REVIEW
The influence of personalized and precision medicine on the nursing profession
La influencia de la medicina personalizada y de precisión en la profesión enfermera
Nayana Borah1 ![]() *,
Vijimol G2
*,
Vijimol G2 ![]() *, Heena Baria3
*, Heena Baria3 ![]() *
*
1JAIN (Deemed-to-be University), Department of Life Sciences. Karnataka, India.
²Teerthanker Mahaveer University, College of Nursing. Moradabad, Uttar Pradesh, India.
³Parul University, Parul Institute of Nursing. PO Limda, Tal. Waghodia, Gujarat, India.
Cite as: Borah N, G V, Baria H. The influence of personalized and precision medicine on the nursing profession. Salud, Ciencia y Tecnología. 2023;3(S1):448. https://doi.org/10.56294/saludcyt2023448
Submitted: 14-05-2023 Revised: 07-06-2023 Accepted: 01-08-2023 Published: 02-08-2023
Editor: Dr.
William Castillo-González![]()
Associate Editor:
Fasi Ahamad Shaik ![]()
ABSTRACT
Several expectations concerning the effect of molecular biology studies on the Precision-Medicine (PM) have been aroused by the significant investment and growth of this field over the past few decades, particularly after the end of the Human Genome Project. To attain the novel criteria for maintenance, the omics sciences should be involved in the field of nursing, particularly in nursing healthcare. The development of functional genomics study, which collectively comprises the omics sciences includes epigenomics, proteomics, metabolomics, and transcriptomics has been made possible by enhanced methods built on structural genomics understanding. The recent issue is to turn this more comprehensive body of data into therapeutic advantages for patients, such as extra exact diagnoses, treatment, and care which is adapted to the particular requirements of individuals and communities. Integrating omics sciences into educational and professional activities is a significant barrier for nursing, as it prevents nurses from being autonomously, securely, and scientifically empowered to provide tailored care to patients and their families who rely on the PM. The article discusses the impact of PM and the challenges it faces in clinical practice.
Keywords: Precision-Medicine (PM); Personalized Nursing Care; Precision Nursing (PN); Omics Sciences.
RESUMEN
Varias expectativas relativas al efecto de los estudios de biología molecular en la Medicina de Precisión (MP) han sido suscitadas por la importante inversión y el crecimiento de este campo en las últimas décadas, en particular tras la finalización del Proyecto Genoma Humano. Para alcanzar los novedosos criterios de mantenimiento, las ciencias ómicas deben implicarse en el campo de la enfermería, en particular en los cuidados de enfermería. El desarrollo del estudio de la genómica funcional, que en su conjunto comprende las ciencias ómicas e incluye la epigenómica, la proteómica, la metabolómica y la transcriptómica, ha sido posible gracias a la mejora de los métodos basados en la comprensión de la genómica estructural. La cuestión reciente es convertir este conjunto más completo de datos en ventajas terapéuticas para los pacientes, como diagnósticos, tratamientos y cuidados más exactos y adaptados a las necesidades particulares de las personas y las comunidades. La integración de las ciencias ómicas en las actividades educativas y profesionales supone una barrera importante para la enfermería, ya que impide que los enfermeros estén capacitados de forma autónoma, segura y científica para proporcionar cuidados adaptados a los pacientes y sus familias que dependen de la PM. El artículo analiza el impacto de la PM y los retos a los que se enfrenta en la práctica clínica.
Palabras clave: Medicina de Precisión (MP); Cuidados Personalizados de Enfermería; Enfermería de Precisión (NP); Ciencias Ómicas.
INTRODUCCIÓN
Precision medicine (PM) is the act of customizing medical care to each patient's individual needs to direct healthcare decisions toward the best diagnostic and therapeutic options for patients, increasing the bar of care and improving disease management. Nursing care approaches are developing through patient-centered clinical decision-making. They are discovering the precision nursing (PN) method to reflect this new era that can concentrate patients' required nursing care.(1) Healthcare is impliedly distinct from trade and other services because all treatments are undertaken with the patient's well-being as their top priority. Healthcare regulations are governed by a complicated web of national laws as well as specific ethical principles from the World Medical Association. National, federal, and local laws only permit (licensed) physicians to practice medicine, protecting patients in the process.(2) The efficient application of ideas and techniques gained from genomics necessitates changes in professional relationships, local healthcare service organizations, and procedures, as is the case with innovation everywhere. Recent studies have looked into how the doctor-patient relationship has changed and the challenges that come with integrating precision medicine into ordinary healthcare.(3)
Clinical methods for nursing are also changing as a result of patient-centered clinical decision-making, to represent this fresh age, they are coming across the PN technique, which can focus on providing patients with nursing care which is dependent on their requirements. To gather data on the exposure, disease susceptibility, evolution, trait and therapeutic reply, precision health (PH) considers a variety of biological markers, or biomarkers, which include omics, in addition to other factors like lifestyle, economic challenges, cultural traits, environmental factors and social features.(4)
To meet the new criteria for care, the omics sciences should be mentioned in nursing work, in nursing care. In this context, the development of functional genomics study that collectively comprises the "omics" sciences including epigenomics, proteomics, metabolomics, and transcriptomics, has been made possible by enhanced tools built on structural genomics understanding. These methods seek to comprehend how the genome functions differently at different phases of growth and in various environmental settings to improve molecular knowledge.(5) By customizing therapies and procedures to each patient depending on their specific needs, the aim of precision and personalized medicine in the nursing profession is to maximize patient care. Precision and customized medicine seek to improve the results of therapy by taking an individual's genetic makeup, lifestyle choices, environmental effects, and other pertinent information into account. Nurses work to determine which treatments are most beneficial for each patient, minimizing side effects and enhancing therapeutic gains.
Brown et al.(6) required a deeper comprehension of the molecular mechanisms underlying the many causes of renal failure to accomplish this objective. Clinical practice is increasingly incorporating and translating these research findings. In this Viewpoint, they sought the opinions of three people who have experienced renal failure regarding the significance of comprehending the causes of kidney illness and, more specifically, what they hoped might be accomplished with this knowledge. Mitchell et al.(7) presented the results of an evidence-based needs evaluation to examine the present state of knowledge of PM, satisfactory training contended, specious abilities of an additional precise method to motivate the participants in a training program between pharmacists, patient care, common practitioners, and advanced practice nurses. A layout that is appropriate for the intended professions can be supported by looking at perceived demands rather than using a top-down strategy. Curtin et al.(8) produced a thorough summary of the causes, characteristics, and effects of precision medicine across many contexts. With this view, precision medicine may be seen as a crucial component of the larger practice of precision health, which was put forth by nursing scholars to give patients comprehensive, all-encompassing treatment. The structure for care is a model for precision health. Fu et al.(9) provided a general review of PH and stresses the significance of involving the nursing field in its execution. The study ends with suggestions for nurse leaders to create strategic plans to adopt precision health in settings such as policy, research, education, clinical practice, and nursing administration. Morgan et al.(10) explored how these results may affect the creation of fresh efforts aimed at enlisting the public in developing PM programs, especially between smaller groups. It also examines interaction-depends on treatments, such as instruction in interpersonal interaction, public relations campaigns, the development of persuasive messages, and the delivery of targeted messages. Lebet et al.(11) integrated genetic and genomic information has become increasingly important in nursing medicine, study, and learning due to the increased emphasis on precision medicine and healthcare. This is because it helps nurses to work efficiently with patients to improve their health and well-being. Smith et al.(12) introduced a new way of doing things and provides methodical clarity about how to quickly examine independently tailored PM interventions. Zatloukal et al.(13) addressed the wide range of illness sub-entities essential for targeted therapeutics, PM study needs access to a significant quantity of trials and information. Fujita et al.(14) provides and implements the most recent study results in this narrative review, they want to advance polypharmacy-related precision medicine. In particular, this article seeks to (1) summarize difficulties in attaining PM related to polypharmacy; (2) synthesize present strategies for PM in polypharmacy; (3) offer an overview of research in the field of predicting unknown drug-drug interactions (DDI); and (4) suggest an innovative strategy to offer PM for patients with polypharmacy. Sun et al.(15) demonstrated the serious concerns held by biomedical professionals over the limitations of the biological model of health. The medical model of health that was based on the 19th-century germ theory can be viewed as a modern update when precision public health is anchored in genomics.
METHODS
Customizing treatment based on the biological traits of individuals or population segments is the aim of PM. A variety of diseases that causes may share the same symptoms. Similarly to this, treatment might work well for some people with a condition but not for others who appear to have the same ailment. Recognizing that diverse groups of people have distinct genetic traits and that therapies should take these variances into account, forms the basis of precision medicine. The Precision-treatment promises to provide the correct treatment, in the exact amount, at the appropriate moment, increasing its efficiency and lowering healthcare expenses. This depends on the recognition of the patient's genetic traits. The discussion of PM in health care typically encompasses a larger idea. This idea gives customization a preventative, predictive, and participative component. These concepts include the possibility of executing prenatal diagnosis, pre-sympathomimetic evaluation, the presence of relevant phenotypes caused by mutations and variations at various loci, the presence of various alleles of an identical gene in the population, the idea that certain diseases may run in families and be caused by genetic variations increasing disease susceptibility through interactions between genes and environments as well as various kinds of mutations. Effective inter-professional teamwork, community outreach initiatives, and care coordination are necessary for the execution of individualized nursing care in the PM. And this is good news for nursing since nurses are in a good position to drive the adoption of PH. Fewer nurses are informed of or able to understand the importance of PH for the nursing profession, despite the growing interest in this field. The nursing profession must therefore create tactical ideas which improve customized nursing care in the PM that involves the nursing study, learning, medical treatment, and health policy sectors. In this approach, important strides have been achieved in preparing the nursing work to expand scientific understanding and utilize information to enhance population health and preventative measures in the PM. Such as, nurses may examine how genetic variation in one or more genes simultaneously (pharmacogenomics) or in individual genes (pharmacogenetics) affects how people react to pharmaceutical drugs and food. Table 1 denotes the suggestions for nurses to transform and combined personalized medicine in the PM in clinical practice.
|
Table 1. Suggestions for nurses to transform and combined personalized nursing care in the PM in clinical practice |
|||
|
Suggestions for Nursing clinical training |
Suggestion for Nursing in health policy |
Suggestion for Nursing study |
Suggestion for Nursing learning |
|
The goal of this course is to ensure that registered nurses in a variety of practice settings have the knowledge and skills necessary to offer personalized nursing care, such as the administration of drugs dependent on Pharmaceutical Genomics, interpreting of genetic test results, and referring of patients with high-risk family backgrounds to genetics therapy. |
Create legislative or regulatory remedies for PM concerns not covered by existing laws that maximize patient privacy. Some examples of these concerns are the need to acquire informed consent from patients before storing or using omic or other health information, as well as the need to preserve patients' privacy and prevent their information from being exploited against them in work and insurance decisions. |
Personalized nursing care in the PM era should emphasize preventive and managing symptoms across the lifetime, thus it's important to conduct study which develops knowledge on the most effective formats and methods for educating patients, family members, and caregivers about these topics. |
Create material for ongoing nurse education and training that focuses on PM-based personalized nursing care. |
|
The nursing profession's understanding of PM interventions is incorporated into the delivery of care in techniques that protect patients and empower them to make educated decisions. |
Encourage healthcare organizations and institutions to adopt cutting-edge practices so that omics data may be used to enhance patient care and results. |
Apply omics science, digital, lifestyle, and environmental factors to patient data to determine which actions will have the most impact on health results. |
To successfully execute omic and Personalized Nursing Care in the PM Era, it is important to use and participate in worldwide nursing professional alliances that have solid genetic/genomic teaching structures. |
|
Create clear and concise patient education materials and informational content on the PM which informs and empowers patients. |
Assistance with PM in healthcare systems, study, and training for nurse officials and leaders. To ensure safe patient care, for example, their institution’s entry-level and advanced practice nursing nursing policies should be developed. |
Maintain ongoing financial assistance for cutting-edge PM Era initiatives including the Graduate Partnerships Program, Postdoctoral Fellowships, Data Science Boot Camp, and training internships or study rotations at the Symptom Science Center. |
Boost governmental and private support for PhD nursing faculty training in order to start maintaining the integrating of Personalized Nursing Care in PM Era content across all nursing programs and curriculum accrediting standards. |
The use of pharmacological substances to improve, manage, and advance patients' health may be monitored and managed by nurses by integrating this information into patient care. Consequently, nursing in the era of PM necessitates an aim on every patient's risk for disease and the efficacy of therapies depending on every patient's particular mix of genetic and environmental risk factors. Even though incorporating a nursing viewpoint into project management is essential for success, there are still barriers to overcome. To provide individualized nursing medicine in the context of PM, the nursing profession needs to develop tactical ideas that improve PH in the study, learning, medical care, and health policy. Nurses are in an ideal spot to lead in the next phase of PM and direct integration into health education, illness avoidance, and treatment because of their holistic approach to nursing.
Omics
Omics relates to a broad range of scientific fields and methods that are utilized to research biological systems on a vast scale. To better understand the function, structure, and communications of biological molecules including RNA, DNA, metabolites, and proteins entails a thorough investigation of those molecules. Numerous biomedical sciences fields that finish in omics, including genomics, transcriptomics, proteomics, and metabolomics, are referred to as omics. These fields' study subjects finish in -ome, including the genome, transcriptome, proteome, and metabolome. The study of genomes' structure, functioning, alteration, mapping, and editing is the emphasis of genomics. The term "transcriptome," which is also used to describe the research of the transcriptome, refers to all the RNA molecules found in a cell. Proteomics is a scientific investigation of all proteins found in a cell, tissue, or organism; the study of the chemical reactions that metabolites the byproduct of biological processes go through is called metabolomics.
Personalized medicine
The most popular term used to represent the possibilities and goals of translational big data predicted, and network biomedicine in biomedical discourses is personalized medicine. Due to the European Commission's adoption of it as the preferred term to describe associated technological development and study in the context of European healthcare facilities, it has also come to be the most commonly used term in debates about European policy. However, there are 2 main areas of disagreement about the definition and application of the idea: Initially, whether the term personalized medicine must be used, and second, what exactly the idea does or must involve. Both arguments center on the concept's future-focused applications as well as the various governmental and biomedical players' contextual interpretations and definitions of the concept's significance. The Innovative Medicines Initiatives of the Horizon 2020 initiative, which aims to hasten the creation of efficient preventive and diagnosis technologies, is a part of the present investment. This description was used by the Horizon 2020 initiative that highlighted greater knowledge of disease etiology at the phase of a system as a significant study focus and recognized personalized medicine as a core subject. The Horizon advisory committee explained why they chose the word personalized medicine over other alternatives, stating that it better expresses the ultimate objective of efficiently personalizing treatment depending on an entity's profiles, as defined by the entity genome and phenotype information. The concept of customized medicine underlines the long-term objectives motivating study spending in the European policy framework by emphasizing patient-centered techniques, individuals' ownership and manage across their health, and medical predictive schemes. The investment is driven by the aspiration of personalized therapies which provides the appropriate therapeutic approach for the appropriate patient at the appropriate time. These aspirations are intertwined with the idea of personalized medicine as an idea shifts not only for studies but also for healthcare systems and citizens. To facilitate ownership, sharing, and accountability to one's data and health, the concept of arranging people at the center of healthcare has several objectives. Health-related responsibilities indicate personalization of healthcare, in the sense which has greater responsibilities for handling the healthcare are mainly laid on.
Precision medicine (PM)
The PM project was supported by the National Research Council (NRC) in their 2011 PM report, which stated the study's ultimate goal is to allow the choice of a subgroup of patients with a similar biological basis for disease who will likely get the greatest from the therapy. The PM Initiative (PMI) spent $215 million to fund its mission of ushering in a innovative era of healthcare study, methods, and regulations which equip patients, investigators, and suppliers to collaborate on bettering individualized care. The Precision Medicine Initiative (PMI) reframes precision medicine as a method to disease treatment and avoidance which must increase efficiency by considering genetic, environmental, and lifestyle variability at the individual level. Initially, the NRC meant subgroup categorization when they used the term precision. After receiving $10 million to establish new directing and evaluate procedures for the PMI, the FDA, like the European Commission, highlighted that the aim of PM is to aim the appropriate medications to the exact patients at the right time. The PMI is based on a plan developed by the National Institutes of Health (NIH) to recruit one million participants in order to establish a longitudinal cohort representative of the demographic variety of the US population. In order to detect connections among genetic and environmental factors and a wide variety of health results, they plan to develop a databank that is large enough to facilitate the research of biological, clinical, social, and environmental determinants of health and disease. The proposal to collect and preserve data includes biospecimens, physical measurements, electronic health records, participant-provided data obtained through enquiries, and even mobile and digital health data from health, fitness, and wellness devices and apps. The databank is expected to be broadly available, such as citizen scientists and engaged participants, and has a wide range of potential uses, containing quantitative estimations of illness risk and optimization of screenings and preventative techniques. The way that precision medicine is conceptualized by the PMI differs dramatically from how it was first marketed by the NCR. But its closeness to policy discourses on customized medicine in Europe shows how different terminology with different connotations have been chosen and used in different policy contexts while being pushed similarly to explain the promise of large health data and predictive systems-level analysis. By avoiding the term personalized's promising but potentially overly ambitious promise, precision avoids objections of the latter while still enabling policymakers to harness the rhetorical power of prescription customized to each individual's lifestyle, genes, environment, and preferences. It sidesteps the moral dilemmas inherent in ethically neutral or even beneficial precision by recasting the medical profiling and group stratification which prediction and systems methods enact as a necessary evil. This last rhetorical aspect stands out in light of the long history of racial divide in American politics that has its roots in scientific racism, as well as the long history of significant and effective anti-racist politics and protest that has developed in response to this split. Using precision as an umbrella term makes it easier to combine genomics with other difficult methodologies including biobanking and data mining of electronic medical records.
RESULTS
In this section, the PM assigns more emphasis on patient-centered care that is consistent with the core values of nursing. Nurses can play a critical part in gathering and evaluating patient data to help grow personalized treatment plans. Personalized and precision medicine concentrate on tailoring healthcare treatments to individual patients depending on their unique characteristics, such as genetics, lifestyle, and environmental factors. Numerous cancer types, the low cost of personalized medicine treatment in cancer pharmaceuticals, and some other illness indicators are predicted to be the main drivers of the expanding domination of the global market for customized medicine. Based on the WHO, cancer raised 10,7 million deaths globally in 2023 and was the next important cause of death. Around the globe, cancer is responsible for 1 in 6 fatalities. In personalized medicine, a diagnosis is often prepared to select the best and most effective treatments depending on the patient's genetic makeup or other molecular or cellular analyses. Personalized medicine has the best response and the highest safety margin, allowing for faster diagnosis, risk assessment, and the optimum treatment for each patient. Another potential benefit of personalized medication.
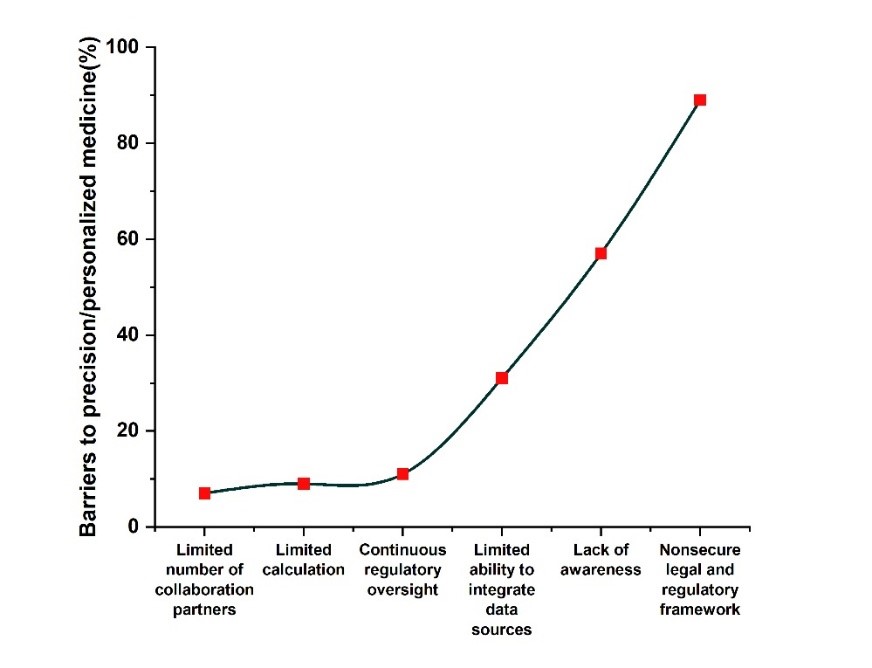
Figure 1. Barriers to Precision and personalized medicine
|
Table 2. Efficiency of PM |
||
|
|
Percentage of Barriers to precision/personalized medicine |
|
|
Limited number of collaboration partners |
7 |
|
|
Limited calculation |
9 |
|
|
Continuous regulatory oversight |
11 |
|
|
Restricted capacity to integrate data sources |
31 |
|
|
Absence of consciousness |
57 |
|
|
Nonsecure legal and regulatory structures |
89 |
|
Figure 1 denotes the barriers to precision and personalized medicine and table 2 denotes the values of PM. The rise in the incidence of various kinds of cancer, the low cost of personalized medicine treatment for cancer drugs and other disease indications, a reduced danger of side effects from personalized medicine treatment, the high adoption in developed markets, and the development of novel drugs are the main factors driving the global personalized medicine market. In the coming years, the industry is projected to be constrained by fierce competition, stringent government regulations governing product permission, and an absence of knowledge between the rural populace in emerging countries. Because it can target cancerous areas, tailored medicine is expected to become much more widespread throughout the projection period. The global market for personalized medicine will also grow as a result of lowered adverse side effects and a high acceptance rate in developed economies.
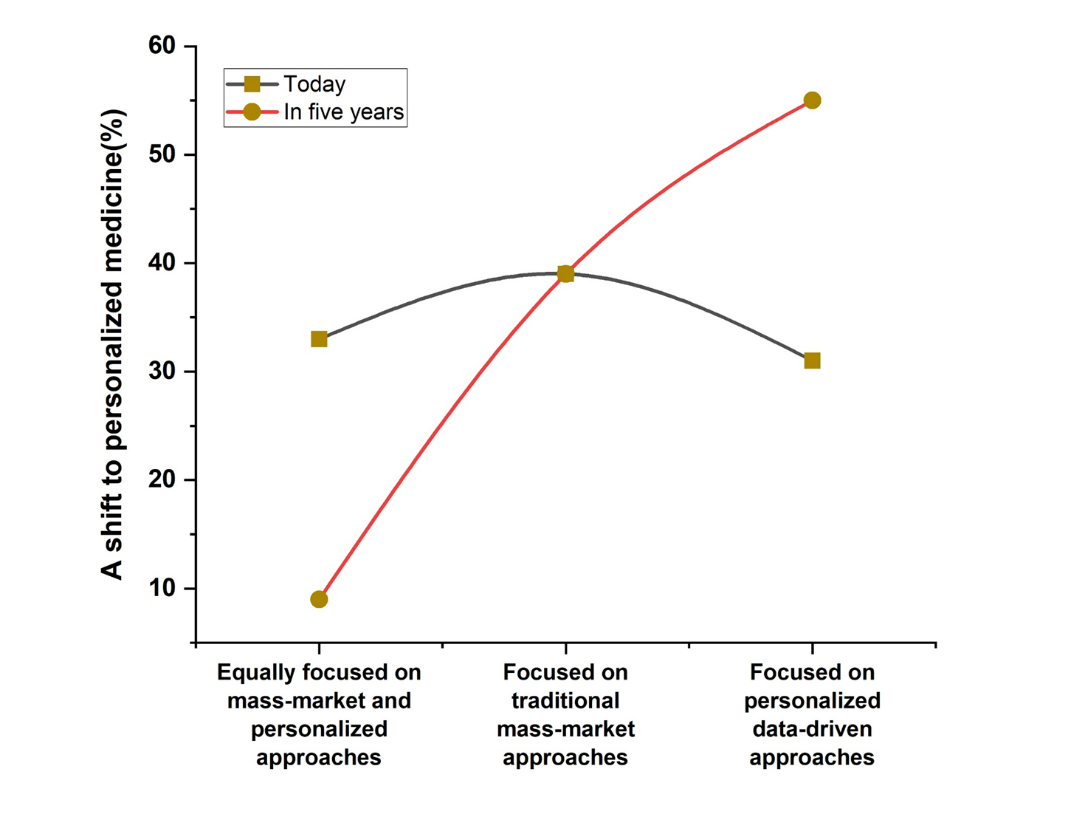
Figure 2. Alteration to Personalized Medicine
|
Table 3. Numerical values of Personalized medicine |
||
|
A shift to personalized medicine |
Today |
In five years |
|
Equally concentrated on mass-market and personalized methods |
33 |
9 |
|
Focused on traditional mass-market approaches |
39 |
39 |
|
Concentrated on personalized data-driven methods |
31 |
55 |
Figure 2 denotes the alteration to personalized medicine and table 3 denotes its numerical outcomes. The paper outlines the pharmaceutical and healthcare organizations are doing to advance the PM revolution as well as what more needs to be done. By moving beyond one-size-fits-all methods of prevention, diagnosis, and treatment, PM is revolutionizing healthcare. It does this by utilizing genetics, genomics, and big data. This tailored treatment comes with the potential of better patient outcomes, cost savings, and increased system effectiveness, but it also comes with significant obstacles. Personalized medicine is becoming more important than mass-market strategies, which were once dominant. The old paradigm is still prevalent, and other initiatives (like population health, which emphasizes community-wide prevention) are also growing, but focused methods are getting closer to being ready for prime time.
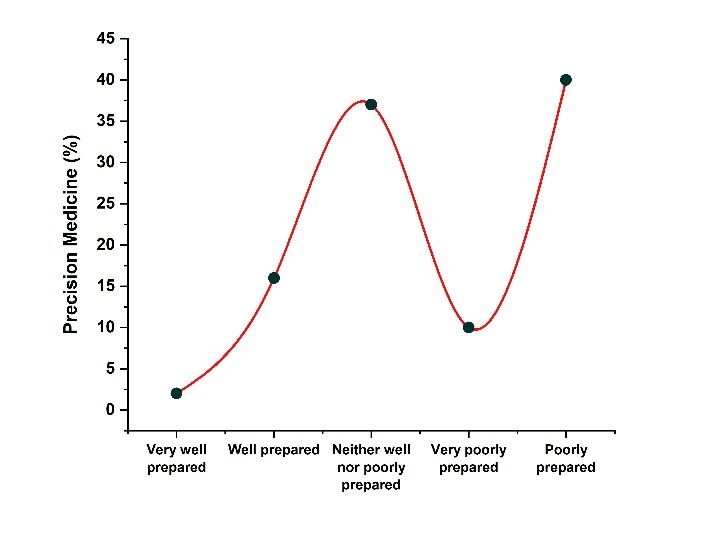
Figure 3. A split of trainee results based on how well-prepared they think they are to practice PM in the future
|
Table 4. Numerical results of PM trainee |
|
|
|
Precision Medicine (%) |
|
Very well prepared |
2 |
|
Well prepared |
16 |
|
Neither well nor poorly prepared |
37 |
|
Very poorly prepared |
10 |
|
Poorly prepared |
40 |
The figure 3 denotes the split of trainee outcomes depending on well prepared to practice PM in the future and the table 4 represents the numerical results of PM trainees. Only 25 % of participants believed they fully understood the implications of mainstreaming genomic treatment for clinical practice in the future. Although more senior trainees than junior trainees are likely to comprehend what genetic mainstreaming means (28,8 % vs 15,3 %), this variation did not reach statistical importance. Comparing trainees with a Master’s or Ph.D. to those with a BSc or no further degree, similar results were found. Furthermore, just 11 % and 18 % respectively, of participants think that their local training program effectively arranges them to apply personalized healthcare.
CONCLUSIONS
The set of data that is currently available has substantially increased to technological developments brought on by the omics sciences, opening up new avenues for more effective illness therapies. The current issue is to translate this larger body of knowledge into therapeutic advantages for patients, including more precise diagnoses, therapies, and individualized care for their unique needs and those of their communities. The importance of nursing roles in the execution of PM cannot be overstated. These roles include providing personalized nursing care for patients, educating families about the description of omic tests, performing healthiness and personal evaluations, such as family history, and providing serious comments and awareness on the viability of integrating novel skills into medical processes. In terms of the level of training, in any clinical setting, nurses can help the PM advance its goals, learning, study, and policy context. It is crucial to conduct a cost-profit analysis from an ethical standpoint before implementing new precision medicine technology, taking into account whether they will be available to everyone who may utilize them and whether they won't worsen health inequities. The integration of the omics science into nursing education and professional practice is the biggest obstacle, to allowing nurses to independently, safely, and scientifically empower patients and families with individualized treatment dependent on PM. Through study and practice that is based on the best available data, the nursing profession can promote precision and individualized treatment. To investigate the efficacy and results of individualized interventions, nurses might take an active part in research projects. To create evidence-based recommendations and practices for individualized care, they can also work with researchers from different fields.
REFERENCES
1. Ielapi N, Andreucci M, Licastro N, Faga T, Grande R, Buffone G, Mellace S, Sapienza P, Serra R. Precision medicine and precision nursing: the era of biomarkers and precision health. Int J Gen Med. 2020;13:1705-1711.
2. Orth M, Averina M, Chatzipanagiotou S, Faure G, Haushofer A, Kusec V, Machado A, Misbah SA, Oosterhuis W, Pulkki K, Twomey PJ. Opinion: redefining the role of the physician in laboratory medicine in the context of emerging technologies, personalized medicine, and patient autonomy ('4P medicine'). J Clin Pathol. 2019;72(3):191-197.
3. Bergeron H, Castel P, Vézian A. Beyond full jurisdiction: pathology and inter-professional relations in precision medicine. New Genet Soc. 2021;40(1):42-57.
4. Al-Kaiyat MO. Precision coordination: the growing role of the nurse coordinator in the Era of personalized medicine. Int J Nurs Stud. 2018;22(1):113-115.
5. Sun S. Between personalized and racialized precision medicine: A relative resources perspective. Int Sociol. 2020;35(1):90-110.
6. Brown KD, Campbell C, Roberts GV. Precision medicine in kidney disease: the patient’s view. Nat Rev Nephrol. 2020;16(11):625-627.
7. Mitchell S, Jaccard E, Schmitz FM, von Känel E, Collombet P, Cornuz J, Waeber G, Guessous I, Guttormsen S. Investigating acceptability of a training program in precision medicine for frontline healthcare professionals: a mixed methods study. BMC Med Educ. 2022;22(1):556.
8. Curtin M, Dickerson SS. An Evolutionary Concept Analysis of Precision Medicine, and Its Contribution to a Precision Health Model for Nursing Practice. Adv Nurs Sci. 2022;45(4):10-1097.
9. Fu MR, Kurnat-Thoma E, Starkweather A, Henderson WA, Cashion AK, Williams JK, Katapodi MC, Reuter-Rice K, Hickey KT, de Mendoza VB, Calzone K. Precision health: A nursing perspective. Int J Nurs Sci. 2020;7(1):5-12.
10. Morgan SE, Occa A, Peng W, McFarlane SJ. Evidence‐based communication in clinical, mass media, and social media contexts to enhance informed consent for participation in clinical trials and precision medicine initiatives. In: Berger CR, Roloff ME, eds. The Handbook of Applied Communication Research. Wiley-Blackwell; 2020:897-915.
11. Lebet R, Joseph PV, Aroke EN. CE: Knowledge of precision medicine and health care: An essential nursing competency. Am J Nurs. 2019;119(10):34-42.
12. Smith J, Braithwaite J, O’Brien TA, Smith S, Tyrrell VJ, Mould EV, Long JC, Rapport F. Re-imagining the data collection and analysis research process by proposing a rapid qualitative data collection and analytic roadmap applied to the dynamic context of precision medicine. Int J Qual Methods. 2022;21:16094069221103097.
13. Zatloukal K, Stumptner C, Kungl P, Mueller H. Biobanks in personalized medicine. Expert Rev Precis Med Drug Dev. 2018;3(4):265-273.
14. Fujita K, Masnoon N, Mach J, O’Donnell LK, Hilmer SN. Polypharmacy and precision medicine. Cambridge Prisms: Precision Medicine. 2023;1:e22.
15. Sun S, Ching AH. Social systems matter Precision medicine, public health, and the medical model. East Asian Sci Technol Soc. 2021;15(4):439-466.
FUNDING
No financing.
CONFLICTS OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Conceptualization: Nayana Borah, Vijimol G, Heena Baria.
Methodology: Nayana Borah, Vijimol G, Heena Baria.
Drafting - original draft: Nayana Borah, Vijimol G, Heena Baria.
Writing - proofreading and editing: Nayana Borah, Vijimol G, Heena Baria.