ORIGINAL ARTICLE
Identifying Noise Sources & Alarm Hazards in ICUs – Occurrences. Tools to Minimize
Identificación de fuentes de ruido y riesgos de alarma en las UCI: ocurrencias; herramientas para minimizarlos
Swetapadma Dash1,2
![]() *
*
1Siksha ‘O’ Anusandhan. Bhubaneshwar, India.
2Sum Ultimate Medicare. Bhubaneswar, India.
Cite as: Dash S. Identifying Noise Sources & Alarm Hazards in ICUs – Occurrences. Tools to Minimize. Salud Cienc. Tecnol. 2022;2(S2):236. https://doi.org/10.56294/saludcyt2022236
Submitted: 01-11-2022 Revised: 04-12-2022 Accepted: 22-12-2022 Published: 31-12-2022
ABSTRACT
ICU of a hospital is considered to be one of the most stressful and psychologically taxing working places because of the congregation of critically ill and severely injured patients. Patients with any life-threatening illnesses are admitted to the intensive care unit. The objective of ICUs is to assist such patients duly recover by providing them advanced treatment with the skillful application of advanced techniques. ICU is also a place where sophisticated equipment and machinery necessary to supervise and care for a seriously ill patient are strung together to meet the treatment needs of patients without the possibility of neglecting them. Part of the ICU architecture is medical device alarms. Clinical devices and other appliances sound hundreds of alarms per patient per day, creating a dissonance that can overwhelm, distract, and desensitize health care workers as well as patients. The hazards related to excessive noise and clinical alarms were conceived as a project when it was observed that the stress level of patients and care givers increased due to the noise coming out of these alarm systems. A study undertaken in one of the multispecialty Hospitals in Bhubaneswar to find out the possible sources of stress revealed that noise from alarms and other sources were proving to be a source of a hindrance for effective communication and contributing to patients’ stress. The results of our study indicate that behavioral modification alone is not adequate to control excessive noise. There is a need for further research involving the supportive involvement by clinicians, nurses, and paramedic and support staffs, along with effective medical device alarm management, and continuous process improvement methods and training.
Keywords: Psychological Factors; Intensive Care Unit; Stressors; Health Care Organization; Alarm Hazards; Medical Devices.
RESUMEN
La UCI de un hospital se considera uno de los lugares de trabajo más estresantes y psicológicamente agotadores debido a la congregación de pacientes en estado crítico y gravemente heridos. Los pacientes con enfermedades potencialmente mortales ingresan en la unidad de cuidados intensivos. El objetivo de las UCI es ayudar a estos pacientes a recuperarse debidamente proporcionándoles un tratamiento avanzado con la hábil aplicación de técnicas avanzadas. La UCI es también un lugar donde se reúnen los sofisticados equipos y maquinaria necesarios para supervisar y atender a un paciente gravemente enfermo, con el fin de satisfacer las necesidades de tratamiento de los pacientes sin posibilidad de descuidarlos. Parte de la arquitectura de la UCI son las alarmas de los dispositivos médicos. Los dispositivos clínicos y otros aparatos hacen sonar cientos de alarmas por paciente y día, creando una disonancia que puede abrumar, distraer e insensibilizar tanto a los trabajadores sanitarios como a los pacientes. Los peligros relacionados con el ruido excesivo y las alarmas clínicas se concibieron como proyecto cuando se observó que el nivel de estrés de pacientes y cuidadores aumentaba debido al ruido que emitían estos sistemas de alarma. Un estudio realizado en uno de los hospitales multiespecialidad de Bhubaneswar para averiguar las posibles fuentes de estrés reveló que el ruido de las alarmas y otras fuentes obstaculizaba la comunicación eficaz y contribuía al estrés de los pacientes. Los resultados de nuestro estudio indican que la modificación del comportamiento por sí sola no es adecuada para controlar el ruido excesivo. Es necesario seguir investigando con la participación de médicos, enfermeras y personal paramédico y de apoyo, junto con una gestión eficaz de las alarmas de los dispositivos médicos y métodos y formación para la mejora continua de los procesos.
Palabras clave: Factores Psicológicos; Unidad de Cuidados Intensivos; Factores de Estrés; Organización Sanitaria; Alarma de Peligros; Dispositivos Médicos.
INTRODUCCIÓN
The field of healthcare is inherently stressful because of the criticality of the cases and the high risk involved; where patients' lives are on the line and death is always a possibility.(1) While for patients and their families, hospitalization brought on by a severe illness is seen as a crisis.(2)
The uncertainties of the ICU environment because of the congregation of severely ill patients represent a challenge that is exhausting and confronting in equal measure. For the patients, the ICU is both a resort of hope and a place of concern because of multiple physical, psychological, and environmental stressors are involved.(3)
The intensive care unit is part of critical care medicine, which provides specialized care to critically ill patients with complex medical problems to sustain physiologic life. It is a part of the hospital that is dedicated to the treatment of patients with life-threatening illnesses and requires critical care. It involves a broad range of interventions, close observation and monitoring by sophisticated medical equipment and treatment by a team of specially trained doctors and nurses who specialize in intensive care.(4)
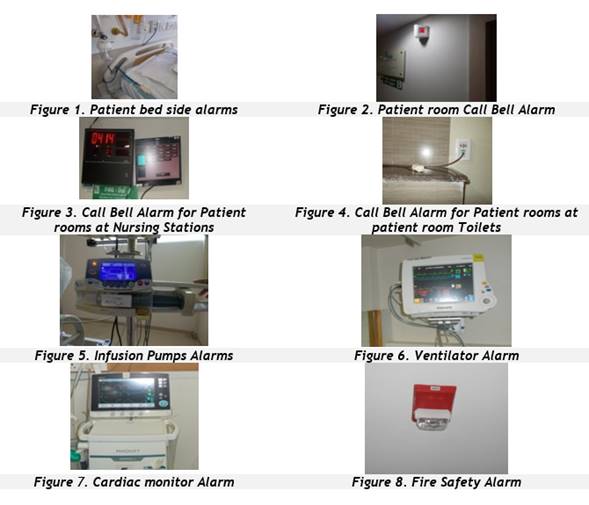
A cursory look around a hospital for clinical alarms and medical systems with alarms would reveal how widespread the use of alarm-based medical devices is, and about the dependence of the healthcare system on medical alarm systems to improve efficiency.
The usage of medical alarm systems has a significant leap in the ICU, where typically a patient has nearly a dozen medical devices with alarms attached to his person. The feel and atmosphere of critical care units have a cadence of their own. The physical environment of an ICU replete with strange and unfamiliar buzzing sounds, continuous bright lighting, noise emanating from respiratory aids, vital sign check monitors and equipment’s together represent an overwhelming array of stimuli that is unreal and unsettling.(5)
The atmosphere in an ICU is anything but tranquil and comforting that is necessary for a patient to recuperate from a critical illness.(6)
The risk of clinical alarms has continued long enough to be recognized as a key patient safety issue. The healthcare hazards of alarm fatigue have been widely researched and the occurrence of adverse alarm related incidents was far too common to warrant acknowledgement of alarm hazard as a healthcare technology safety concern and a threat to patient safety. "Alarm Fatigue" has been listed as the fifth-greatest healthcare hazard in ECRI Institute's 2020 report for Top 10 Health Technology Hazards.(7)
While on one hand alarm hazards have become a major patient safety concern with Alarm fatigue from medical alarm devices having potentially deadly consequences, high noise levels in the ICU have also emerged as source of stress and a cause for concern. The decibel levels of noise in the ICU have been found to exceed the World Health Organization recommended level of 30 decibels for the hospitals and the Environmental Protection Agency’s recommended decibel levels of 45 during the day and 30 at night for the ICU.(8)
When patients are exposed to a steady drone of auditory stimuli from different sources in the ICU, it sets off a permanent alarm in the body and creates sleep disturbances which affect the endocrine and cardiovascular systems and causes enormous stress to the patients adversely affecting their health. Wenham & Pittard(9) have highlighted that decibels levels often exceed 60 in the ICU, which is on par with the noise produced by a standard vacuum cleaner and is recognized as a source of noise-induced stress for patients.
To date, most studies have centered on the effects of alarm fatigue on ICU caregivers. The sources of noise and the effects of noise emanating from medical alarm devices on ICU patients have not received widespread attention in research.
This study aims to identify the sources of noise in the ICU, the hazards they present the effect it has on the patients and propose strategies to improve medical devise alarms safety bring efficiencies in alarm management and minimize risk and improve patient safety.
Review of literature
A study highlights that attention deficit and lack of observation on the part of the healthcare provider to detect changes in the patient's condition can be the reason for many ICU accidents.(10) To enhance patient safety in the ICU, monitoring systems were devised to measure patient variables and, subsequently, alarm systems were added to draw the attention of caregivers if the patient variables were below or beyond acceptable levels.
In another study it is pointed out that many problems have been reported in the critical care areas of the hospital, especially the ICU and the operating rooms regarding auditory warnings.(11) They note that there is a suffusion of medical device systems alarms in the ICU and the constant and loud alarm tones have been deemed vexing by the care giving staff.
The problem is further accentuated by the lack of standard agreement between manufacturers on the auditory warnings used for medical equipment. This usually translates into the same piece of medical device producing different alarms because they have different manufacturers. Adding to the confusion is the incongruity of alarm systems in terms of urgency mapping, i,e the acoustic urgency of the alarms was not always linked to the clinical urgency of the situation. This leads to increased numbers of false alarm rates and low response levels because of a lack of trust or perceived unreliability of the alarms system by the user.
The problem of high false alarms has been cited by Carrol who contends that the presence of high numbers of alarms and the rate of false alarms makes it tough for the caregivers to locate the alarm source amidst a bevy of high-pitched systems like, infusion pumps, ventilators, and also distinguish the important ones that require an immediate response.(12)
To deal with typical alarm-related problems and alarmfatigue, nurses have been known to silence alarms or unsafely modify alarm settings to counter alarm overload.(13)
Modifying alarm settings or turning them off and then forgetting to activate the electronic monitor to signal the next crisis led to the death of a patient.(14)
ICU alarms should never be turned off. Instead, significant efforts should be made to improve alarm safety and reduce alarm nuisance by reviewing alarm-based technologies and processes, the hospital's clinical alarm protocols and the response of clinical users.
Noise, simply put, is defined as unwanted sounds having both psychological and physiological implications for people.(15)
explains that people's response to noise is determined by its decibel levels or loudness, what the noise represents and personal sensitivity levels; with loudness being a function of sound intensity and frequency.(16)
There it is further described that frequency as pitch, expressed in cycles per second, and that sound intensity is measured in decibels [dB] on an exponential scale. The World Health Organization (WHO) recommends that the average background noise in hospitals wards should not exceed 30 A weighted decibels (dB[A]), with night-time limits not exceeding 40 dB(A).(17) 35 decibels of noise and less is considered appropriate for sleeping and noise levels in the ICU should not exceed fifty decibels (50 dB(A)).(18)
One of the studies also have determined that there is a profusion of environmental noise in the ICU from alarms, movement of people and objects, people talking or laughing, coughing patients, telephones, computer printers, and mechanical equipment that adds to the noisiness of the space with potential interference in speech and sleep disturbances because of the increased stimuli from unwanted sounds.(19)
Noise is also referred as acting as a hindrance to optimal care by acting as a barrier to verbal communication among caregivers. They also reported that environmental noise could also be a stress factor for nurses, resulting in deficient attention and hampered efficiency.
The impact of the application of automated human voice delivery to warning devices has also been explained in earlier studies where it has been found that the patients perceived the conventional non-verbal signal as threatening.(20)
Sleep disturbance is a regular problem for ICU patients as the noise levels range from 50 to 75 dBA, reaching a peak level of 103 dBA at night.(21)
The effect of noise on the quality of sleep of ICU patients was studied and it was confirmed the adverse consequences of noise on the sleep quality in ICU patients and advocating strengthening the usefulness of noise-mitigation strategies.(19)
It has also have been found out that the negative influence of noise on patients' sleep in ICU includes cardiovascular stimulation, hearing loss, increased gastric secretion, pituitary and adrenal gland stimulation, and suppression of the immune response to infection.(22)
METHODS
The ICU in-patients of a 350-bed multi-speciality Corporate Hospital at Bhubaneswar were the subjects of the study. Only adult patients above the age of 18 admitted to ICU were included as subjects for the study. Informed consent was obtained in all cases.
The study includes both qualitative and quantitative methods because the approach provides a comprehensive understanding and ensures the outcomes that were apparent in the study involving intense human emotions revealed through interaction is accounted for and not limited to numerical data and statistics.(23)
Additionally, the mixed model approach helped provide an enhanced understanding of data by drawing meaningful and defensible inferences on the meanings, intentions, context, and consequences of the collected data.
The questionnaire for the patients was based on studies conducted for Hospital stress items by Volicer(24) and further studies conducted in the ICU settings by Ballard.(25) The questionnaire was in bilingual English and Odia.
The responses from the study subjects on the administered questionnaires were analyzed on a 5-point scale. This formed the basis for quantitative analysis. The respondent's versions, expressions, gestures, and postures were duly recorded for qualitative analysis.
The first stage (Stage -I) of the study was a pilot study of two weeks, where thirty minutes of intense personal interactions were held to collect an in-depth understanding of different aspects of patients’ experiences in the ICUs and their perceptions of the items of the questionnaires. This helped in the development of the study instrument which was an adaptation of the English VolicerTest.
In Stage II, it was item analyzed to retain the required items in the questionnaire.
Stage III was the pre-intervention data collection where the revised adopted study instruments were administered.
The revised adopted study instruments comprising 50 items were administered to 125 patients to identify and understand the source and nature of stress faced by them in the ICU.
Stage- IV involved the implementation of the devised plan of action to manage and counter the stress experienced by the ICU patients who formed the subjects of the study.
Stage –V describes the post-intervention data collected to understand the efficacy of the measures implemented.
RESULT AND DISCUSSION
In the study undertaken on the patients of the ICUs, who volunteered as subjects, to identify the possible sources of stress in stage III, it was revealed that noise from alarms and other sources were proving to be a source of a hindrance to effective communication and contributing to patients’ stress.
Based on these findings as discussed in the above paragraphs, an action plan was developed and implemented, in accordance with the priorities, hospital's mission & vision, hospital standardized policies, financial concurrence, human commitment and with the approval of the Head of the Unit.
Stage III: Response of ICU patients to the questionnaire on item No. 4:
The psychological item listed number 4 in the questionnaire on which the stress level of the patients was assessed was found to be having a disturbing effect on the respondents.
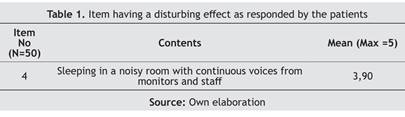
Table 1 represents the response of patients on the item number one. Sleeping in a noisy room with continuous voices from monitors and staff was responded as stressful by 69,60 % of patients out of which 36,80 % of patients found it as slightly stressful. This Item is a validated source of stress in the hospital ICUs.(24)
Interaction with the patients revealed that during third to seventh day of their hospitalization in ICU, they found this item to be highly stressful. Such a stressful experience can also lead to ICU psychosis which is said to occur on third day of illness and admission to the ICU.
The hospital care comes with the cost of privacy and more so when a patient is admitted in an ICU. Patient has to share the space with other patients and the continuing noise from the ICU apparatus, the nurses might also be a point of stress.
The qualitative experiences from the interactions held with the ICU patients revealed a lot of facets.
"The beeping of the monitors is disrupting my sleep more than the sounds of human voices. I can't sleep and it is irritating," said a visibly disturbed patient.
An ICU is steaming with plenty of highly sophisticated medical equipment which has a sound of its own along with its beeps and alarms so there is constant noise emanating from these equipments. The nursing staffs in charge of ICUs can also contribute to the noise levels whenever they are discussing among themselves or attending to other patients. All this chatter or beeping noise might be a source of disturbance to the patients.
"I have a weak heart and sounds frighten me in current physical and psychological conditions. The machines in these rooms keep making strange noises. They keep beeping and buzzing and it is throughout the day," said a patient complaining about the noise levels in the room.
Another patient said, "I find it hard to get sleep here and whenever I do manage some sleep the telephone in the room buzzes or the nurses are chatting. The beeps from machines go off intermittently interrupting my sleep," said a tired-looking patient”.
Another patient said, "I find hard to get sleep here and whenever I do manage some sleep the telephone in the room buzzes or the nurses are chatting.”
He isn't alone in his frustration. Another patient said, "Noise levels are disturbing and upsetting, most of the noise generated by rowdy staff and large groups of visitors that had no care or concern about anyone else in the hospital. I hope the hospital starts disciplining their staff and enforcing quiet zones on ICU floors."
“The beeps from machines go off intermittently interrupting my sleep," said a tired-looking patient.
Stage IV: Action Plan Implementation
The information that emerged from stage III became the subject of intense debate and discussion. The brainstorming sessions took into account patients as stakeholder, management, consultants and patients and their attendants who had been in the hospital for a considerable length of time.
These sessions threw up some very interesting insights which formed the core of the action plan that were devised to mitigate the effects of stress and to reduce the incidents of stress in the ICUs. The action plan implemented also focused on strengthening the activities that the stakeholders found to be highly or slightly reassuring or important for them, along with devising countervailing measures to compensate the effects of highly or slightly stress inducing items. The implementation of action plan is spread out over a period of two years and the measures that prove to be effective shall be adopted and sustained into the future.
Stage IV: Action Plan Implementation
To offset the stress that was due to the noisy rooms, and to avert the harmful effect of stress arising out of undesirable levels of noise a project named “SHHH Project” (Silence Hospital Helps Healing Project) was undertaken to check and manage the decibel levels on the hospital premises and to create noise free zone at patient care areas. Along with this, the staffs were educated on observing silence inside ICUs. Visitors were also made to participate in the SHHH initiative as a stakeholder and were asked to support and observe silence while visiting their patients inside ICUs. Education brochures were displayed across the hospital to give a visual illustrate about this program. Signage like “maintain silence please”, “please switch off your mobiles”, “your speaking hurts” etc were displayed at patient waiting areas and other important areas where silence is a necessity as a message for the patients to extend their co-operation in maintaining a silence zone.

Figure 1. ‘SHHH Project”: Silence Hospital Project taken up to create Silent environment for patients and to facilitate faster healing; messages displayed across the hospital
The figure 1 shows the message displayed at various strategic location in the hospital as a reminder for staffs to follow creating a silent environment for patients. The crux of the program included educating hospital staff about the harmful effect of noise and requesting them to maintain the minimum levels of voice while communicating with each other. The staffs were asked to keep their mobile in silent mode while at work.
To reduce the stress due to non-availability of medium of entertainment like TV, radio and also the newspapers, management called for a meeting of ICU Consultants and other staffs working in ICUs. It was concluded from the discussion that this result is derived from the responses of only those patients, who are conscious, oriented and can read because most of the patients in ICUs are critical or on ventilator or disoriented. Hence, a TV would only add to the problem of noise pollution or addition instead of providing entertainment or distraction. A decision was taken in favor of newspaper to make them available to patients who are conscious and are interested in reading paper on their own.
The hospital has been operational for the last 10 years and most of the machineries and equipments like trolleys, wheelchairs, stretchers etc have undergone wear and tear. These emanate noises that could have been the reason for bringing about stress in patients. The waiting area is adjoining the ICUs where attendants wait on information for the patients. It has been observed that an increase in the no. of visitors in the waiting area makes the place crowded and noises which might have been the source of stress for the patients in ICU.
The ongoing maintenance and repair work in the ICUs and the areas nearby might also bring about a feeling to the patients in ICUs that the ICUs are noisy.
For reducing the noise level of the Alarm systems; Health care workers/ nursing staffs were educated on the equipment management to keep them alert. They were further educated and trained on how to reduce the noise level of these equipments.
Noises emanating from the squeaky wheels, trolleys equipments, machines, wheels and doors which could be repaired were promptly assigned to the maintenance department and those which were beyond repair were replaced with the new acquisitions.
Chart 2. Alarms present in the system and are sufficiently audible with respect to distances and competing noise within the unit (Nursing Station)
Source: Own elaboration.
Stage V: response of ICU patients post intervention for item No.4
The post intervention data collection period is necessitated to assess the impact of action plan implemented, by analyzing the change in the perceptions of the stake holders, post the implementation of the action plan. This exercise enabled to develop an understanding of the efficacy of the plan and to come out with suggestions or recommendations that can make the ICU Patient’s comfortable with their hospital stay. The impact of the interventions was assessed by administering a paired t –test. The result is as follows (Table 2).
Table 2. Depicts the mean and percentage of the responses of patients for the parameter – Sleeping in a noisy room with continuous voices from monitors and staff in Pre and post intervention stages
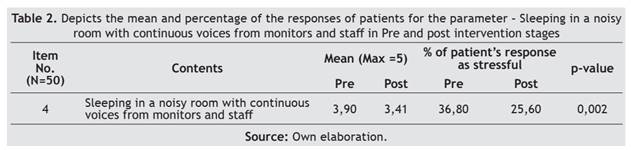
The analysis of the data for the post intervention period focused on understanding the efficacy of the action plan implemented. On analyzing the responses to the administered questionnaires in this period of study, it was revealed that the action plan implemented have worked towards alleviating effect of the item no. 4 that had stressful effect for the patient in the pre intervention period.
The comparative data for the pre and post intervention period highlight a positive net effect that can be very much substantiated by the P- Values. This conveys the stress has been significantly countered by the measures put in place in the action plan implementation stage. The action plan implemented had a positive impact as evident by respondent’s view in the post intervention period.
CONCLUSION
In the current scenario where, increasing emphasis is being laid on comprehensive care and holistic treatment for the patients that include in its ambit the wellbeing of the patient, attendants and the care givers, this study is a case for deep engagements and interactions for a comprehensive understanding of the patient’s experiences in ICUs. For the period this study was alive, it covered vast activities and, in the process, identified the existing gaps in the ICU noise management, devised interventional strategies, action plan was implemented that yielded positive results in the perception of ICU experiences of patients regarding the parameter- “Sleeping in a noisy room with continuous voices from monitors and staff”. It highlighted the importance of considering qualitative approach towards understanding the different experiences, perceptions of patients. Since humans are in the Centre of all health care activities, more time devoted to understanding the many facets of human well-being would contribute a great deal in reducing the stress that envelops the Patients and other stakeholders. This study focuses on clearly identifiable and discernible dimensions which is changed and shown to make a change.
The project stands out for its comprehensiveness and differentiates itself because of the detailed work that was undertaken where even the minute parts were accounted for. Noise is a source of stress but the sources of it at ICU, contribution of alarms and alarm induced distraction and stresses have not been given required importance. This study went in depth, identified the alarm issues, and deployed measures that limited the alarms from turning alarming. If proof of the pudding is in the eating, then the positive results speak for themselves. The uniqueness and the extent of success of the measures implemented make this research a starting point for other researches to build on in their effort to improve the ICU experiences and mitigate the attendant ICU stressors.
BIBLIOGRAPHIC REFERENCES
1. Riegel B, Ehrenreich D. Psychological aspects of critical care nursing. Rockville, Md.: Aspen Publishers; 1989.
2. Molter NC. Needs of relatives of critically ill patients: a descriptive study. Heart Lung 1979;8:332–9.
3. Blacher RS. The psychological and psychiatric consequences of the ICU stay. Eur J Anaesthesiol Suppl 1997;15:45–7. https://doi.org/10.1097/00003643-199705001-00009.
4. Srivastava M. Planning And Design Considerations Of ICU. Technichal Paper SHAPE 95 Section II; 1995.
5. Malkin J. Hospital Interior Architecture: Creating Healing Environments for Special Patient Populations. New York: Jon Wiley Sons; 1992.
6. Putsep E. Modern hospital: international planning practices. London: Lloyd-Luke; 1979.
7. Miliard M. ECRI’s top health tech hazards for 2020 include EHR errors, alert fatigue, missing MRI data. Healthcare IT News 2019. https://www.healthcareitnews.com/news/ecris-top-health-tech-hazards-2020-include-ehr-errors-alert-fatigue-missing-mri-data
8. Kahn DM, Cook TE, Carlisle CC, Nelson DL, Kramer NR, Millman RP. Identification and modification of environmental noise in an ICU setting. Chest 1998;114:535–40. https://doi.org/10.1378/chest.114.2.535.
9. Mistraletti G, Umbrello M, Anania S, Andrighi E, DI Carlo A, Martinetti F, et al. Neurological assessment with validated tools in general ICU: multicenter, randomized, before and after, pragmatic study to evaluate the effectiveness of an e-learning platform for continuous medical education. Minerva Anestesiol 2017;83:145–54. https://doi.org/10.23736/S0375-9393.16.11103-4.
10. Sykes MK, Vickers MD, Hull CJ. Principles of measurement and monitoring in anaesthesia and intensive care. London: Blackwells; 1991.
11. Meredith C, Edworthy J. Are there too many alarms in the intensive care unit? An overview of the problems. J Adv Nurs 1995;21:15–20. https://doi.org/10.1046/j.1365-2648.1995.21010015.x.
12. O’Carroll TM. Survey of alarms in an intensive therapy unit. Anaesthesia 1986;41:742–4. https://doi.org/10.1111/j.1365-2044.1986.tb12844.x.
13. The hazards of alarm overload. Keeping excessive physiologic monitoring alarms from impeding care. Health Devices 2007;36:73–83.
14. Kowalczyk L. MGH death spurs review of patient monitors. The Boston Globe 2010.
15. Kang J. Urban Sound Environment. London: CRC Press; 2006. https://doi.org/10.1201/9781482265613.
16. Khanna A. A study of Intensive Care facilities in Command Hospital, Ruby Hall and Sassoon General Hospital. Pune: University of Poona; 1993.
17. Berglund B, Lindvall T, Schwela DH, Team WHOO and EH. Guidelines for community noise. Geneva: World Health Organization; 1999.
18. Qutub HO, El-Said KF. Assessment of ambient noise levels in the intensive care unit of a university hospital. J Family Community Med 2009;16:53–7.
19. Simons KS, Verweij E, Lemmens PMC, Jelfs S, Park M, Spronk PE, et al. Noise in the intensive care unit and its influence on sleep quality: a multicenter observational study in Dutch intensive care units. Crit Care 2018;22:250. https://doi.org/10.1186/s13054-018-2182-y.
20. McIntyre JWR, Nelson TM. Application of automated human voice delivery to warning devices in an intensive care unit: A laboratory study. J Clin Monit Comput 1989;6:255–62. https://doi.org/10.1007/BF01733631.
21. Al-Samsam RH, Cullen P. Sleep and adverse environmental factors in sedated mechanically ventilated pediatric intensive care patients. Pediatr Crit Care Med 2005;6:562–7. https://doi.org/10.1097/01.pcc.0000165561.40986.a6.
22. Snyder-Halpern R. The effect of critical care unit noise on patient sleep cycles. CCQ 1985;7:41–51.
23. Buemi M, Allegra A, Grasso F, Mondio G. Noise pollution in an intensive care unit for nephrology and dialysis. Nephrol Dial Transplant 1995;10:2235–9. https://doi.org/10.1093/ndt/10.12.2235.
24. Volicer BJ, Isenberg MA, Burns MW. Medical-surgical differences in hospital stress factors. J Human Stress 1977;3:3–13. https://doi.org/10.1080/0097840X.1977.9936082.
25. Ballard KS. Identification of environmental stressors for patients in a surgical intensive care unit. Issues Ment Health Nurs 1981;3:89–108. https://doi.org/10.3109/01612848109140863.
CONFLICTS OF INTEREST
None.
FINANCING
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Swetapadma Dash.
Methodology: Swetapadma Dash.
Writing - Original Draft: Swetapadma Dash.
Writing - Review & Editing: Swetapadma Dash.