ORIGINAL
Implications for nursing practice on the association between sleep and health outcomes
Implicaciones para la práctica enfermera de la asociación entre el sueño y los resultados de salud
Roma Patel1 ![]() *, Asha Kademane1
*, Asha Kademane1 ![]() *,
Surendra Dadheech3
*,
Surendra Dadheech3 ![]() *
*
1Parul Institute of Nursing, Parul University. Gujarat, India.
2Department of Life Sciences, School of Sciences, JAIN (Deemed-to-be University). Karnataka, India.
3College of Nursing, Teerthanker Mahaveer University. Moradabad, Uttar Pradesh, India.
Cite as: Patel R, Kademane A, Dadheech S. Implications for nursing practice on the association between sleep and health outcomes. Salud, Ciencia y Tecnología. 2023;3(S1):449. https://doi.org/10.56294/saludcyt2023449
Submitted: 11-05-2023 Revised: 30-06-2023 Accepted: 01-08-2023 Published: 02-08-2023
Editor: Dr.
William Castillo-González ![]()
Associate Editor: Fasi
Ahamad Shaik ![]()
ABSTRACT
Between January and December of 2020, a prospective, cross-sectional, observational research was done with 264 nursing staff members, selected among 989 individuals at “Botucatu General Hospital” and stratified by professional type. Sleep quality (SQ) was measured using the Pittsburg Sleep Quality Index (PSQI), while sleep and health were measured using the WHOSAH. A conventional questionnaire was used to obtain expressed characteristics. Means and standard deviations for constant variables and percentages for categorical ones were provided. The correlation coefficient of Spearman’s was used to analyze the strength of relationships. A statistical regression analysis, with age adjustment, was used to assess the link between night shift employment and gender in terms of sleep disruption. P 0,05 was considered significant. When considering age, the association between night shift work and a considerable decline in sleep quality for at least one measure remained substantial. Sleep problems were more common among women. A strong relationship existed between how well you slept and lived. There is a correlation between how well nurses sleep and how satisfied they are with their lives, both of which are influenced by the nature of the nursing profession.
Keywords: Nursing Practice; Sleep and Health; Sleep Quality; Health.
RESUMEN
Entre enero y diciembre de 2020, se realizó una investigación prospectiva, transversal y observacional con 264 profesionales de enfermería, seleccionados entre 989 individuos del “Hospital General de Botucatu” y estratificados por tipo profesional. La calidad del sueño (SQ) se midió con el Índice de Calidad del Sueño de Pittsburg (PSQI), mientras que el sueño y la salud se midieron con el WHOSAH. Se utilizó un cuestionario convencional para obtener las características expresadas. Se proporcionaron medias y desviaciones estándar para las variables constantes y porcentajes para las categóricas. Se utilizó el coeficiente de correlación de Spearman para analizar la fuerza de las relaciones. Se utilizó un análisis estadístico de regresión, con ajuste por edad, para evaluar la relación entre el empleo en turno de noche y el sexo en cuanto a la alteración del sueño. P 0,05 se consideró significativo. Cuando se tuvo en cuenta la edad, la asociación entre el trabajo en turno de noche y una disminución considerable de la calidad del sueño en al menos una medida siguió siendo sustancial. Los problemas de sueño eran más frecuentes entre las mujeres. Existía una fuerte relación entre lo bien que se dormía y se vivía. Existe una correlación entre lo bien que duermen las enfermeras y lo satisfechas que están con su vida, ambos factores influidos por la naturaleza de la profesión enfermera.
Palabras clave: Práctica de la Enfermería; Sueño y Salud; Calidad del Sueño; Salud.
INTRODUCTION
Nurses are the most numerous health care workers in almost every country. Stressful environments, such as those seen in hospitals and clinics, may put a lot of strain on the body and mind of those working there. The necessity to constantly learn new skills to keep up with the rapid evolution of medical care and technology may contribute to the high prevalence of mental health issues among nurses.(1) As a career, nursing has its ups and downs. UK nurses have widespread esteem and a stigma associated with mental illness. The revised nursing proficiency requirements acknowledge that a lack of resilience contributes to poor mental health and aim to remedy the situation. One way to address this issue is by teaching future nurses the value of caring for their mental health as they prepare for careers where they may experience high-stress levels. Because of the high prevalence of mental health issues among both practicing nurses and nursing students, this is crucial. As found among other UK medical students, poor mental health among nursing students may be linked to the stigmatization of those with mental health issues. Nursing learners may have a favorable association between psychological disorders and stigma.(2) Frontline doctors providing care for patients are the most likely to get burned out.
Similarly, close to 60 % of critical care doctors and 60 % of nurses in acute care report feeling burned out. Concerningly, doctors showed higher rates of burnout and dissatisfaction with their existing balance between work and life relative to an average random sample. Depressive disorders, drug misuse, suicidal thoughts, and sleeplessness are only some of the negative health repercussions of burnout identified in the literature. The consequences of burnout for doctors extend even further to the quality of patient care.(3) According to the American Academy of Sleep Medicine's 2005 International Classification of Sleep Disorders, around 20-30 % of shift workers suffer from the illness known as shift work disorder. The typical shift pattern consists of morning, afternoon, and night shifts that rotate continuously. No matter the timetable, the adverse effects on well-being may be traced back to a complicated interplay of inside and outside factors. Shift work is standard in the healthcare industry to guarantee that patients are always cared for. Growing proof suggests that the disruption of natural equilibrium and circadian fall-asleep processes has a profound effect on the wellness and efficiency of medical professionals, potentially endangering the well-being of patients and the security of healthcare workers.(4)
Numerous adverse health effects are associated with the poor sleeping conditions experienced by nurses. Lack of adequate sleep increases nurses' risk of burnout, sadness, and anxiety. Sleep deprivation also has the potential to impair mental abilities, including memory and attention, which might negatively impact both workplace productivity and patient safety. It is crucial to study patterns of poor sleep quality in nurses to allocate health resources, create appropriate therapies, and facilitate the adverse effects of poor sleep. No previous meta-analyses have investigated the global incidence of poor SQ and its related determinants among nursing employees, which prompted the current investigation.(5) Sleep deprivation makes it more likely that nurses may make errors or cause harm to patients since they can't think clearly or react quickly enough. For instance, sleep deprivation has been associated with a higher rate of medication errors among nurses.
Additionally, nurses reported worse quality of life when they had inadequate sleep. Female nurses who rated their quality of life as excellent also rated their SQ as good. Evidence shows that women are more likely to have sleeplessness and sleep disturbances. Inadequate self-care, such as insufficient exercise, has been related to sleep problems and adverse health consequences, including weight gain, persistent disease, and pain.(6) To keep our bodies functioning properly, sleep is a necessary biological process. Insomnia is more common when people are under stress because they have to react quickly to environmental events, which may lead to symptoms including suppressed sleep and increased awake. The most frequent type of sleep condition known as “sleep apnoea-hypopnea syndrome (SAHS)” is obstructive sleep apnoea-hypopnea syndrome (OSAHS).(7) This study discusses the relationship between sleep and health outcomes with implications for nursing practice.
Related works
Many mental and physical wellness disorders may be improved by prolonged lack of sleep, making it difficult to perform at work. The inability of nurses working in various areas of the healthcare system to get a good night's rest may be linked to the stress they experience on the job. However, studies evaluating the prevalence of sleep disorders and their correlation with work stress among Chinese community nurses are uncommon. The study's focus was on Chinese nurses in a community hospital and how their job stress affected the quality of their sleep. We used the Job Stress Questionnaire (also known as the PSQI) to collect data on stress levels in the workplace.(8) The inability to think clearly or respond fast increases the risk of nurses making mistakes or causing injury to patients due to sleep deprivation. It has been shown that nurses who are sleep deprived are more likely to make prescription mistakes. Not enough research has been done on the work–family disputes, sleeping habits, and overall health of nurses working in hospitals, but what has been done is notable. 575 registered nurses working in hospitals around Taiwan were brought on board.
The work-family issues Scale, the PSQI, and the Chinese Wellness Survey were all used during the data collection. We conducted several regression analyses, a Sobel test,(9) and a series of t-tests as well as a chi-squared test. Negative effects on SQ and depression have been linked to working the night shift, which may have serious consequences for both physical and mental health. The study's goals were to compare and contrast the level of sleep and depressed symptomatology of nurses who performed night shifts with those of nurses that worked exclusively day shifts, and to evaluate these relationships among nurses overall. In the careful research, there were a total of 865 registered nurses that participated. Nurses' signs of depression and SQ were evaluated using the Hospital Anxiety and Depression Scale (HADS) and the PSQI respectively.(10) The purpose of the study was to look at how working night shifts affects the health of nurses. A descriptive research approach was used in the study, supplemented by three subjective open-ended questions. Survey Monkey, a method for collecting private data located online and accessible over the internet, was used to gather the data. In the context of this research, the group of interest consisted of registered nurses working in hospitals throughout the United States. The concerns of night shift employees suffering from weariness and ailments linked to tiredness were not taken seriously, according to the respondents.(11)
The purpose of the research was twofold: to determine whether or not there is a correlation between sleep duration and nurse performance, and to characterize the working conditions of licensed nurses in a variety of healthcare settings and types of units. In our study, we took a look backward to see what may have happened. In the United States, acute care hospitals play a key role as both medical and social hubs.The number of hours RNs slept on their days off and at work was the independent variable. Results from the Healthcare Research and Quality's (AHRQ) Hospital Study on Patient Safety Culture and the nurses' perceptions of the standard of the treatment delivered were used to determine variables in the study.(12) The purpose of the study is to determine whether or not workplace context moderates the association between violence at work and three health outcomes. Using the cross-sectional and correlational responses, an additional analysis was performed. The process module in SPSS was used to do mediation-mediated regression analysis on the survey data.(13)
The article suggests two things: (a) proposing solutions that target individual nursing staff, nurse supervisors, and medical care organizations to improve the sleep situation in shift nurses, and (b) briefly reviewing the current studies on shift nurses' sleeping patterns, their sleeping conditions, and the strategies currently implemented in professional environments. Both of these things are intended to enhance the health of shift nurses' sleep. Problems falling asleep during shifts are becoming an increasingly acknowledged serious concern at both personal and managerial levels among nurses working in shift work. But the answers to these problems are not well recognized.(14) Using the Pittsburgh SQ Index (PSQI), researchers estimated that around 21 percent of the study's nurses likely had insomnia. Poor SQ was also reported by nurses working during the COVID-19 epidemic. Many managers have switched to more flexible work structures to help guarantee that nurses get enough sleep, although 8-hour shifts continue to be necessary. Nurses in high-stress environments like ICUs or isolation wards may find their sleep schedules severely disrupted by doing shift work. During the COVID-19 epidemic, caregivers have been working shorter hours more often to minimize their daily exposure to high-risk regions and to lessen the inconvenience of wearing PPE. However, there is evidence that more frequent shifts are linked to lower-quality sleep.(15)
Professional Nurses and the Phenomenon of Sleep Deprivation and Nonstandard Work Schedules
Due to competing factors increasing expectations for superior patient care and the worldwide trend of health-systems budget limitations necessitating maxi-mum efficient operation with minimal staffing, nursing shifts have become more atypical in recent years. As a result, twelve-hour changes, or longer, which first appeared at the end of the 1980s, have become standard practice in the nursing profession, making for a very taxing workplace for nurses. They must care for many clients without enough rest during shifts and frequently without pauses or rest periods during working hours. As a result, many people in the nursing field feel burned out and question their ability to make good decisions to provide sufficient treatment for patients.
As a result of the staffing crisis, the surviving nurses have to put in more hours, and the burden keeps growing. Despite regulations and even laws in some countries (the United States of America) restricting the shift length to 12 hours and avoiding extra hours with the exception in crucial situations, they function with a great deal of flexibility, depending on the approval of the healthcare facility or the decisions taken by nurses amongst themselves about more working hours. It is acceptable for nurses to work unregulated overtime if needed. Their 12-hour shift is more like 13 hours long because of things like paperwork, admitting new patients, reporting shift handovers, helping others, increasing salary, and accruing vacation days.
Hospital nurses have work-related sleep issues due to inconsistencies between their natural circadian rhythms, the time demands of their jobs, and other factors. Disrupting the circadian cycle and leading to sleep issues and weariness, atypical scheduling arrangements of nursing staff include things like continuous overnight shifts, shift work patterns with a high percentage of night shifts, and brief rest periods between shifts at work. According to the research conducted at the Emergency Centre of Vojvodina, the level of work-related weariness also influences drowsiness in nurses. In truth, shift workers' work and sleep schedules often clash with the norms of society and the human body.
Not everyone will have an impact on their quality of sleep, but those that do will likely see it mediated by the same variables that affect their overall tolerance or susceptibility. Individual variations may be broken down into two categories are represented in figure 1:
· "Fixed" elements connected to stable genetic, demographic, and psychological features and
· "Variable" circumstances that rely on the current situation.
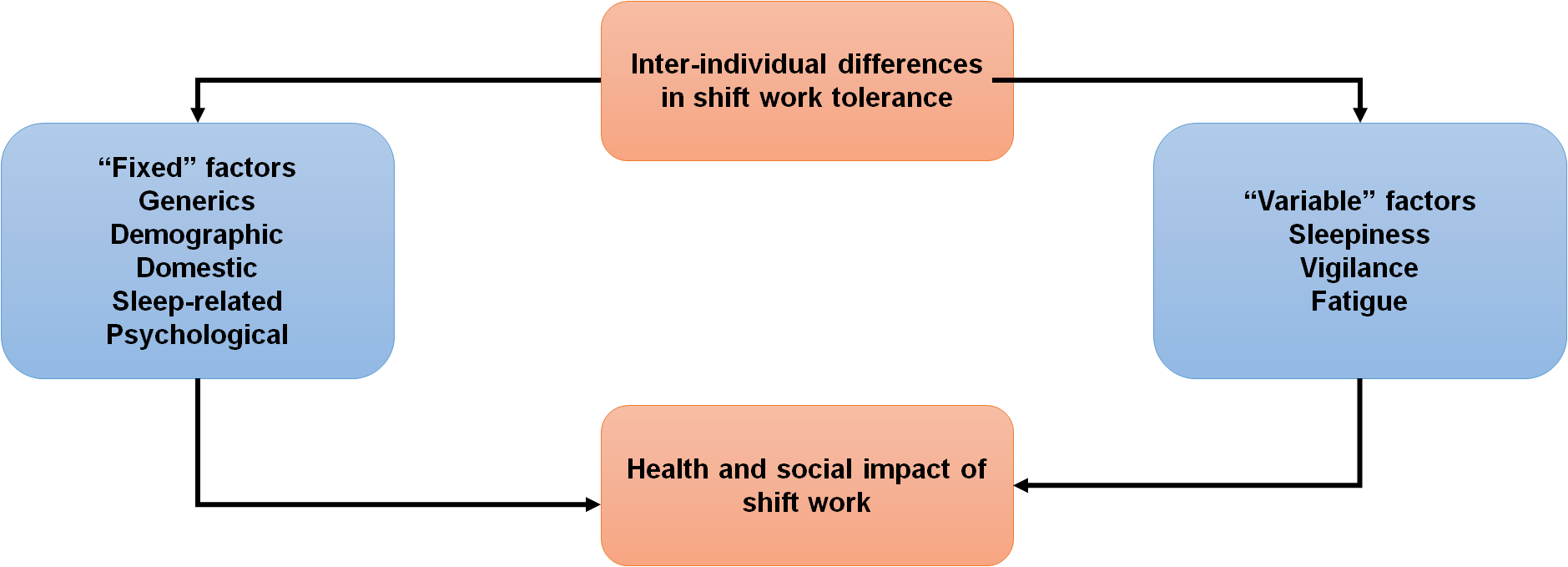
Figure 1. Fixed and Variable inter-individual factors potentially explaining the impact of health and sleep
Nursing Practice on health outcomes
The implications for nursing practice on health outcomes are extensive and include a variety of angles and perspectives. Nurses play an essential part in promoting and enhancing health outcomes within a wide range of healthcare environments. The following are some crucial ramifications for nursing practice in connection to the results of health assessments:
Instruction and advocacy of health Nurses are at the forefront of health instruction and promotion. They can impart vital information to clients on the avoidance of illness, the selection of healthy lifestyle behaviors, and the execution of self-care procedures. Nurses can encourage patients to make educated choices and take responsibility for their health by teaching clients good habits, eventually leading to better medical results.
Immunizations, screenings, and health evaluations are all examples of how nurses contribute significantly to the early identification and prevention of illness. They can identify those at risk, provide immunizations, perform checks for diseases such as diabetes, high blood pressure, or malignancy, and administer screenings. Nurses may play an important role in halting the course of illnesses, lowering the risk of complications, and achieving better overall health if they emphasize the need for early identification and preventative care.
Coordination and management of patient care: Nurses often take on the role of care coordinators and collaborate with multidisciplinary healthcare teams to effectively manage their care. They do patient needs assessments, design care plans, monitor treatment adherence, and enable communication between different sources of medical care. Nurses may enhance general health, maximize the effectiveness of therapy, and lower the number of times patients need to be readmitted to the hospital by coordinating care effectively.
When it comes to medication management, nurses are the ones who are in charge of giving patients their drugs and instructing them on how to take them correctly. They ensure the prescription is taken as prescribed, watch for unpleasant effects, and offer details on drug combinations. The ability of nurses to effectively manage medicine may significantly influence individuals' health by increasing the efficacy of treatment and reducing the risk of problems connected to drug use.
Advocacy for Patients Nurses advocates for their patients, ensuring their rights are honored, and their opinions are heard. They work as an interface between patients and those in charge of healthcare, assisting patients in understanding the many treatment choices available to them and making decisions based on accurate information. Nurses can contribute to better health outcomes and improved client satisfaction by advocating for patient-centered treatment and facilitating effective interaction.
Management of chronic diseases is a common aspect of a nurse's employment since they often interact with patients afflicted with disorders such as diabetes, heart disease, or asthma. They help patients negotiate the intricacies of their conditions by providing knowledge, supporting self-management techniques, and assistance. Nurses are uniquely positioned to assist patients in adequately managing their persistent illnesses, reducing the risk of problems, and enhancing their quality of life. Continual monitoring, lifestyle changes, and treatment regimen compliance may accomplish.
In conclusion, nursing practice significantly influences the final results of health assessments. Nurses make a significant contribution to improving overall health outcomes and enhancing patients' well-being via the provision of care that includes promoting health, preventing illnesses, coordinated care, lobbying for patients, managing chronic diseases, psychological assistance, and hospice care.
METHODS
Cross-sectional design for descriptive purposes researchers in this study gave nurses a self-made checklist measuring their patient-care skills and their level of sleepiness to see whether or not there was a connection between the two.
A prospective, longitudinal qualitative study was conducted at an academic medical center in “Botucatu, SP, Southeast Brazil between January and December of 2020”. The study population consisted of 182 RNs, 222 LTs, and 285 aides among the 989 employees of the University Hospital of the “Botucatu Medical School ”. Shifts ran from 7:00 AM to 4:00 PM, 2:00 PM to 11:00 PM, and 11:00 PM to 7:00 AM, respectively. Throughout these times, the hospital's staffing fluctuated at will to meet the changing demands of the facility and its employees. The 989 nurses were dispersed throughout the hospital and assigned to various departments such as emergency rooms, operating rooms, units for intensive care, post-anesthesia care units, dialysis centers, and school health centers to offer nursing assistance. The sample size was determined using the following assumptions: = 5,0 %, a PSQI score > 5 in 20 % of the humanity, and stratification by occupational category (n = 989 nurses). A total of 250 healthcare workers, comprising 46 nurses, 146 aides, and 58 technicians, were included in the study.
Volunteers were initially chosen randomly and then accepted into the study if they consented to participate. Maternity and an absence from work of less than four weeks were ruled out for participation. The final analysis did not include all participants' responses due to incomplete questionnaires. Those who answered all 12 PSQI questions (n = 226) were used to determine the total score.
Data Set
The PSQI was used to measure SQ, the WHOSAH was used to evaluate wellness, and an ordinary survey was used to collect demographic information. The seven-factor PSQI has been vetted for use with the Brazilian population. Insomnia latency, duration of sleep, sleep effectiveness, sleep disorders, use of sleep medicine, morning dysfunction, and dependent SQ. The total score is determined by adding the results from the seven subscores. The least good maximum on a Likert-type scale is 3. Therefore, scores between 0 and 3 are all given equal importance. From 0 to 21, a score of 5 indicates a high-quality number; 4-15 indicates severe sleep disruption. The results of the WHOSAH, a self-assessment tool considering the previous two weeks of experience, were used to generate scores. The questionnaire covers four primary areas: (i) physiological, (ii) mental, (iii) interpersonal, and (iv) ecological. There is a 5-point Likert scale used to score each item. The health domain score may be anything from 0 to 100.
The PSQI was used to measure SQ, the WHOSAH was used to evaluate wellness, and an ordinary survey was used to collect demographic information.
Average and standard deviations are shown for continuous variables, whereas proportions are used to represent categorical ones. The association between SQ ratings and quality of life was analyzed using the Spearman's correlation coefficient. The correlation between nighttime work, gender, and sleep disturbance was analyzed using linear regression, with age as an independent variable and significant disruption in at least one component of the PSQI as the dependent variable. The level of statistical significance used in all of the tests was 0,05.
Pittsburgh Sleep Quality Index (PSQI)
The PSQI was used to assess nurses' reports of their SQ throughout the preceding month. There are 19 questions total, and they cover seven different aspects of sleep: how you feel about your sleep, how long you get to sleep, how well you sleep on average, what causes disruptions in your sleep, what sleep aids you to take, and how your day goes. A Likert scale is used to rate each dimension. If your overall score is more significant, your SQ is terrible. With a sensitivity of 98 % and specificity of 55 %, a PSQI score of >5 indicates insufficient sleep. Adults living in the community showed satisfactory test-retest reliability of the PSQI at 2-3 weeks after the first administration.
RESULT
Stratified proportionately into three groups, 270 nursing professionals (53 nurses, 61 PNs, and 152 NTs) participated in this research. The average age was 42, with a standard deviation of 11,2 years, are explained in table 1.
|
Table 1. Demographic data |
||||
|
|
Nurse (N = 53) |
Nursing assistant (N = 61) |
Nurse technician (N = 153) |
Total (N = 270) |
|
Age (years)a |
37(11,0) |
34 (8,9) |
45 (10,1) |
42 (11,2) |
|
Gender (Male/Female) |
5/49 |
3/59 |
30/124 |
36/230 |
|
Other jobs (Yes/No/NI) |
9/45/0 |
15/47/0 |
17/136/1 |
39/226/1 |
|
Overtime (Yes/No/NI) |
6/48/0 |
29/33/0 |
81/71/2 |
114/150/0 |
|
Shift (Day/Night/NI) |
45/8/1 |
35/27/0 |
122/28/4 |
200/61/6 |
|
Working hours (30h/40h/NI) |
7/46/1 |
3/59/0 |
23/126/5 |
31/229/6 |
Gender had no effect on quality of life, but age did (R = -0,15; p = 0,019) on the physically-focused subscale). Working nights had no effect on WHOSAH ratings, although overtime did influence scores in the environment domain (R = 0,19; p = 0,004) are represented in table 2. Professionals' regular workweeks were associated with the social domain, and overtime with the environmental domain. There was a correlation between education and quality of life, but not with the other factors.
|
Table 2. Domains of health and demographic factors: a correlation analysis |
|||||
|
Variable |
|
Physical |
Psychological |
Social |
Environmental |
|
Gender (Male/Female) |
Coefficient (p) |
-0,11 |
-0,07 |
-0,04 |
0,01 |
|
|
|
0,0826 |
0,2393 |
0,4765 |
0,8613 |
|
|
N |
258 |
253 |
257 |
257 |
|
Age (Years) |
Coefficient (p) |
-0,15 |
0,01 |
-0,004 |
-0,03 |
|
|
|
0,0195 |
0,8655 |
0,9540 |
0,6484 |
|
|
N |
258 |
253 |
257 |
257 |
|
Overtime (Yes/No) |
Coefficient (p) |
-0,02 |
-0,04 |
0,04 |
0,19 |
|
|
|
0,6872 |
0,5546 |
0,5634 |
0,0048 |
|
|
N |
256 |
251 |
255 |
255 |
|
Working hours (30h/40h) |
Coefficient (p) |
-0,03 |
-0,02 |
-0,12 |
-0,08 |
|
|
|
0,6358 |
0,7178 |
0,0481 |
0,1904 |
|
|
N |
252 |
247 |
251 |
251 |
The physical domain had the lowest score on the WHOSAH (58,7, with a standard deviation of 16,0), while the social interactions area received the most significant score (68,8, with a standard deviation of 19,5). The scores for the physical and psychological domains, respectively, were 67,4 (standard deviation equal to 19,5) and 66,3 (standard deviation equal to 18,5) are represented in table 3.
|
Table 3. WHOSAH domain scores |
||||||
|
Variable |
N |
Mean (SD) |
SD |
Minimum |
Maximum |
Median |
|
Physical |
258 |
67,4 |
19,5 |
4,58 |
100 |
65,7 |
|
Environment |
257 |
58,7 |
16,0 |
13,62 |
100 |
60,5 |
|
Psychological |
253 |
66,3 |
18,5 |
9,44 |
100 |
67,8 |
|
Social relations |
257 |
68,8 |
19,5 |
0 |
100 |
76,1 |
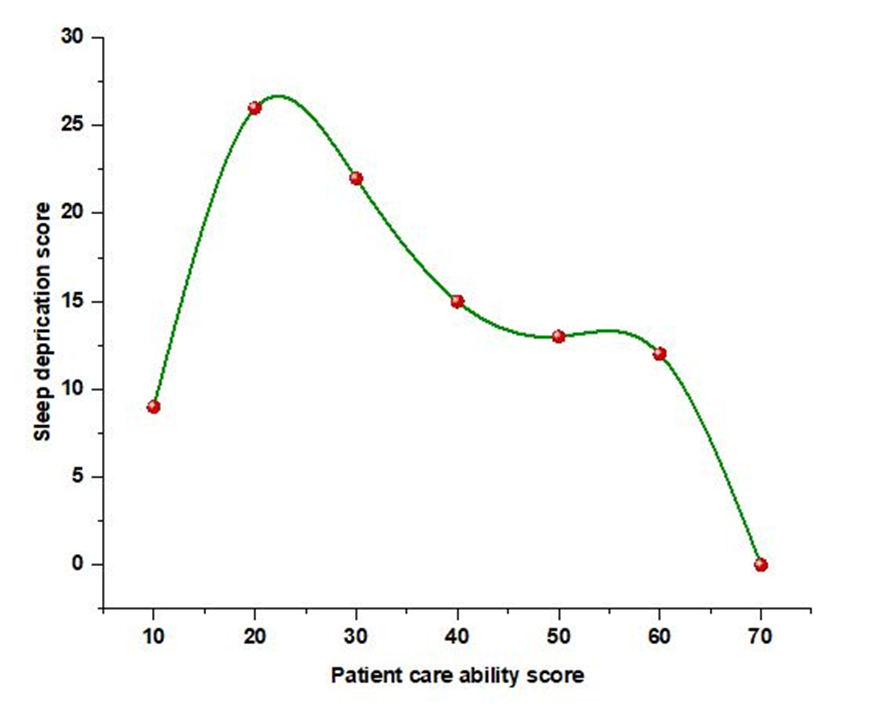
Figure 2. Correlation between sleep deprivation and patient care ability
The relation between sleep deprivation and patient care abilities among nurse is represented in figure 2. When the patient care ability score increases sleeping rate decreased, it means nurse sleep rate is disturbed. The highest patient ability score 70 reflects the least sleep deprivation score. The lowest patient care ability score is 10 meets the score 8.
CONCLUSIONS
Since nurses make up the bulk of the medical staff, and shift work is necessary to maintain patient safety and continuity of care, it is crucial to foster a safe working environment for them. Certainly, it is a huge difficulty for healthcare businesses to accomplish perfect night shifts administration. However, everyone in the area, from individual workers and patients to the whole healthcare system, could benefit from the rewards.
REFERENCES
1. Bazazan A, Dianat I, Mombeini Z, Aynehchi A, Jafarabadi MA. Fatigue as a mediator of the relationship between quality of life and mental health problems in hospital nurses. Accident Analysis & Prevention. 2019;126:31-36.
2. Kotera Y, Cockerill V, Chircop JG, Forman D. Mental health shame, self-compassion and sleep in UK nursing students: Complete mediation of self-compassion in sleep and mental health. Nursing open. 2021;8(3):1325-1335.
3. Stewart NH, Arora VM. The impact of sleep and circadian disorders on physician burnout. Chest. 2019;156(5):1022-1030.
4. Alfonsi V, Scarpelli S, Gorgoni M, Pazzaglia M, Giannini AM, De Gennaro L. Sleep-Related problems in night shift nurses: towards an individualized interventional practice. Frontiers in Human Neuroscience. 2021;15:644570.
5. Zeng LN, Yang Y, Wang C, Li XH, Xiang YF, Hall BJ, Ungvari GS, Li CY, Chen C, Chen LG, Cui XL. Prevalence of poor sleep quality in nursing staff: a meta-analysis of observational studies. Behavioral sleep medicine. 2020;18(6):746-759.
6. Kim-Godwin YS, Lee MH, Logan JG, Liu X. Factors influencing sleep quality among female staff nurses during the early COVID-19 pandemic in the United States. International Journal of Environmental Research and Public Health. 2021;18(9):4827.
7. Zhuo K, Gao C, Wang X, Zhang C, Wang Z. Stress and sleep: a survey based on wearable sleep trackers among medical and nursing staff in Wuhan during the COVID-19 pandemic. General psychiatry. 2020;33(3).
8. Deng X, Liu X, Fang R. Evaluation of the correlation between job stress and sleep quality in community nurses. Medicine. 2020;99(4).
9. Cheng SY, Lin PC, Chang YK, Lin YK, Lee PH, Chen SR. Sleep quality mediates the relationship between work–family conflicts and the self‐perceived health status among hospital nurses. Journal of nursing management. 2019;27(2):381-387.
10. Dai C, Qiu H, Huang Q, Hu P, Hong X, Tu J, Xie Q, Li H, Ren W, Ni S, Chen F. The effect of night shift on sleep quality and depressive symptoms among Chinese nurses. Neuropsychiatric disease and treatment. 2019;15:435-440.
11. Books C, Coody LC, Kauffman R, Abraham S. Night shift work and its health effects on nurses. The health care manager. 2020;39(3):122-127.
12. Stimpfel AW, Fatehi F, Kovner C. Nurses' sleep, work hours, and patient care quality, and safety. Sleep Health. 2020;6(3):314-320.
13. Havaei F, Astivia OLO, MacPhee M. The impact of workplace violence on medical-surgical nurses’ health outcome: A moderated mediation model of work environment conditions and burnout using secondary data. International journal of nursing studies. 2020;109:103666.
14. Sun Q, Ji X, Zhou W, Liu J. Sleep problems in shift nurses: A brief review and recommendations at both individual and institutional levels. Journal of nursing management. 2019;27(1):10-18.
15. Liu Y, Jiang TT, Shi TY, Liu YN, Liu XM, Xu GJ, Li FL, Wang YL, Wu XY. The effectiveness of diaphragmatic breathing relaxation training for improving sleep quality among nursing staff during the COVID-19 outbreak: a before and after study. Sleep Medicine. 2021;78:8-14.
FUNDING
No financing.
CONFLICTS OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Conceptualization: Roma Patel, Asha Kademane, Surendra Dadheech.
Methodology: Roma Patel, Asha Kademane, Surendra Dadheech.
Drafting - original draft: Roma Patel, Asha Kademane, Surendra Dadheech.
Writing - proofreading and editing: Roma Patel, Asha Kademane, Surendra Dadheech.