REVIEW
VERSION 2: PEER REVIEW - APPROVED
Cannabis as a precursor of psychosis and its relationship with schizophrenia
El cannabis como precursor de la psicosis y su relación con la esquizofrenia
Roberto Carlos Mora Vera1 ![]() *, Rosa Solorzano1
*, Rosa Solorzano1 ![]() *, Jorge Andrés Lozano Aveiga1
*, Jorge Andrés Lozano Aveiga1 ![]() *, Byron Enrique Peña
Cordero1
*, Byron Enrique Peña
Cordero1 ![]() *
*
1Universidad Católica de Cuenca. Carrera de Medicina-Campus Cuenca. Cuenca, Ecuador.
Cite as: Mora Vera RC, Solorzano R, Lozano Aveiga JA, Peña Cordero BE. El cannabis como precursor de la psicosis y su relación con la esquizofrenia. Salud Cienc. Tecnol. 2022; 3:262. https://doi.org/10.56294/saludcyt2023262
Received: 01-23-2023 Revised: 02-18-2023 Accepted: 02-21-2023 Published: 02-03-2023 (Version 1); 02-22-2023 (Version 2)
Editor: Dr.
Adrián Alejandro Rojas Concepción ![]()
ABSTRACT
Introduction: schizophrenia is a chronic mental disease affecting around 24 million people worldwide. Within this disease, it is common to find the consumption of psychoactive substances by patients, with cannabis ranking first on the list; this drug bears a particular relation to schizophrenia through the effects of the cannabinoids proper to that plant.
Objective: determine the relationship between the consumption of cannabis and schizophrenia.
Methodology: a narrative bibliographic review was performed to find information using databases such as Scopus and PubMed with descriptors MESH/DECS via keywords, taking into account articles from 2009 to 2023, in English and Spanish and with criteria of inclusion and exclusion of the articles to be analyzed.
Results: it was assessed that cannabis consumption could trigger a psychotic episode in vulnerable individuals; the transition to psychosis was found to occur among those who started to consume cannabis before being 15 years old and continued consuming it frequently. Cannabis consumers were not more prone to develop psychosis than those who had never consumed cannabis.
Conclusions: cannabis consumption is one of the most important modifiable risk factors in the development of psychosis since it works as a componential cause for the outcome of a psychotic event framed within the spectrum of schizophrenia.
Keywords: Schizophrenia; Cannabis Sativa; Tetrahydrocannabinol; Cannabidiol.
RESUMEN
Introducción: la esquizofrenia es una enfermedad mental crónica que afecta a alrededor de 24 millones de personas en el mundo, dentro de esta enfermedad es común encontrar el consumo de sustancias psicoactivas por parte de los pacientes en las que el cannabis encabeza esta lista, esta droga tiene relaciones particulares con la esquizofrenia por medio del efecto de los cannabinoides propios de la planta.
Objetivo: determinar la relación entre el consumo de cannabis y la esquizofrenia.
Metodología: se realizó una revisión bibliográfica narrativa; para la búsqueda de información utilizándose bases de datos como Scopus y PubMed con descriptores MESH/DECS mediante palabras clave, teniendo en cuenta artículos desde el 2009 hasta el 2023, en idiomas inglés y español y con criterios de inclusión y exclusión de los artículos a analizar.
Resultados: se evaluó que el consumo de cannabis podía desencadenar un episodio psicótico en individuos vulnerables; se encontró que la transición a la psicosis se produjo entre quienes empezaron a consumir cannabis antes de los 15 años y continuaron con su consumo de manera frecuente. Los consumidores de cannabis no fueron más propensos a desarrollar psicosis que aquellos que nunca habían consumido cannabis.
Conclusiones: el consumo de cannabis es uno de los factores de riesgo modificables con mayor importancia en el desarrollo de psicosis ya que este actúa como una causa componencial para el desarrollo de un evento psicótico que se enmarque dentro del espectro de la esquizofrenia.
Palabras clave: Esquizofrenia; Cannabis Sativa; Tetrahidrocannabinol; Cannabidiol.
INTRODUCTION
Cannabis sativa is a plant of the family Cannabaceae. Within the spectrum of this plant, it is worth mentioning the role of cannabinoids that give it its particularity characterizing it. Here, THC (tetrahydrocannabinol) and CBD (cannabidiol) stand out.(1) THC has a powerful psychoactive effect to which the recreational use of the plant is referred; on the other hand, when we speak about the non-psychoactive components of the plant, CBD represents the most valuable object seen from the viewpoint of its medicinal properties.(2)
Consumption of psychoactive substances relates to schizophrenia since it is estimated that 30 % to 66 % of those suffering from that disease have informed they abuse different substances such as alcohol, Cannabis, Tobacco, and cocaine, where cannabis keeps on ranking first on the list.(3)
In clinical practice, it is common to find patients diagnosed as schizophrenic dependent on psychoactive substances.(4) As explanations in this regard, drug induction due to dopaminergic malfunctions causes the negative symptoms suggestive of compulsive consumption, owing to the decadent affective condition of the individual, which has been proposed as a comorbidity of this fact.(5)
As suggested by the World Health Organization, schizophrenia is a mental disorder that has a frequency ranging from 1 % to 1,5 % of the population worldwide.(6)
The frequency of appearance of this disease is not high; however, it is important to stress that schizophrenia is one of the 10 diseases causing disability at the world level.(7)
In recent years, it has been possible to bring to light the causes of schizophrenia. They have been related to genetic components and environmental factors that have repercussions on this disease's later development.(8) Exposure to cannabis may be a part of an etiology component of this disease that, when interacting with other factors triggering a psychotic episode, can induce the appearance of this disease. However, it is not to be understood that exposure to cannabis is the only triggering factor.(9) However, in depriving of the known etiologies of this disease, the componential etiology keeps being important.
To elucidate the neurobiological panorama of exposure to cannabis and the development of psychosis, a causal relationship has been stipulated where the possibility that there may be a repercussion on the process of neurobiological development, such as synaptic neuroplasticity, is considered.(10)
Several environments because of which cannabis and schizophrenia bear relation have been proposed following are some of them: common sociodemographic factors and shared genetics, the hypothesis of self-medication, the hypothesis of vulnerability and also severe intoxication occurring with psychotic experiences.(11)
Cannabis worsens psychotic symptomatology, thus posing the possibility of the existence of a “vulnerable” group. In a piece of research in which intravenous THC was administered to patients who have schizophrenia and receiving antipsychotic treatment, it was found that, after administering THC, the positive symptoms were exacerbated. Likewise, within the spectrum of individuals with high vulnerability, there was a group with more unusual symptoms such as unusual perception, paranoia and hostility. This theory has been used to explain the vulnerability proper to the individual to denote its relation to psychosis.(12)
Within the sociodemographic factors, a study using images at the brain level evidenced that both men and women who started consumption before being 17 years old lacked a significant percentage of gray matter in the cerebral cortex and a higher proportion of white matter as compared to the group who started consumption later, thus proposing that the early age for consumption could fall into a period prone to the effects produced by cannabis at the brain level.(13)
In a study where the interaction between Vall158Met polymorphism of the genotype (COMT) (related to dopaminergic regulation) and cannabis consumption at the initial stages of psychosis, cannabis users had a significantly earlier start of psychosis. The relation cannabis-COMT denoted a significant effect at the beginning of the psychosis, as the duration of untreated psychosis. This way, cannabis could modulate the genotype, suppressing the delaying impact on the onset of this episode in patients with the MET allele.(14,15)
The main goal of this piece of research is to determine the relationship between cannabis consumption and schizophrenia.
METHODS
A narrative bibliographic review was performed, and information in databases such as Pubmed, Lilacs and Scopus, in English and Spanish, was gathered.
Included in the selection criteria were the articles relating to cannabis consumption and its adverse effects and articles on schizophrenia and its relation to the consumption of psychoactive substances. Duplicated articles and those without any results relevant to the topic under study were excluded.
The following keywords were used: Cannabis and Schizophrenia, Schizophrenia and Neurobiology, and Cannabis and Psychosis, according to the terms MESH/DECS; likewise, the boolean operators “And”, “Or” and “Not” were combined. Finally, 8 articles were included for analysis after applying selection criteria (Figure 1).
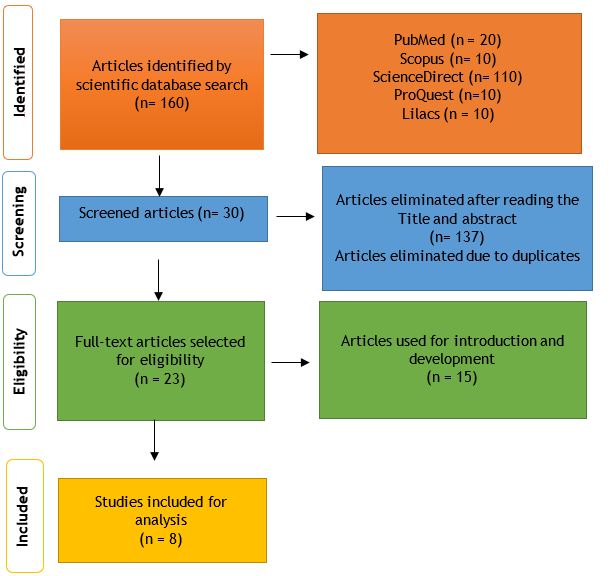
Figure 1. Eligibility criteria
RESULTS
|
Table 1. Relationship of cannabis use to the occurrence of a first psychotic episode |
||||
|
Author(s), Year, Place |
Title |
Sample |
Type of study |
Results |
|
Valmaggia et al.(16) 2014, London |
Consumo de cannabis y transición a la psicosis en personas con riesgo alto |
134 |
Prospective |
The transition to psychosis occurred among those who started using cannabis before the age of 15 years and continued to use it frequently (frequent use at the beginning: 25 %; infrequent or late use: 5 %; χ 2 1 = 10,971, p = 0,001). However, in the overall sample, cannabis users were no more likely to develop psychosis than those who had never used cannabis (use: 12,7 %; non-use: 18,8 %; χ 2 1 = 1,061, p = 303). |
|
Wobrock et al.(17) 2009, Saarland, Alemania |
Abuso de sustancias comórbido y morfología cerebral en la psicosis de inicio reciente |
68 |
Prospective |
Using the interview (Europ-ASI), 32 of 68 patients with established schizophrenia or a recent diagnosis of schizophrenia reported lifetime substance abuse. The substance of abuse was cannabis (THC) in 31 patients, stimulants (amphetamines, ecstasy) in nine patients, cocaine in six patients, opioids in four patients, hallucinogens in four patients and alcohol in four patients. In all cases, patients experienced their first admission concerning the psychopathology of schizophrenia. Twenty patients had detections of delta-9-tetrahydrocannabinol (THC) or its metabolites and amphetamine derivatives in their urine on admission, and two patients had detections of both substances. |
|
Peters et al.(18) 2009, Ámsterdam |
Esquizofrenia de inicio reciente y consumo de cannabis en adolescentes: ¿Evidencia de hiperconectividad estructural mediante resonancia magnética? |
35 |
Prospective |
This study found increased anisotropy in the frontal white matter and anterior internal capsule in patients with recent-onset schizophrenia who had used cannabis or more severe drugs before the age of 17 years compared to controls in healthy patients, this is because there was considerable masking between the two groups of patients, regardless of whether the result was related to the actual use of cannabis or another type of substance of abuse. |
|
Hindley et al.(19) 2020, Reino Unido |
Síntomas psiquiátricos causados por los constituyentes del cannabis: revisión sistemática y metanálisis |
- |
Systematic review/Meta analysis |
Total symptoms were assessed by nine studies, ten trials (including two independent trials) and 196 participants; THC significantly increased the severity of schizophrenia symptoms compared to placebo and the effect was large (SMR: 1,10 [95%CI: 0,92-1,28]. p<0,0001. |
|
Colizzi et al.(20) 2020, London |
El delta - 9 - tetrahidrocannabinol aumenta los niveles de glutamato estriatal en individuos sanos: implicaciones para la psicosis |
16 |
Prospective |
Eleven subjects (69 %) were identified as responding to the psychostimulant effects of 9-THC due to an increase of ≥2 points on associated PANSS items. Baseline psychotic symptoms increased by 5,91 points (±4,18), compared with 0,6 points (±0,55) for the other participants (drug effect, t = 4,13, p = 0,002). |
|
Welch et al.(21) 2011, Edinburgh, Escocia. |
El impacto del uso de sustancias en la estructura cerebral en personas con alto riesgo de desarrollar esquizofrenia |
150 |
Case-control |
When comparing subjects with one or more cannabis exposures to those with less exposure, the former had a higher prevalence of schizophrenia (p = 0,029, OR = 3,18, 95%CI = 1,08-9,36). Ecstasy and amphetamine use did not predict the development of schizophrenia. However, given the small number of subjects exposed to these drugs, the results are not limited specifically to the effects of cannabis, but also to the use of ecstasy and amphetamines. |
|
James et al.(22) 2011, Oxford (Inglaterra) |
Mayores cambios en la materia blanca y gris asociados con el consumo temprano de cannabis en la esquizofrenia de inicio en la adolescencia (EAO) |
60 |
Case-control |
Compared to non-users, cannabis users had lower gray matter density in the temporal sulcus, parahippocampal cortex, ventral striatum, right medial temporal cortex, insular cortex, parietal lobe, right parahippocampal cortex, dorsolateral prefrontal cortex, left occipital cortex, lateral occipital cortex, and cerebellum. Comparisons of similar groups showed reduced fractional anisotropy (FA) in the using patients especially in the brainstem, internal capsule, radial cortex, and superior and inferior longitudinal tracts; there were no differences in cognitive function among non-using patients. |
|
Stanfield et al.(23) 2018, Edimburgo, Escocia. |
Impacto del consumo de cannabis en el volumen talámico en personas con alto riesgo familiar de esquizofrenia |
57 |
Longitudinal |
Cannabis exposure was associated with a reduction in bilateral thalamic volume. This effect was significant on the left side (F = 4,47, p = 0,04) and highly significant on the right side (F = 7,66, p = 0,008). These results remained significant when subjects who had used other illicit drugs were excluded from the analysis. |
DISCUSSION
When analyzing the different patterns of cannabis consumption and how its measure may trigger a psychotic episode, it was found that transition to psychosis occurred among those who started to consume cannabis before being 15 years old and continued consuming it frequently.(16) This denotes that early cannabis consumption (before being 15 years old) may interfere with the onset of a psychotic episode in certain patients, as not all cannabis consumers developed a psychotic episode; this is in tune with the comparison of those who do not consume any substance.
These results were found by Peters et al.(18) who, in their study, demonstrated that those patients consuming cannabis or another kind of drug before being 17 years old developed psychotic symptomatology compatible with the spectrum of schizophrenia. This piece of research used imaging methods (magnetic resonance) to compare changes at the brain level of those substance-consuming patients who included cannabis compared to patients who did not consume any substance. There were results denoting changes in the frontal white matter and at the level of the internal capsule in those who consumed cannabis or other drugs before being 17 years old. Likewise, in their study that compared individuals with a more prolonged period of exposure to cannabis with those who were less exposed, Welch et al.(23 ) denoted that the former had a much higher prevalence of schizophrenia.
In this sense, according to the above and when analyzing these results, we can affirm that factors such as early cannabis consumption and prolonged exposure to this substance are precipitants of a psychotic episode compatible with the spectrum of schizophrenia.
The abused substance was cannabis (THC). Here we can infer that cannabis consumption in tune with the consumption of other drugs predisposes their consumers to a higher risk of developing a psychotic disorder compatible with the spectrum of schizophrenia, as evidenced in almost half of the studied patients.
The results were in tune with the study by Colizzi et al.(20), where 17 participants were exposed to the psychoactive component of cannabis, and 69 % of them developed psychotic symptomatology, unlike the unexposed participants. According to the questionnaire: Positive and Negative Syndrome Scale (PANSS) (used to determine the adverse symptomatology of schizophrenia), this first group increased by 5,91 points, and the unexposed group increased by only 0,6 points. Also, the study by James et al.(22) elucidated the changes occurring at the nervous system level in continuous cannabis consumers, such as less density in the gray matter of the temporal groove, parahippocampal cortex, right temporal cortex and parietal lobe. In contrast with the imaging findings in non-consumers, who did not have any critical anomaly at the level of the cephalic mass.
Regarding the findings, it can be elucidated that factors such as drug poly-consumption at an early age can precipitate the onset of a psychotic episode that, when recurring continuously, can fall into the spectrum of schizophrenia. Also, the imaging findings concerning the changes in the nervous system in continuous cannabis consumers in tune with those who do not consume that substance are evident. Therefore, it is worth mentioning that consumption of multiple drugs in addition to cannabis at an early age is a precipitant factor for the development of a sustained psychotic episode that can be compatible with the spectrum of schizophrenia, a fact the imaging findings and the clinical spectrum of this disease support that.
These results coincide with those found by Peters et al.(18) in their study, where they observed an increase in the anisotropy of the white matter in the frontal area and the anterior internal capsule in patients whose schizophrenic condition had started recently. They all had been drug users before being 17 years old. For their part, Valmaggia et al.(16), in their study, stress that transition to psychosis occurred in those users who started to consume cannabis before being 15 years old with a frequent and regular consumption pattern.
In light of the above, we can establish that most research emphasizes the same psychosis-triggering factor: early and sustained cannabis consumption. This factor, in tune with the imaging findings, makes us compare the evident loss of the thalamic volume in those consuming patients that is very similar to the loss of thalamic volume present in those who already have an established diagnosis of schizophrenia and have undergone an imaging study.
CONCLUSIONS
We can conclude that cannabis consumption may be the precipitant of a psychotic episode and, later on, schizophrenia, mainly those who started to consume before being 15 years old and keep a frequency and regularity for a considerable time. The imaging findings play an important role as they are reliable markers of the changes at the level of encephalic mass, the most frequent being the bilateral loss of thalamic volume both in chronic cannabis consumers and in patients with an established diagnosis of schizophrenia
BIBLIOGRAPHIC REFERENCES
1. Lucas CJ, Galettis P, Schneider J. The pharmacokinetics and the pharmacodynamics of cannabinoids. Br J Clin Pharmacol 2018; 84(11):2477-82. https://doi.org/10.1111/bcp.13710
2. Jenkins BW, Khokhar JY. Cannabis Use and Mental Illness: Understanding Circuit Dysfunction Through Preclinical Models. Front Psychiatry 2021 ;12:597725. https://doi.org/10.3389/fpsyt.2021.597725
3. Connor JP, Stjepanović D, Le Foll B, Hoch E, Budney AJ, Hall WD. Cannabis use and cannabis use disorder. Nat Rev Dis Primers. 2021; 7(1):16. https://doi.org/10.1038/s41572-021-00247-4
4. Jalewa J, Todd J, Michie PT, Hodgson DM, Harms L. The effect of schizophrenia risk factors on mismatch responses in a rat model. Psychophysiology 2023; 60(2). https://doi.org/10.1111/psyp.14175
5. Gunasekera B, Diederen K, Bhattacharyya S. Cannabinoids, reward processing, and psychosis. Psychopharmacology 2022; 239(5):1157-77. https://doi.org/10.1007/s00213-021-05801-2
6. Queirós TP, Coelho FS, Linhares LA, Correia DT. Esquizofrenia: O Que o Médico Não Psiquiatra Precisa de Saber. Acta Med Port 2019; 32(1):70. https://doi.org/10.20344/amp.10768
7. Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, et al. Global Epidemiology and Burden of Schizophrenia: Findings From the Global Burden of Disease Study 2016. Schizophrenia Bulletin 2018; 44(6):1195-203. https://doi.org/10.1093/schbul/sby058
8. Green MF, Horan WP, Lee J. Social cognition in schizophrenia. Nature reviews. Neuroscience 2015; 16(10), 620–631. https://doi.org/10.1038/nrn4005
9. Hamilton I. Cannabis, psychosis and schizophrenia: unravelling a complex interaction: Cannabis, psychosis and schizophrenia. Addiction 2017; 112(9):1653-7. https://doi.org/10.1111/add.13826
10. Pozo-Hernández E, Mariño-Tamayo C, , Ramos-Galarza C. EFECTOS NEUROPSICOLÓGICOS POR EL CONSUMO DE MARIHUANA EN ADULTOS JÓVENES. http://dx.doi.org/10.7714/CNPS/13.3.201
11. Blair Thies M, DeRosse P, Sarpal DK, Argyelan M, Fales CL, Gallego JA, et al. Interaction of Cannabis Use Disorder and Striatal Connectivity in Antipsychotic Treatment Response. Schizophrenia Bulletin Open 2020; 1(1):sgaa014. https://doi.org/10.1093/schizbullopen/sgaa014
12. Ortiz-Medina MB, Perea M, Torales J, Ventriglio A, Vitrani G, Aguilar L, et al. Cannabis consumption and psychosis or schizophrenia development. Int J Soc Psychiatry. noviembre de 2018;64(7):690-704. https://doi.org/10.1177/0020764018801690
13. Wilson J, Freeman TP, Mackie CJ. Effects of increasing cannabis potency on adolescent health. The Lancet Child & Adolescent Health 2019; 3(2):121-8. https://doi.org/10.1016/S2352-4642(18)30342-0
14. Hamilton I, Monaghan M. Cannabis and Psychosis: Are We any Closer to Understanding the Relationship? Curr Psychiatry Rep 2019; 21(7):48. https://doi.org/10.1007/s11920-019-1044-x
15. Sami MB, Bhattacharyya S. Are cannabis-using and non-using patients different groups? Towards understanding the neurobiology of cannabis use in psychotic disorders. J Psychopharmacol 2018;32(8):825-49. https://doi.org/10.1177/0269881118760662
16. Valmaggia LR, Day FL, Jones C, Bissoli S, Pugh C, Hall D, et al. Cannabis use and transition to psychosis in people at ultra-high risk. Psychol Med 2014; 44(12):2503-12. https://doi.org/10.1017/S0033291714000117
17. Wobrock T, Sittinger H, Behrendt B, D’Amelio R, Falkai P. Comorbid substance abuse and brain morphology in recent-onset psychosis. Eur Arch Psychiatry Clin Neurosci 2009; 259(1):28-36. https://doi.org/10.1007/s00406-006-0707-x
18. Salazar de Pablo G, Davies C, de Diego H, Solmi M, Shin JI, Carvalho AF, Radua J, Fusar-Poli P. Transition to psychosis in randomized clinical trials of individuals at clinical high risk of psychosis compared to observational cohorts: a systematic review and meta-analysis. European psychiatry : the journal of the Association of European Psychiatrists 2021; 64(1), e51. https://doi.org/10.1192/j.eurpsy.2021.2222
19. Hindley G, Beck K, Borgan F, Ginestet CE, McCutcheon R, Kleinloog D, et al. Psychiatric symptoms caused by cannabis constituents: a systematic review and meta-analysis. The Lancet Psychiatry 2020; 7(4):344-53. https://doi.org/10.1016/S2215-0366(20)30074-2
20. Colizzi M, Weltens N, McGuire P, Lythgoe D, Williams S, Van Oudenhove L, et al. Delta-9-tetrahydrocannabinol increases striatal glutamate levels in healthy individuals: implications for psychosis. Mol Psychiatry 2020; 25(12):3231-40. https://doi.org/10.1038/s41380-019-0374-8
21. Welch KA, McIntosh AM, Job DE, Whalley HC, Moorhead TW, Hall J, et al. The Impact of Substance Use on Brain Structure in People at High Risk of Developing Schizophrenia. Schizophrenia Bulletin 2011;37(5):1066-76. https://doi.org/10.1093/schbul/sbq013
22. James A, Hough M, James S, Winmill L, Burge L, Nijhawan S, et al. Greater white and grey matter changes associated with early cannabis use in adolescent-onset schizophrenia (AOS). Schizophrenia Research 2011; 128(1-3):91-7. https://doi.org/10.1016/j.schres.2011.02.014
23. Welch KA, Stanfield AC, McIntosh AM, Whalley HC, Job DE, Moorhead TW, et al. Impact of cannabis use on thalamic volume in people at familial high risk of schizophrenia. Br J Psychiatry; 199(5):386-90. https://doi.org/10.1192/bjp.bp.110.090175
FUNDING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHOR CONTRIBUTION
Conceptualization: Roberto Carlos Mora Vera, Rosa Solorzano, Jorge Andrés Lozano Aveiga, Byron Enrique Peña Cordero.
Investigation: Roberto Carlos Mora Vera, Rosa Solorzano, Jorge Andrés Lozano Aveiga, Byron Enrique Peña Cordero.
Methodology: Roberto Carlos Mora Vera, Rosa Solorzano, Jorge Andrés Lozano Aveiga, Byron Enrique Peña Cordero.
Project administration: Roberto Carlos Mora Vera, Rosa Solorzano, Jorge Andres Lozano Aveiga, Byron Enrique Peña Cordero.
Writing - original draft: Roberto Carlos Mora Vera, Rosa Solorzano, Jorge Andres Lozano Aveiga, Byron Enrique Peña Cordero.
Writing - review and editing: Roberto Carlos Mora Vera, Rosa Solorzano, Jorge Andres Lozano Aveiga, Byron Enrique Peña Cordero.