there was a chance that their condition might worsen over time.
Data Collection
The Web of Science, Cochrane Library, Scopus, and PubMed databases were searched until March 2024 for publications that fulfilled the eligibility requirements. Three categories of data were collected from the listed studies: the first category includes demographic and baseline data of the participants, such as study design, year, author, country, age, study period, gender, hypertension, dyslipidemia, and diabetes mellitus. The second category included the outcomes for analysis including Mild artery occlusion (less than 50 %), moderate artery occlusion (50–69 %), severe artery occlusion (70–99 %), abnormal intima-media thickness, and detection of carotid artery plaques. The third category included data from quality assessment.
Quality Assessment
The National Heart, Lung, and Blood Institute's (NHLB) quality assessment tool was employed to evaluate the possibility of bias in the observational studies that were included.(21) Cochrane risk of bias tool(22) was used for the assessment of the risk of bias of the included trial.(23) We evaluated the quality of this study in accordance with The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Guidelines.
Statistical Analysis
The data that we extracted from the involved studies was analyzed using Open Meta analyst software.(24) There were dichotomous results in our search. Pooled proportion and a 95 % confidence interval (CI) were used in our data analysis. A fixed-effects model was utilized to analyze the homogeneous data, while a random-effects model was employed to analyze the heterogeneous data. The I2 and p-value of the Chi-square tests were utilized to estimate heterogeneity among the data. A major indicator of the existence of heterogeneity was P < 0,1 values. We attempted to use Cochrane's leave-one-out technique(25) to deal with the inconsistency of heterogeneous results.
RESULTS
Summary of included studies
The electronic search is illustrated in figure 1.
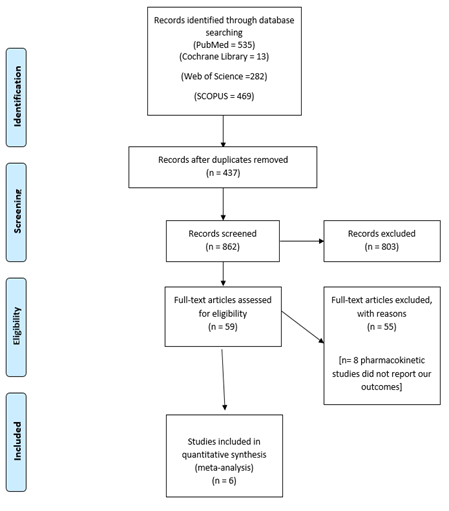
Figure 1. Shows a PRISMA flow diagram of our literature search
A total of 1 051 patients at risk of ischemic stroke as they suffer from carotid artery stenosis were analyzed in our study from six included studies.(23,36,37,38,39) All patients underwent DUS for the assessment and detection of carotid artery stenosis. The mean age of participants was 62,9 years. Data of the included studies and demographic data of patients are described in table 1-2.
|
Table 1. Described data of the included studies, demographic data of patients |
|||||
|
Study ID |
Country |
Study design |
Study duration |
Sample size |
Age (mean) |
|
Higgins et al.(22) |
Italy |
Prospective cohort study |
2006-2010 |
416 |
54 |
|
Barlinn et al.(36) |
Germany |
Retrospective cohort study |
2012 |
303 |
72 |
|
Cui et al.(37) |
China |
Prospective cohort study |
2012-2014 |
54 |
63.06 |
|
Li et al.(38) |
China |
Prospective cohort study |
2018-2019 |
98 |
66 |
|
Saxhaug et al. (23) |
Norway |
Clinical trial |
2021 |
80 |
71.5 |
|
Shehata et al.(39) |
Egypt |
case-control study |
2017-2018 |
100 |
51.35 |
|
Table 2. Described data of the included studies, demographic data of patients |
||||||
|
Study ID |
Male (n) |
Female (n) |
BMI (kg/m2) |
Hypertension n (%) |
Diabetes mellitus (n) |
Hyperlipidemia |
|
Higgins et al.(22) |
304 |
112 |
26 ± 2,7 |
34 (40) |
17 (20) |
13 (15) |
|
Barlinn et al.(36) |
176 |
127 |
NR |
NR |
NR |
NR |
|
Cui et al.(37) |
32 |
22 |
NR |
NR |
NR |
NR |
|
Li et al.(38) |
75 |
23 |
25,22 ± 3,79 |
72 (73) |
26 (26,5) |
37 (37,7) |
|
Saxhaug et al.(23) |
42 |
38 |
27,9 ±4 |
NR |
11 (14) |
15 (19) |
|
Shehata et al.(39) |
31 |
69 |
NR |
100 (100 %) |
NR |
NR |
Results of risk of bias
The result of the quality evaluation of the observational studies yielded an overall score of 9,8 out of 14 based on the NHLB tool of quality evaluation. Table 3 shows the quality assessment of the included studies in detail.
|
Table 3. Showing Quality assessment for included retrospective studies |
|||||
|
|
Higgins et al.(22) |
Barlinn et al.(36) |
Cui et al.(37) |
Li et al.(38) |
Shehata et al.(39) |
|
1. Was the research question or objective in this paper clearly stated? |
1 |
1 |
1 |
1 |
1 |
|
2. Was the study population clearly specified and defined? |
1 |
1 |
1 |
* |
1 |
|
3. Was the participation rate of eligible persons at least 50 %? |
1 |
1 |
1 |
* |
1 |
|
4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? |
1 |
1 |
1 |
1 |
1 |
|
5. Was a sample size justification, power description, or variance and effect estimates |
0 |
0 |
0 |
0 |
0 |
|
6. For the analyses in this paper, were the exposure (s) of interest measured prior to the outcome(s) being measured? |
1 |
1 |
1 |
1 |
1 |
|
7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? |
1 |
1 |
1 |
1 |
1 |
|
8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? |
N\A |
N\A |
N\A |
N\A |
N\A |
|
9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
1 |
0 |
0 |
* |
1 |
|
10. Was the exposure(s) assessed more than once over time? |
0 |
0 |
0 |
0 |
0 |
|
11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
1 |
1 |
1 |
1 |
1 |
|
12. Were the outcome assessors blinded to the exposure status of participants? |
* |
* |
* |
* |
* |
|
13. Was loss to follow-up after baseline 20 % or less? |
1 |
1 |
1 |
* |
1 |
|
14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? |
1 |
1 |
1 |
1 |
1 |
|
Total score (out of 14) |
11/14 |
10/14 |
10/14 |
7/14 |
11/14 |
|
Key: 1 = Yes, 0 = No, * = Not reported, N/A = Not applicable |
|||||
Saxhaug et al.(23) is the only included trial and its risk of bias assessment shows a high risk of randomization and allocation concealment and a low risk of blindness.
Analysis of outcomes
Mild artery occlusion (less than 50 %). Five studies(24,27,28,29,30) reported and analyzed the data of this outcome. Out of 1405 vessels, DUS detected occlusion less than 50 % in 352 vessels. The pooled proportion was 28,4 %, 95 % CI (14,9 %, 41,9 %). Data showed heterogeneity (P=0.001) (I2 =97,43 %) (figure 2).

Figure 2. Demonstrates the analysis of mild artery occlusion (less than 50 %)
Moderate artery occlusion (50–69 %). Moderate artery occlusion was assessed by six studies.(24,27,28,29,30,31) The analysis showed that DUS detected 193 vessels with moderate occlusion from 1503 examined vessels. The pooled proportion was 14,3 %, 95 % CI (7 %, 21,6 %). Data showed heterogeneity (P=0,001) (I2 =97,9 %) (figure 3).

Figure 3. Demonstrates the analysis of moderate artery occlusion (50–69 %)
Severe artery occlusion (70–99 %). A total of 1 403 vessels were analyzed by five of the included studies.(24,28,29,30,31) DUS detected severe occlusion with 201 vessels. The pooled proportion was 17,2 %, 95 % CI (7,6 %, 26,8 %). Data showed heterogeneity (P=0,001) (I2 =98,4 %) (figure 4).

Figure 4. Demonstrates the analysis of severe artery occlusion (70–99 %)
Abnormal intima-media thickness. Two studies(24,27) reported this outcome. Our analysis showed that DUS detected 78 arteries out of 360 arteries with abnormal intima thickness. The pooled proportion was 21,3 %, 95 % CI (15,1 %, 27,6 %). Data was homogeneous (P=0,139) (I2 =54,4 %) (figure 5).

Figure 5. Demonstrates the analysis of abnormal intima media thickness
Detection of carotid artery plaques. Two studies(30,31) reported this outcome. Our analysis showed that DUS detected carotid artery plaques in 129 arteries. The pooled proportion was 65,6 %, 95 % CI (1 %, 1,32 %). Data showed heterogeneity (P=0,001) (I2 =99,56 %) (figure 6).

Figure 6. Demonstrates the analysis of the detection of carotid artery plaques
Netuka et al.(30) reported that the diagnostic accuracy of CDUS was 74,07 % (160/216 vessels) while Mostafa et al.(28) found that the diagnostic accuracy of CDUS was 76 % (255/336 vessels). The sensitivity of DUS in the diagnosis of mild, moderate, and severe carotid stenosis were 78,18 %, 50 %, and 100 %, respectively as proved by Netuka et al.(30). Additionally, they found that the specificity of DUS in the diagnosis of mild, moderate, and severe carotid stenosis was 79,05 %, 93,36 %, and 98,10 %, respectively. On the other hand, Mostafa et al.(28) reported that the specificity and sensitivity of DUS were 67 % and 87 %, respectively.
DISCUSSION
A significant contributing factor to ischemic stroke is CAS, which is thought to be the cause of 8–15 % of cases. In order to decrease the impact of this disease, we must enhance our methods for stroke early detection and treatment.(26) Four imaging modalities are commonly used to diagnose CAS: computed tomographic angiography (CTA), magnetic resonance angiography (MRA), carotid duplex ultrasound (CDUS), and invasive cerebral angiography.(27,28) The advancement of imaging technology has made it possible to enhance the methods used to diagnose CAS. For example, the position and degree of CAS, as well as the state of the surrounding wall-adherent plaques, can be assessed by carotid DUS, digital subtraction angiography (DSA), and MRA. Although it is still uncertain how accurate non-invasive imaging procedures like MRA and CDUS are, they are replacing DSA in the detection of CAS because they are now widely accessible.(29) This systematic review and meta-analysis aimed to assess the efficiency of CDUS for monitoring and screening of CAS.
In our study, we found that CDUS could detect mild CAS in 25 % of the vessels, moderate CAS in 13 % of the examined vessels, and severe CAS in 14,5 % of the examined vessels. Regarding the detection of carotid artery plaques and abnormal intima thickness, CDUS detected them in 36,5 % and 21,5 % of the included vessels, respectively.
According to earlier findings, CDUS assessments typically overestimate the severity of stenosis. Due to variations in the imaging principles used for CDUS, several false-positive results were produced by the CDUS. CDUS images improve the visibility of plaques and show the structure of vascular lumens and walls. By making intravascular membrane thickness and structure visible, this improved imaging could result in a higher percentage of accurate diagnoses.(30,31,32)
Our findings correlate with those of previous research. Zavanone et al.(32) conducted a review to evaluate the role of DUS in the detection of CAS. They found that CDUS detected mild, moderate, and severe CAS in 26 %, 17,8 %, and 46 % of the examined vessels. Wardlaw et al.(33) conducted a meta-analysis involving 912 patients and 1704 arteries to compare different methods for the detection of CAS. They revealed that carotid DUS detected mild, moderate, and severe CAS in 20 %, 3 %, and 33,33 % of the examined vessels. Netuka et al.(30) examined 103 patients with carotid DUS and demonstrated that 2,9 % of the examined patients had mild CAS, 21,4 % suffered from moderate CAS, and 75,7 % showed severe CAS. Cassola et al.(34) performed a review that involved 15 articles and evaluated the efficiency of DUS for the detection of CAS. They found that CDUS detected mild and severe CAS in 46 % and 45,1 % of the examined vessels.
Jahromi et al.(35) demonstrated the specificity and sensitivity of DUS for the detection of CAS in its meta-analysis. For 1716 individuals, it demonstrated 88 % (CI, 76 % to 100 %) and 98 % (95 % CI, 97 % to 100 %) specificity and sensitivity for diagnosing stenosis of 50 % or greater, respectively. Among the 2,140 individuals, the specificity and sensitivity for identifying stenosis of 70 % or more were 94 % (CI, 88 % to 97 %) and 90 % (CI, 84 % to 94 %). Additionally, Wardlaw et al.(33) reported that the sensitivity of DUS in the diagnosis of mild, moderate, and severe carotid stenosis were 83 %, 36 %, and 89 %, respectively, and the specificity of DUS in the diagnosis of mild, moderate, and severe carotid stenosis were 84 %, 91 %, and 84 %, respectively. Cassola et al.(34) found that the sensitivity of DUS in the diagnosis of mild and severe carotid stenosis were 63 % and 85 %, respectively, and the specificity of DUS in the diagnosis of mild and severe carotid stenosis was 99 % and 98 %, respectively. All of these findings are consistent with our results.
Limitations
The results of this systematic review and meta-analysis are relevant to patients who may have suspected CAS along with neurologic complaints. However, due to the small number of involved studies, the results cannot be regarded as definitive. There was variability across the included studies, and many of them had a high or uncertain risk of bias. Most of the outcomes in the analysis were heterogeneous.
Contribution to the literature
The results of this analysis show that DUS can accurately distinguish between substantial CAS (< 50 % or 50 % to 99 %) and its absence. Consequently, there is proof in favour of DUS being the primary modality of choice for detecting CAS. Given the high value of sensitivity for this category, evidence suggests that in cases of DUS identifying > 50 % CAS, further imaging may not be required to detect the presence of CAS.
CONCLUSIONS
In conclusion, Duplex ultrasound is clearly an important exam in the identification of patients with symptomatic carotid stenosis. Understanding its complexities and limitations can improve clinical practice and provide cost-effective management for patients. Carotid DUS showed a high specificity and sensitivity in the diagnosis of CAS especially a severe degree of stenosis. Also, carotid DUS had a significantly higher rate of carotid sinus plaque detection. Therefore, to identify the type of carotid plaque, CDUS may be helpful for routine screening. Future studies should be conducted and include comparisons between different diagnostic methods such as MRA versus CTA or DUS.
BIBLIOGRAPHIC REFERENCES
1. Zhang X, Wan T-F, Chen J, Liu L. Tenecteplase versus alteplase for patients with acute ischemic stroke: a meta-analysis of randomized controlled trials. Aging (Albany NY) [Internet]. 2023;15(24):14889–99. Available from: http://dx.doi.org/10.18632/aging.205315
2. Saduakas AY, Kurakbayev KK, Baubekov AA. The benefits of duplex scanning of extracranial carotid pathologies for risk stratification of ischemic stroke. New Armen Med J [Internet]. 2023;31–5. Available from: http://dx.doi.org/10.56936/18290825-2023.17.f-31
3. de Jesus M, Maheshwary A, Kumar M, da Cunha Godoy L, Kuo C-L, Grover P. Association of electrocardiographic and echocardiographic variables with neurological outcomes after ischemic Stroke. Am Heart J Plus [Internet]. 2023;34(100313):100313. Available from: http://dx.doi.org/10.1016/j.ahjo.2023.100313
4. Saduakas AY, Shamshiyev AS, Kurakbayev KK, Matkerimov AZh, Tergeussizov AS, Zhakubayev MA, Baubekov AA. Modern organization aspects of the prevention of ischemic stroke in patients with extracranial carotid stenosis. Bull Surg Kaz. 2023;2:51-53. Available from: https://vhk.kz/wp-content/uploads/2023/05/8.pdf
5. Saduakas A, Shamshiyev A, Matkerimov A, Tergeussizov A, Demeuov T, Khanchi M, et al. Is screening for extracranial carotid stenosis effective in preventing ischemic stroke? Literature review. Bulletin of Surgery in Kazakhstan [Internet]. 2023;(1):4–4. Available from: http://dx.doi.org/10.35805/bsk2023i004
6. Hu S, Cai J, Chen S, Wang Y, Ren L. Identification of novel biomarkers and immune infiltration characteristics of ischemic stroke based on comprehensive bioinformatic analysis and machine learning. Biochem Biophys Rep [Internet]. 2024;37(101595):101595. Available from: http://dx.doi.org/10.1016/j.bbrep.2023.101595
7. Stepanova N, Korol L, Burdeyna O, Snisar L, Rysyev A, Filonov V, et al. Oxidative stress as the bridge between dyslipidemia and peritoneal ultrafiltration failure: A bi-center cross-sectional cohort study. Ukr J Nephrol Dial [Internet]. 2023;(4(80)):34–45. Available from: http://dx.doi.org/10.31450/ukrjnd.4(80).2023.05
8. Gleißner C, Kaczmarz S, Kufer J, Schmitzer L, Kallmayer M, Zimmer C, Wiestler B, Preibisch C, Göttler J. Hemodynamic MRI parameters to predict asymptomatic unilateral carotid artery stenosis with random forest machine learning. Front Neuroimaging [Internet]. 2023 Jan 12 [cited 2024 Apr 10];1. Available from: https://doi.org/10.3389/fnimg.2022.1056503
9. Low M, Gray B, Dicks A, Ochiobi O, Blas J, Gandhi S, Carsten C. Comparison of Complications and Cost for Transfemoral Versus Transcarotid Stenting of Carotid Artery Stenosis. Ann Vasc Surg [Internet]. 2022 Sep [cited 2024 Apr 10]. Available from: https://doi.org/10.1016/j.avsg.2022.08.014
10. Mohimen A, Gupta A, Gill S, Sahu S, Anadure R. Correlation of CT perfusion with MRI brain in symptomatic carotid artery stenosis. Med J Armed Forces India [Internet]. 2023;79(4):421–7. Available from: http://dx.doi.org/10.1016/j.mjafi.2022.04.003
11. Vostrotin O, Litovchenko T. Clinical and paraclinical features of psychopathological disorders in right hemisphere stroke. FM [Internet]. 2023 Sep. 30 [cited 2024 Apr. 10];2(3):29-40. Available from: https://futurity-medicine.com/index.php/fm/article/view/49
12. Tekieli L, Mazurek A, Dzierwa K, Stefaniak J, Kablak-Ziembicka A, Knapik M, et al. Misclassification of carotid stenosis severity with area stenosis-based evaluation by computed tomography angiography: impact on erroneous indication to revascularization or patient (lesion) migration to a higher guideline recommendation class as per ESC/ESVS/ESO/SVS and CMS-FDA thresholds. Postepy Kardiol Interwencyjnej [Internet]. 2022;18(4):500–13. Available from: http://dx.doi.org/10.5114/aic.2023.125610
13. Sharma K, Blaha MJ, Blumenthal RS, Musunuru K. Clinical and research applications of carotid intima-media thickness. Am J Cardiol [Internet]. 2009;103(9):1316–20. Available from: http://dx.doi.org/10.1016/j.amjcard.2009.01.020
14. Masley SC, Masley LV, Gualtieri CT. Cardiovascular Biomarkers and Carotid IMT Scores as Predictors of Cognitive Function. J Am Coll Nutr [Internet]. 2014 Feb [cited 2024 Apr 10];33(1):63-9. Available from: https://doi.org/10.1080/07315724.2014.870010
15. Mitsuhashi N, Tanaka Y, Kubo S, Ogawa S, Hayashi C, Uchino H, et al. Effect of Cilostazol, a Phosphodiesterase Inhibitor, on Carotid IMT in Japanese Type 2 Diabetic Patients. Endocr J [Internet]. 2004;51(6):545-50. Available from: http://www.jstage.jst.go.jp/article/endocrj/51/6/51_6_545/_article
16. Martinelli O, Alunno A, Drudi FM, Malaj A, Irace L. Duplex ultrasound versus CT angiography for the treatment planning of lower-limb arterial disease. J Ultrasound [Internet]. 2021 Dec 9;24(4):471–9. Available from: https://link.springer.com/10.1007/s40477-020-00534-y
17. Piotin M, Gailloud P, Bidaut L, Mandai S, Muster M, Moret J, et al. CT angiography, MR angiography and rotational digital subtraction angiography for volumetric assessment of intracranial aneurysms. An experimental study. Neuroradiology [Internet]. 2003 Jun 1;45(6):404–9. Available from: http://link.springer.com/10.1007/s00234-002-0922-8
18. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Ítems de referencia para publicar Revisiones Sistemáticas y Metaanálisis: La Declaración PRISMA. Rev Esp Nutr Humana Diet [Internet]. 2014;18(3):172–81. Available from: http://dx.doi.org/10.14306/renhyd.18.3.114
19. EndNote - the best citation & reference management tool [Internet]. EndNote. 2023 [cited 2024 Apr 10]. Available from: https://endnote.com/
20. Katz A. Microsoft Excel 2010. Style (DeKalb, IL). 2010
21. Pearson GD, Mensah GA, Rosenberg Y, Stoney CM, Kavounis K, Goff DC. National Heart, Lung, and Blood Institute cardiovascular clinical trial perspective. Am Heart J [Internet]. 2020;224:25–34. Available from: http://dx.doi.org/10.1016/j.ahj.2020.02.014
22. Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ [Internet]. 2011;343(oct18 2):d5928. Available from: http://dx.doi.org/10.1136/bmj.d5928
23. Saxhaug LM, Graven T, Olsen Ø, Kleinau JO, Skjetne K, Ellekjær H, et al. Reliability and agreement of point-of-care carotid artery examinations by experts using hand-held ultrasound devices in patients with ischaemic stroke or transitory ischaemic attack. Open Heart [Internet]. 2022;9(1):e001917. Available from: http://dx.doi.org/10.1136/openhrt-2021-001917
24. Wallace BC, Lajeunesse MJ, Dietz G, Dahabreh IJ, Trikalinos TA, Schmid CH. Open MEE : Intuitive, open-source software for meta-analysis in ecology and evolutionary biology. Poisot T, editor. Methods Ecol Evol. 2017;8(8):941–7.
25. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Handbook for Systematic Reviews of Interventions. 2019.
26. Woo EY, Dearing J. Carotid artery stenosis. Vasc Endovasc Rev [Internet]. 2019;2(1):40–4. Available from: http://dx.doi.org/10.15420/ver.2018.14.2
27. Saxena A, Ng EYK, Lim ST. Imaging modalities to diagnose carotid artery stenosis: progress and prospect. Biomed Eng Online [Internet]. 2019;18(1):66. Available from: http://dx.doi.org/10.1186/s12938-019-0685-7
28. Mostafa S, Shabana H, Khalil F, Mancy IME, Zedan HA-M, Elmoursi A, et al. Evaluation of the safety and efficacy of dual therapy perindopril/amlodipine in the management of hypertension. A systematic review and meta-analysis. High Blood Press Cardiovasc Prev [Internet]. 2022;29(6):565–76. Available from: http://dx.doi.org/10.1007/s40292-022-00544-3
29. Gaisenok OV, Samorodskaya IV, Drapkina OM. Can a referral diagnosis code for duplex ultrasound “predict” carotid artery stenosis? Cardiovasc Ther Prev. 2023 May;22(4):3432.
30. Netuka D, Ostrý S, Belšán T, Ručka D, Mandys V, Charvát F, et al. Magnetic resonance angiography, digital subtraction angiography and Doppler ultrasonography in detection of carotid artery stenosis: a comparison with findings from histological specimens. Acta Neurochir (Wien) [Internet]. 2010;152(7):1215–21. Available from: http://dx.doi.org/10.1007/s00701-010-0645-2
31. Sydorenko T. Critical Evaluation of Modern Strategies and Methods of Formation of Communicative Competency in the System of Continuing Education of Document Managers. FSocS [Internet]. 2024 Feb. 19 [cited 2024 Apr. 10];2(1):28-55. Available from: https://futurity-social.com/index.php/journal/article/view/12
32. Zavanone C, Ragone E, Samson Y. Concordance rates of Doppler ultrasound and CT angiography in the grading of carotid artery stenosis: a systematic literature review. J Neurol. 2012 Jun;259(6):1015-8.
33. Wardlaw JM, Chappell FM, Best JJK, Wartolowska K, Berry E, NHS Research and Development Health Technology Assessment Carotid Stenosis Imaging Group. Non-invasive imaging compared with intra-arterial angiography in the diagnosis of symptomatic carotid stenosis: a meta-analysis. Lancet [Internet]. 2006;367(9521):1503–12. Available from: http://dx.doi.org/10.1016/S0140-6736(06)68650-9
34. Cassola N, Baptista-Silva JC, Nakano LC, Flumignan CD, Sesso R, Vasconcelos V, et al. Duplex ultrasound for diagnosing symptomatic carotid stenosis in the extracranial segments. Cochrane Database Syst Rev [Internet]. 2022;7(7):CD013172. Available from: http://dx.doi.org/10.1002/14651858.CD013172.pub2
35. Jahromi AS, Cinà CS, Liu Y, Clase CM. Sensitivity and specificity of color duplex ultrasound measurement in the estimation of internal carotid artery stenosis: a systematic review and meta-analysis. J Vasc Surg [Internet]. 2005;41(6):962–72. Available from: http://dx.doi.org/10.1016/j.jvs.2005.02.044
36. Barlinn K, Floegel T, Kitzler HH, Kepplinger J, Siepmann T, Pallesen L-P, et al. Multi-parametric ultrasound criteria for internal carotid artery disease—comparison with CT angiography. Neuroradiology [Internet]. 2016;58(9):845–51. Available from: http://dx.doi.org/10.1007/s00234-016-1706-x
37. Cui H, Liu Q, Wu Y, Cao L. Cumulative triglyceride-glucose index is a risk for CVD: a prospective cohort study. Cardiovasc Diabetol [Internet]. 2022;21(1):22. Available from: http://dx.doi.org/10.1186/s12933-022-01456-1
38. Li YL, Qiu D, Hu C, Ouyang FY, He J, Zang DF, Luo D, Xiao SY. Stressful life events and poor sleep quality: a cross-sectional survey in the Chinese governmental employees. Sleep Med [Internet]. 2021 Sep [cited 2024 Apr 10];85:123-30. Available from: https://doi.org/10.1016/j.sleep.2021.06.030
39. Shehata ZH, Rabea H, El Sherif R, Abdelrahim ME, Dawoud DM. Estimating Societal Cost of Illness and Patients’ Quality of Life of Duchenne Muscular Dystrophy in Egypt. Value Health Reg Issues [Internet]. 2023 Jan [cited 2024 Apr 10];33:10-6. Available from: https://doi.org/10.1016/j.vhri.2022.08.006
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Almas Saduakas, Kuralbay Kurakbayev.
Data curation: Yenglik Askar, Mairash Baimuratova.
Formal analysis: Kuralbay Kurakbayev, Mairash Baimuratova.
Research: Almas Saduakas, Yenglik Askar.
Methodology: Kuralbay Kurakbayev, Almas Saduakas.
Project management: Yenglik Askar.
Software: Mairash Baimuratova.
Supervision: Almas Saduakas.
Validation: Kuralbay Kurakbayev, Yenglik Askar.
Display: Yenglik Askar.
Drafting - original draft: Almas Saduakas, Kuralbay Kurakbayev.
Writing - proofreading and editing: Almas Saduakas, Kuralbay Kurakbayev.