ORIGINAL
Nursing Practice Improvement Strategies for Reducing Medication Errors
Estrategias de mejora de la práctica enfermera para reducir los errores de medicación
Malathi Hanumanthayya1 ![]() *,
Basavaraj Mudhol2
*,
Basavaraj Mudhol2 ![]() *,
Varsha Agarwal3
*,
Varsha Agarwal3 ![]() *
*
1JAIN (Deemed-to-be University), Department of Life Sciences. Karnataka, India.
2Teerthanker Mahaveer University, College of Nursing. Moradabad, Uttar Pradesh, India.
3ATLAS SkillTech University, ISME - School of Management & Entrepreneurship. Mumbai, India.
Cite as: Hanumanthayya M, Mudhol B, Agarwal V. Nursing Practice Improvement Strategies for Reducing Medication Errors. Salud, Ciencia y Tecnología. 2023;3(S1):454. https://doi.org/10.56294/saludcyt2023454
Submitted: 06-06-2023 Revised: 13-07-2023 Accepted: 01-08-2023 Published: 02-08-2023
Editor: Dr.
William Castillo-González ![]()
Associate Editor: Fasi
Ahamad Shaik ![]()
ABSTRACT
The safety of the patient is put at risk by medication mistakes, particularly during administration. In order to achieve Joint Commission International (JCI) certification, a Chinese hospital undertook research to lower medication errors (MEs). Comprehensive interventions were carried out, and the number of MEs fell by 58,3 % between the first half of 2016 and the first half of 2018. During the same time frame, there was a 55,6 % drop in high-alert drug mistakes. The majority of mistakes were omissions, which decreased by 50 %. Errors in intravenous administration also declined. Nurses with more experience made fewer mistakes, and surgical wards had twice as many mistakes as medical wards. ME rates were greater in intensive care units. In order to improve pharmaceutical safety, the study emphasized the value of teamwork among healthcare professionals, including doctors, chemists, nurses, information engineers, and administrators. It was discovered that JCI certification enhanced MEs awareness, prevention, and quality enhancements. Overall, the study supported the 3-and-a-half-year intervention program’s ability to reduce MEs.
Keywords: Medication Errors (MES); Nursing; Quality Improvements; Practice; Management.
RESUMEN
Los errores de medicación, sobre todo durante su administración, ponen en peligro la seguridad del paciente. Para lograr la certificación de la Joint Commission International (JCI), un hospital chino emprendió una investigación para reducir los errores de medicación (EM). Se llevaron a cabo intervenciones integrales, y el número de EM se redujo en un 58,3 % entre el primer semestre de 2016 y el primer semestre de 2018. Durante el mismo periodo de tiempo, se produjo un descenso del 55,6 % en los errores de medicación de alerta elevada. La mayoría de los errores fueron omisiones, que disminuyeron un 50 %. También disminuyeron los errores en la administración intravenosa. Las enfermeras con más experiencia cometieron menos errores, y las salas quirúrgicas tuvieron el doble de errores que las salas médicas. Las tasas de EM fueron mayores en las unidades de cuidados intensivos. Para mejorar la seguridad farmacéutica, el estudio hizo hincapié en el valor del trabajo en equipo de los profesionales sanitarios, incluidos médicos, químicos, enfermeras, ingenieros informáticos y administradores. Se descubrió que la certificación de la JCI mejoraba la concienciación, la prevención y la calidad de los EM. En conjunto, el estudio respaldó la capacidad del programa de intervención de tres años y medio para reducir las EM.
Palabras clave: Errores de Medicación (EM); Enfermería; Mejoras de la Calidad; Práctica; Gestión.
INTRODUCTION
The administration of medications is a crucial part of providing healthcare, and mistakes here can have serious repercussions for patient safety. The frontline healthcare workers that administer medications to patients in hospitals are the nursing staff. However, medication administration errors (MEs) continue to be a major problem in healthcare settings, endangering patients' health and the standard of care as a whole.(1) Initiatives for quality improvement that lower MEs have received more attention in recent years. Due to their emphasis on research, education, and high-quality care, academic medical center hospitals have emerged as key locations for the implementation of methods to improve pharmaceutical safety. In an academic medical center hospital context, this introduction gives a broad overview of the significance of addressing MEs and the value of quality improvements.(2) Medication mistakes are a common problem in healthcare, and when they happen during the administration process, they can result in adverse drug events, patient injury, longer hospital stays, and higher healthcare expenses. According to numerous studies, MEs are responsible for a sizeable share of adverse occurrences in hospitals. For patient safety to be improved, as well as the quality of healthcare as a whole, the root causes of these errors must be found and addressed. Nursing staff plays a significant role in drug safety initiatives as they are primarily in charge of giving patients their medications. They are essential to ensuring appropriate medicine administration because they calculate dosage, use the right technique, and follow prescriptions. However, there are a number of variables that can increase the risk of MEs among nursing personnel, including a heavy workload, complicated drug schedules, disruptions, and poor communication.(3)
Hospitals affiliated with academic medical centers offer distinctive healthcare settings where patient care, instruction, and research come together. These organizations frequently use multidisciplinary teams, cutting-edge technology, and evidence-based procedures. Academic medical centers are in a good position to execute quality improvement programs targeted at lowering MEs and improving patient safety since they are centers of innovation.(4) Exploring novel approaches, conducting research, and sharing best practices for medication administration are made possible by the integration of research and education with clinical treatment. Initiatives for quality improvement seek to systematically address and minimize errors in healthcare procedures, including the administration of medication. Academic medical center hospitals should work towards a culture of safety that prioritizes patient well-being by applying evidence-based practices, encouraging interdisciplinary collaboration, and utilizing technology solutions. In addition to reducing errors, quality improvements in medicine administration can increase productivity, encourage standardization of practices, and boost employee confidence and morale.(5)
Trakulsunti et al.(6) was to illustrate, through the use of four case studies, the application of Lean Six Sigma (LSS) to decrease pharmaceutical mistakes. In order to enhance the medical process, the paper will also recommend suitable Lean and Sigma tools. To assess the effectiveness of professional, organizational, and structural changes to the usual level of care in reducing primary care providers' avoidable prescription mistakes that result in adult hospitalizations, ER visits, and death.(7) Farzi et al.(8) was to investigate and characterize the factors that lead to medication mistakes in intensive care units (INTENSIVE CARE UNITs) from the viewpoints of nurses, physicians, and pharmacists in clinical practice. Hammoudi et al.(9) evaluated the elements from the nurse's perspective that affect the likelihood and reporting of prescription mistakes. Naseralallah et al.(10) assessed statistically and subjectively the effects of clinical chemist treatments on pediatric hospitalized patients' medication error levels. In order to better the nurses' proper use of EMMS in two Australian hospitals, this study employs the Theoretical Domains Framework (TDF) to pinpoint obstacles and provide focused treatments.(11) Robertson et al.(12) was to (1) discuss how medical errors affect the involved vendors, (2) list possible explanations for why medical errors might have an adverse impact on vendor psychological well-being, and (3) offer recommendations for how vendors and healthcare organizations can recognize and lessen the adverse impacts that medical errors have on vendors. Assiri et al.(13) was to evaluate the epidemiology of medication mistakes and adverse events associated with errors that occurred in individuals while receiving primary health care, ambulatory healthcare, or medical treatment in their homes. Wei et al.(14) is to determine, evaluate, and summarize the main themes of research on nurse workplaces in the US that were published between January 2005 and December 2017, as well as to offer suggestions for how to make such situations better. Walsh et al.(15) was conducted with the intention of describing and quantifying the financial impact that is connected with drug errors. The purpose of this paper is to explore how beneficial such stewardship treatments are in inpatient care and offer some reference material for overseas equivalents.
The remainder of the paper is divided into subsequent parts. Part 2 contains the method explained. Part 3 contains the result. Part 4 discusses the conclusions.
METHODS
Collection of data
In BIMC, a hospital with 2900 beds, 2,4 million visits from outpatients, and 70 000 patients discharged every year (data from 2017), a treatment program that focused on MEs in inpatient nursing care was carried out over the course of three and a half years. This hospital is located in the Bali region, People's of Indonesia, which has a populace of nearly 35,6 million people. A mandatory electronic medication error reporting system known as BIMC was in place from January 2015 to June 2018, and it was used to compile data on the number of MEs that occurred every six months among nursing personnel. A data extraction operation was carried out, with the primary attention being placed on the different types of MEs, severity ratings, high-alert drugs occupied, management routes, times of incidence and recognition of MEs, ward distributions, and nursing qualifications.
|
Table 1. Benner's Model, NCC MERP, and Professional Titles |
||
|
Professional Title |
Benner’s Model |
NCC MERP Category |
|
Major charge nurse |
Expert Nurse (N4) |
N/A |
|
Nurse Practitioner |
Proficient Nurse (N3) |
N/A |
|
Nurse |
Competent Nurse (N2) |
N/A |
|
|
Advanced Beginner (N1) |
N/A |
|
|
Novice (N0) |
N/A |
|
Type-I Errors |
N/A |
Although errors reached the individual, they didn't hurt the individual in question. |
|
Type-II Errors |
N/A |
Errors happened that reached the patient and necessitated surveillance to make sure the individual wasn't harmed and/or treatment to prevent damage. |
|
Type-III Errors |
N/A |
Errors happened that may have led to or caused the individual's temporary injury, necessitating action, a beginning hospital stay, or both. |
|
Type-IV Errors |
N/A |
Errors happened that needed action to maintain life, errors requiring treatment to prevent lasting patient injury, and mistakes that might have caused or contributed to patient death. |
The Drug and Therapeutics Committee (DTC) of BIMC records contain the information that was given in the research. The BIMC DTC must grant access to and use of these data.
Comprehensive Intervention Measures
Quality enhancing resources: "Plan-do-check-act (PDCA)," "quality control circles (QCCs)," and "continuous quality improvement (CQI)" were all used as quality improvement tools. The separation of Nursing ran 1 289 quality development programs from 2015 to 2019; these included 1 123 PDCA, 176 QCCs, and 88 CQIs. There were 99 programs pertaining to medications, 69 of which were devoted to ME prevention (figure 1).
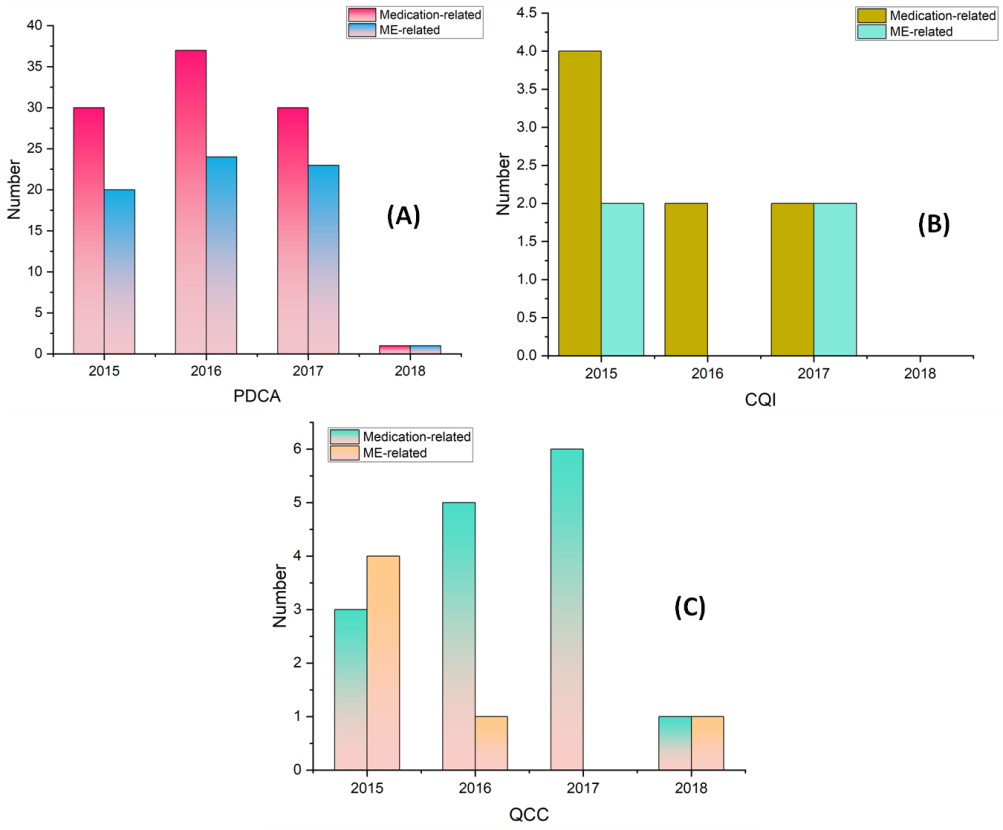
Figure 1. Medication- or ME-related quality improvement
Organizational measures
The Division of “Nursing’s Committee of Quality and Safety Administration” formed the Section of Safe Medication Administration in 2015, with ten head nurses serving as its core members. A three-level stewardship mechanism for secure medication administration was established in the January-June of 2016. It consists of monthly on-site inspection of medication administration inwards by inpatient pharmacy technicians, biannual self-evaluations by each nursing unit, and annual checking by the Division of Secure medication management. Additionally, in June 2015, BIMC created 16 functional groups in accordance with JCI certification requirements. The worldwide patient safety objective group and the pharmaceutical usage and administration group both contributed significantly to quality enhancements and the security of patients. The Office of Quality Management, Therapeutics Committee and Pharmacy, and Division of Nursing all conducted quarterly meetings to discuss the security of medications. If required, sessions for multidisciplinary cooperation and brainstorming were convened. The summaries of every meeting were all recorded. A tracing mode was initially implemented in medication administration, use, and nursing quality evaluation at the beginning of 2017. Case tracking and systematic tracing were coupled to raise patient safety understanding among doctors, chemists, logisticians, nurses, and data technologists, as well as to make it simpler for executives to identify systemic issues in inpatient healthcare.
IT Controls
1. Monitoring medications electronically. This system was implemented in June 2015 using digital nursing reference technology and pharmaceutical management data. It was distinguishable for suggesting, documenting, prescribing the auditing process, sterile mixing, transportation shipment, and wards nurses acquiring drugs, doses, and IV infusions, resulting in a potent instrument for process management in managing doctor's orders. Every nursing facility received an audio device in November 2015 that informed employees of ST Doctor's instructions. If the nurses do not respond, the alarm will sound once more in one minute. For ST medications, the hospital pharmacy raised the alert.
2. Creating an internet search system for tablet or capsule appearance. This platform, which was launched in June 2015, was very helpful to nurses when it came to monitoring medicine or locating the relevant prescriptions that the doctor had ordered but had temporarily stopped prescribing.
3. Creating online software for drug counseling and medication monitoring. In October 2015, such a system was launched and integrated with the electronic medical record (EMR), digital nursing reference structure, and pharmacy management database. Through this program, nurses may simply check on essential drug knowledge.
4. Creating a unit dosage labeling system that complies with JCI guidelines. As of July 2016, a unit dosage card comprising a QR code, the patient's name, an identifying number, drug details, and warnings was attached to every prescription filled by the inpatient pharmacist.
5. Establishing a thorough JCI-compliant pharmacy management information system gateway for medication tracking. Such a system was created in January 2017. Since that time, trained chemists have assessed orders from doctors based on information that was available as of the final day of 2016 as well as other significant information.
6. Growing IT spending on nursing care. PDAs and portable nursing carts were introduced in June 2015 in a number of BIMC wards. Each nursing unit had four to 8 PDAs and 3 to 4 mobile nursing carts, for a sum of 220 and 117, in the second half of 2016. While accurate medication label information and barcode scanning before administration were deemed to increase pharmacological safety, portable nursing carts made nurses' lives simpler.
|
Table 2. Process Optimization |
||
|
Process Optimization |
Date Implemented |
Details |
|
Centralized IV Admixture |
November 2014 |
Apart from the critical care unit, emergency intensive care unit, and neurological intensive care unit, all wards are supplied by the inpatient pharmacist. |
|
Extended IV Admixture |
October 2016 |
Emergency, Intensive care unit and Neurological intensive care units received centralized IV admixture service. |
|
No High-Concentration Electrolyte Storing |
October 2016 |
Pharmacy-only storage of high-concentration electrolytes |
|
Ready-to-Use Infused Sleeves |
October 2016 |
Inpatient pharmacies provide potassium chloride infusion bags. |
|
Unit Dose Mode Strengthened |
January 2015 |
Inpatient pharmacies provide potassium chloride infusion bags. |
|
24/7 Pharmacy |
Beginning of 2016 |
Inpatient pharmacy began 24/7 pharmaceutical treatment. |
|
Table 3. Process Optimization in Each Ward: Standardized Procedures and Checks |
|
|
Process Optimization |
Details |
|
Reorder the doctor's orders |
- Timely printing and a consistent quality-control procedure |
|
- Within an hour after printing the change order, the primary nurse must review and sign the physician order. |
|
|
- Change order signed and to be retained for three months |
|
|
Micro-pump Sustained Infusion |
- The infusion must be administered by the primary nurse in accordance with the execution sheet of the doctor's directions. |
|
- Every shift nurse must sign the procedure page after confirming the injection label and infusing speed. |
|
|
Standardized Double-Check for Medications for High-Alert |
- Before providing any particular high-alert drugs, double-check at the bedside. |
|
- Beginning with the second half of 2016, the implementation |
|
|
- Using a PDA to capture the two operators' identity details throughout the operation for process traceability if necessary |
|
Intensified human resource management and educational measures: One hundred ten nurse positions had revised in 2017. The analytical weight assigned to work efficiency when assessing particular nursing abilities was increased by 35 %. Each nursing unit's staff members were maximized. In each nursing unit, there were two groups. A nurse group leader was assigned to each group. Each primary nurse was assigned to oversee a group of rooms for a continuous two weeks. It was built with a good nursing qualification administration. For each nurse, a professional growth dossier was created. The Division of Nursing worked on strengthening the individualized management strategy and increasing the nursing staff's understanding of managing oneself. Multi-level education was planned for nurses with varying levels of experience in nursing in accordance with Benner's beginner-to-specialist method. Since the start of 2017, the separation of Nursing has been offering annual training courses for N0 (10 hrs), N1 (10 hrs), N2 (10 hrs), N3 (11 hrs), and other nursing staff (7 hrs). Doctors visited a sequence of lectures on wise drug use every year and got specialized training on how to write orders utilizing an EMR.
Outcomes Measures
The result metrics consisted of the number of MEs made by nurses, the frequency of MEs, the number of MEs connected with high-alert medications, the frequency of MEs associated with high-alert medications, the frequency of absence, the trends of MEs with various seriousness ratings, the management path, the frequency and timing of ME recognition, and the relative proportion of specific ME types.
Statistical Analysis
There was a descriptive analysis done. The program SPSS (v 13,0) was used to assess the variations in occurrence rates between the two groups. When two (45 %) of an emergency table's cells had an anticipated count lower than five, Fisher's exact test was utilized. When one cell (20 %) had an anticipated count below five, Pearson's chi-square continuity correction was utilized. When there was an anticipated count of fewer than five in 0 cells (0 %), Pearson's chi-square was utilized. Statistical significance was defined as a P-value < 0,05.
RESULTS
From the January-June of 2015 to the January-June of 2016, there was an increase in the number of MEs. The incidence rates of MEs over this time, however, did not change statistically significantly (P < 0,05). Nursing personnel consistently reduced the number of MEs from 123 to 56 during the January-June of 2016 and the January-June of 2018. In BIMC, the number of patients who were discharged climbed consistently from 32 810 in the January-June of 2015 to 47 286 in the January-June of 2018, whereas the frequency of MEs performed by nursing staff reduced by 47,5 % (figure 2).
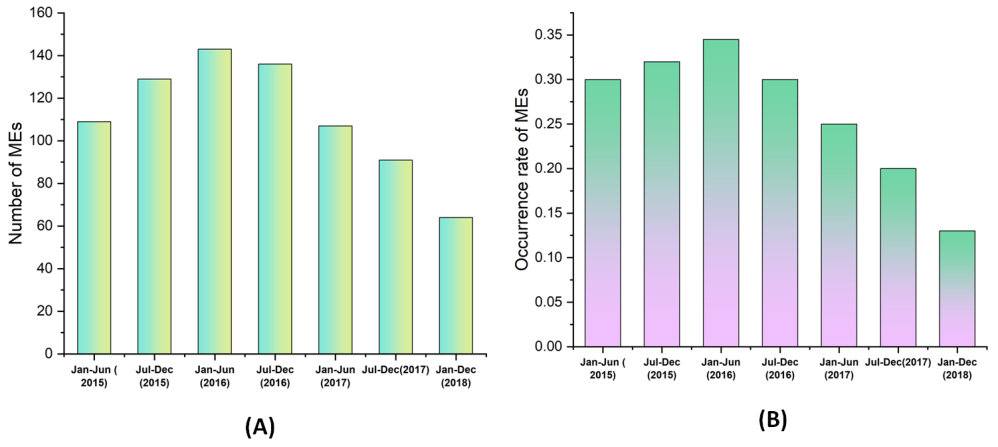
Figure 2. MEs performed by nursing personnel between January 2015 and June 2018
Between 2015 and 2018, venous exosmosis (0,5 %) and inappropriate processing of computerized physician prescriptions before transmitting them to inpatient pharmacies accounted for 1,7 % and 0,5 %, respectively, of all MEs. Omission accounted for 31,7 % of all MEs. Between the January-June of 2015 and the January-June of 2018 (Table 4), the number of omissions reduced by 50%, and the incidence rate of omission decreased by 53,8 %, P<0,05, over the same time period. Additionally, development was seen in the following areas: inappropriate handling of a doctor's order, venous exosmosis, pharmaceutical preparation mistakes, patient selection errors, dosage timing errors, noncompliance with skin test regulations, and cross-allergy contraindications. However, throughout the January-June of 2018, patient error rates showed a trend toward improvement. In terms of the method of administration, oral management accounted for 49,4 % of all MEs from 2015 to 2018. The most common mistake category was IV administration problems. However, they drastically declined from 64 in the January-June of 2016 to 27 in the same period in 2018 (figure 3). Additionally, improvements were shown when the medication was administered orally, nasogastrically, externally, and intramuscularly.
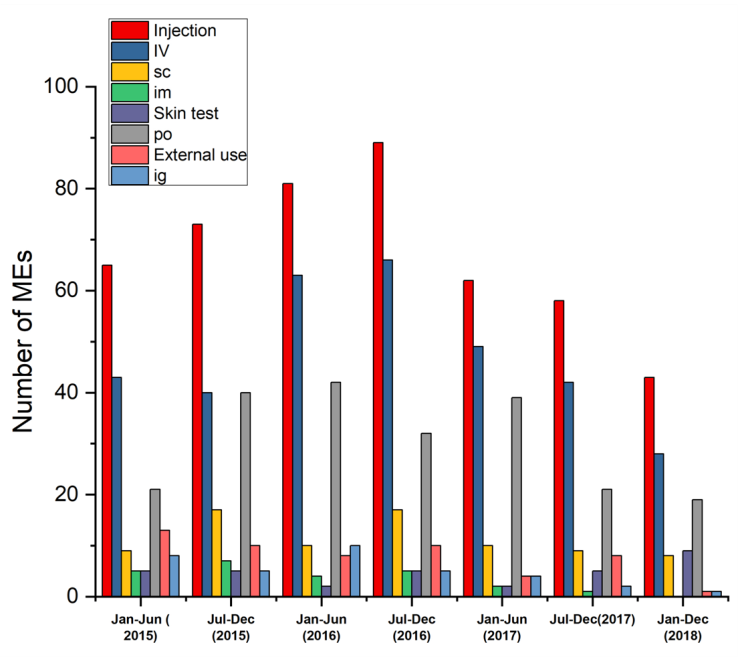
Figure 3. During the time period of January 2015 to June 2018, the administration route and MEs
|
Table 4. ME subtypes during the intervention |
|||||||||||||
|
Period |
Subtype of MEs |
|
|||||||||||
|
|
Omission |
Skin testing and cross-allergy precautions not followed |
Preparation error |
Dose error |
Speed error |
Route error |
Time error |
Duplicate dosing |
Inadequate doctor order management prior to inpatient pharmacy delivery |
Exosmosis |
Wrong patient error |
||
|
Jan-Jun ( 2015) |
42 (0,12 %) |
12 (0,029 %) |
17 (0,042 %) |
10 (0,023 %) |
4 (0,004 %) |
2 (0,004 %) |
11 (0,029 %) |
6 (0,009 %) |
6 (0,012 %) |
5 (0,007 %) |
16 (0,040 %) |
||
|
Jul-Dec (2015) |
32 (0,077 %) |
16 (0,035 %) |
19 (0,039 %) |
14 (0,028 %) |
6 (0,008 %) |
9 (0,018 %) |
13 (0,031 %) |
7 (0,011 %) |
6 (0,008 %) |
5 (0,006 %) |
24 (0,058 %) |
||
|
Jan-Jun (2016) |
45 (0,11 %) |
10 (0,020 %) |
22 (0,045 %) |
15 (0,029 %) |
6 (0,008 %) |
3 (0,003 %) |
15 (0,034 %) |
9 (0,015 %) |
9 (0,013 %) |
0 (0 %) |
31 (0,072 %) |
||
|
Jul-Dec (2016) |
46 (0,098 %) |
13 (0,025 %) |
22 (0,042 %) |
14 (0,025 %) |
6 (0,008 % |
10 (0,019 %) |
16 (0,032 %) |
5 (0,005 %) |
0 (0 %) |
0 (0 %) |
23 (0,047 %) |
||
|
Jan-Jun (2017) |
47 (0,12 %) |
6 (0,011 %) |
13 (0,029 %) |
9 (0,022 %) |
7 (0,011 %) |
6 (0,008 %) |
14 (0,030 %) |
3 (0,003 %) |
0 (0 %) |
0 (0 %) |
17 (0,039 %) |
||
|
Jul-Dec(2017) |
33* (0,067 %) |
6 (0,010 %) |
17 (0,030 %) |
16 (0,029 %) |
4 (0,003 %) |
8 (0,012 %) |
9 (0,016 %) |
0 (0 %) |
2 (0,003 %) |
0 (0 %) |
14 (0,029 %) |
||
|
Jan-Dec (2018) |
23* (0,042 % |
8 (0,013 %) |
7 (0,010 %) |
7 (0,009 %) |
0 (0 %) |
4 (0,005 %) |
4 (0,005 %) |
6 (0,011 %) |
0 (0 %) |
0 (0 %) |
21 (0,042 %) |
||
|
Sum |
268 |
71 |
117 |
85 |
33 |
42 |
82 |
36 |
23 |
10 |
146 |
||
Between 2015 and 2018, no kind four mistakes occurred. In all MEs between 2015 and 2018, type 2 mistakes made up the majority of cases, followed by type 1 errors and type 3 errors. From the January-June of 2015 to the January-June of 2016, there was an upward trend in the number of type 2 mistakes. The frequencies of type 2 mistakes over this time, however, did not alter statistically significantly (P < 0,05). From 133 in the January-June of 2016 to 53 in the January-June of 2018, type 2 mistakes fell steadily (figure 4), with a statistically significant reduction in the incidence rate, P<0,05.
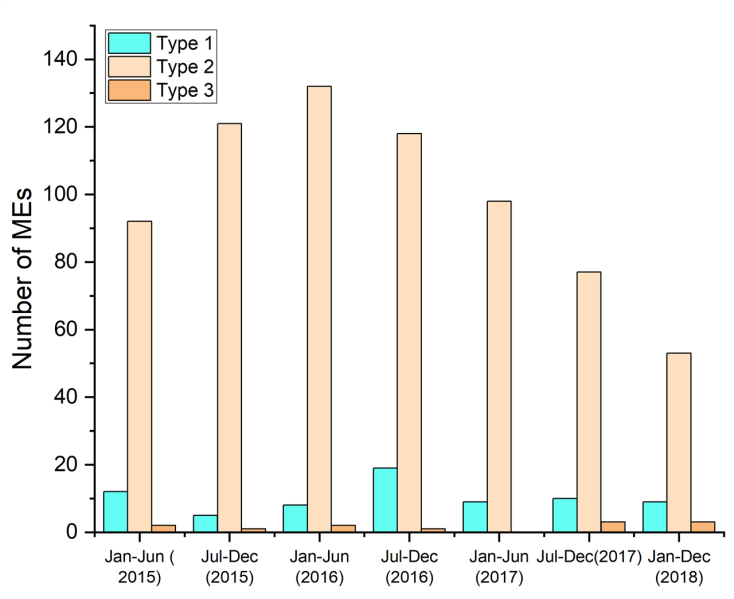
Figure 4. Number of MEs based on the degree of mistake severity
The number of MEs produced by nursing staff in relation to high-alert drugs reduced from 24 (July-December of 2015) to 12 (January-June of 2018), and the incidence of ME incidence reduced (P<0,05) (figure 5).
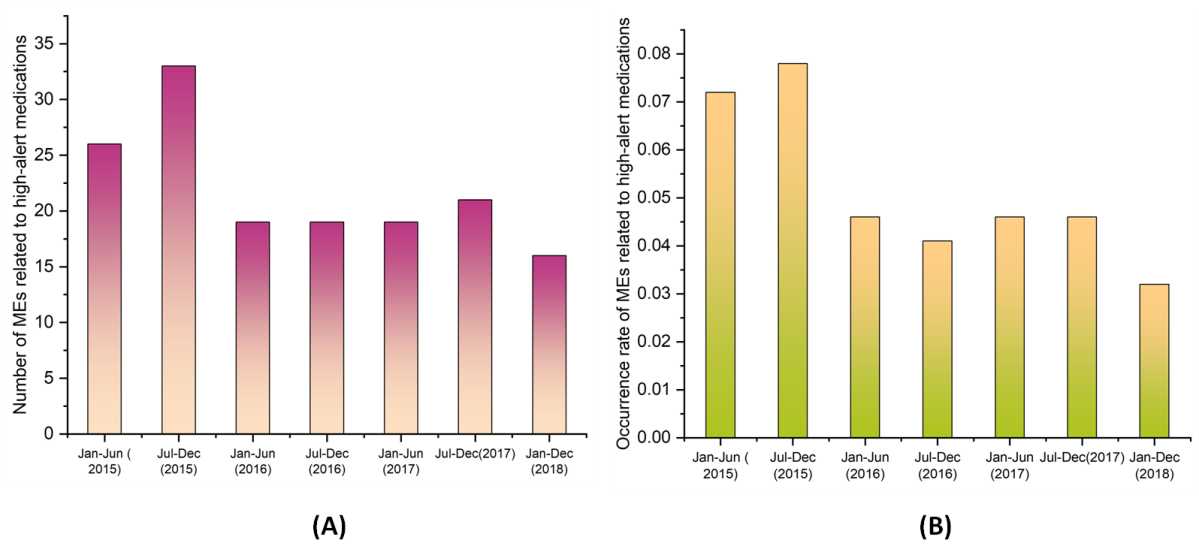
Figure 5. MEs connected with high-alert drugs between January 2015 and June 2018
Insulin, oral hypoglycemic treatments, high-concentration electrolytes, nutrition, complete parenteral, anticoagulants, contrast agents, psychotropic, chemotherapy agents pharmaceuticals, aminophylline, adrenergic agonists, and IV antiarrhythmics were among the high-alert medications under question. Four different high-alert drugs kinds showed overall benefits (figure 6).
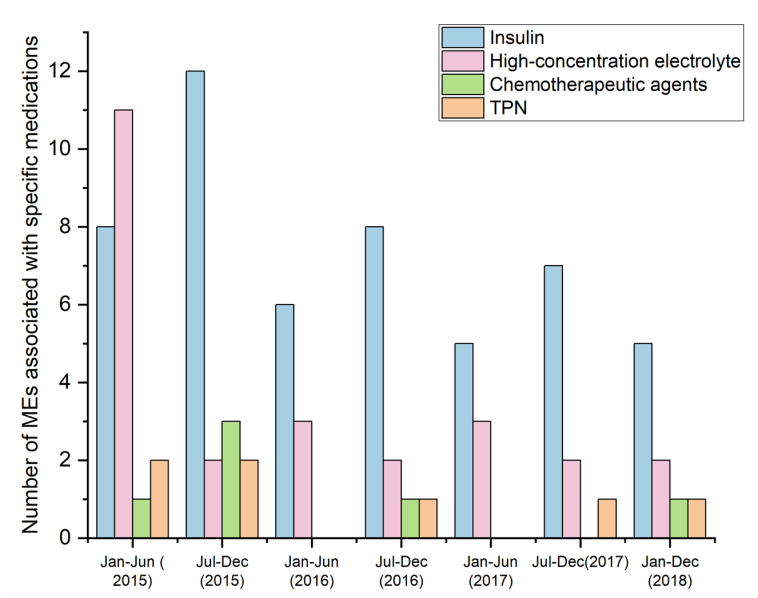
Figure 6. From January 2015 to June 2018, there were four kinds of high-alert drugs that were linked to MEs
The % of MEs discovered within five minutes, thirty minutes, one hour, two hours, and twelve hours increased somewhat from the July-December of 2016. Only around 6,2 %-12,8 % of MEs could be found in the first five minutes, 14,8 %-26,2 % in the first thirty, 22,4 %-29,9 % in the first hour, and 3,9 %-14,6 % on the first day after administration.
47 % to 69 % of all MEs occurred between 8 anti-meridians and six post-meridian. The January-June of 2016 compared to the January-June of 2018, respectively, showed a substantial continuous decline in the occurrence of MEs among seven anti-meridian and five post-meridian, but not between 5 post-meridian and seven anti-meridians. During the January-June of 2018, there were 50 % fewer MEs between 5 post-meridian and seven anti-meridian, and the incidence rate of MEs decreased in tandem (P<0,05).
The majority of the nursing personnel dispensing drugs (about 80 %) were registered nurses. Between 2015 and 2018, nurses made the bulk of MEs, followed by nurses and senior nurses-in-chief. There has been a noticeable steady decline in the number of MEs among registered nurses. Between 2015 and 2018, N1 nurses made up the majority of MEs, followed by N2, N0, N3, and N4 nurses. In January-June 2015, N2 nurses made up 55 % of MEs, and from that point on, MEs have been steadily declining. The majority of N1 nurses who made MEs during the July-December of 2015 and the January-June of 2017 belonged to this cohort. Between the January-June of 2016 and the January-June of 2018, the proportion of MEs made by N0 nurses climbed from 4 % to 32 %. Between 2015 and 2018, the no of MEs made by N4 nurses did not exceed one, whereas the no of MEs made by N3 nurses declined steadily from 14 to 3 (Figure 7). The sequence of relative % of MEs seemed reasonable in the July-December of 2017 and January-June of 2018, which indicates that extra-practiced registered nurses made fewer medication errors.
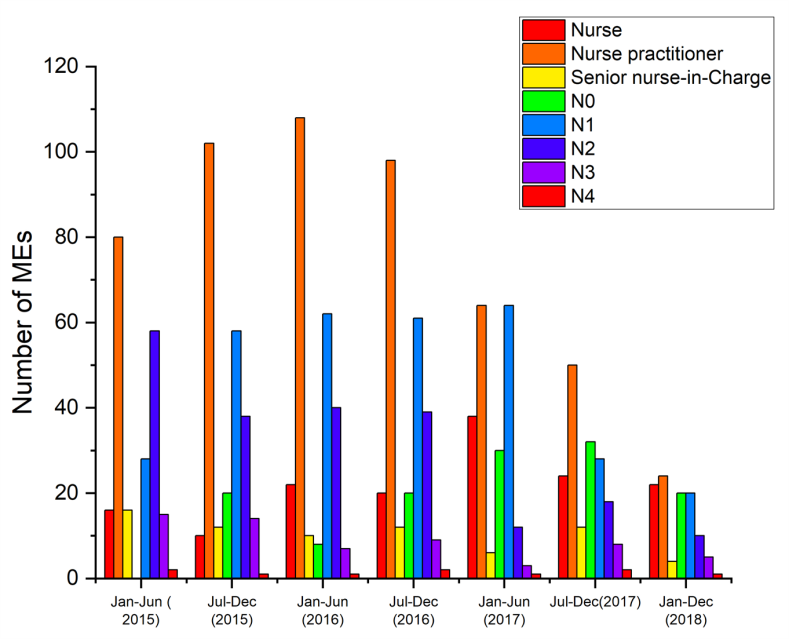
Figure 7. MEs and nurse certification between January 2015 and June 2018
During 2015 and 2018, 6,2 % of all MEs occurred in critical care unit rooms. The difference between the rates of MEs in rooms with and without Intensive Care Units was significantly different (P < 0,001). P < 0,05 showed that intense care unit rooms had a greater prevalence of various ME subgroups than non-intensive care unit rooms (Figure 8). There was no variation in the occurrence of MEs among the two room types, as evidenced by the ratio of MEs in surgical rooms to medicinal rooms of 1,89, which was the same as the ratio of patients released in surgical rooms to medicinal rooms (P<0,05). Surgical rooms, however, demonstrated a more severe reduction in the absolute number of MEs from the January-June of 2016 to the January-June of 2018 than did medical rooms.
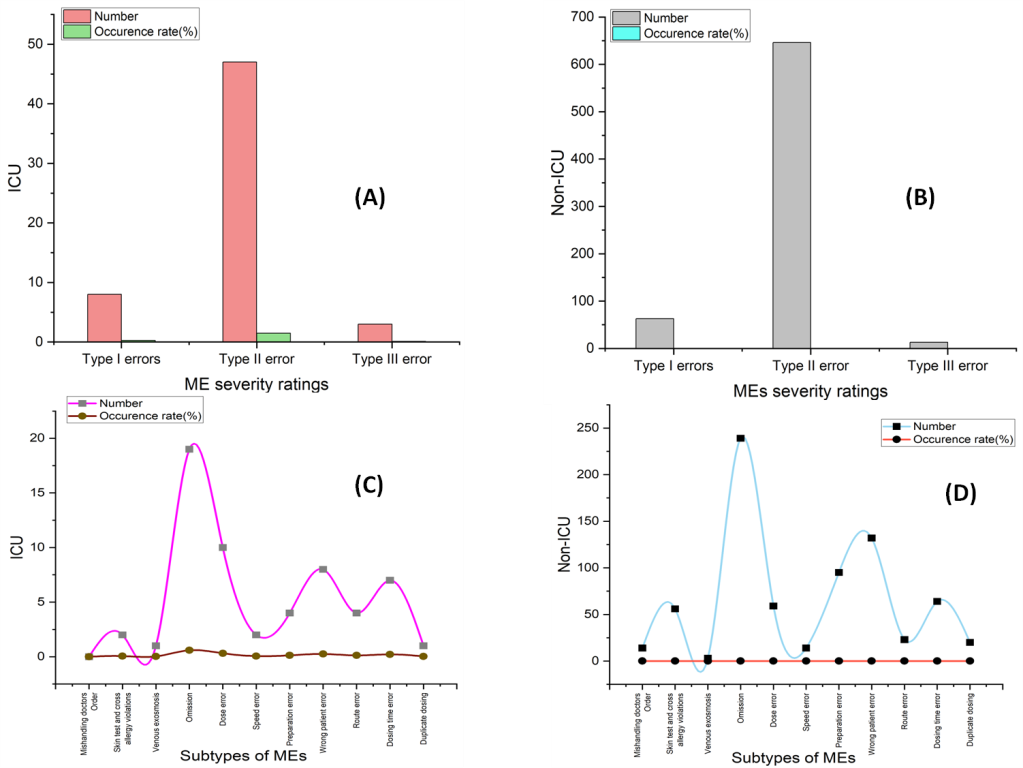
Figure 8. ME subtypes in ICU and non-ICU wards in 2015–2018
CONCLUSION
In this paper, we have outlined BIMC's experience in lowering MEs both prior to and after receiving JCI certification. It was determined that a 3-and-a-half-year ME treatment program was successful. MEs created by nursing personnel might be decreased but not entirely eliminated. Safety in medicine delivery depends critically on the breadth, depth, and effectiveness of multidisciplinary collaboration among nurses, hospital administrators, doctors, information engineers, and chemists. JCI certification could increase health systems' knowledge of, capacity for, and success in preventing MEs and achieving quality enhancements.
The following are some of our study's shortcomings. First off, we didn't statistically look into how many dosages were given and how many MEs there were. Second, given that the number of discharged patients significantly rose from the first half of 2015 to the first half of 2018, modifications to the patient case mix may have prevented the ME decline. Although we provided a good example of implementing a patient-safety policy in a complex hospital to address medication errors, we only analyzed trends during the journey to JCI accreditation and post-accreditation (2015-2019). We couldn't clearly define the pre-intervention and post-intervention phases or conduct a strict comparison between them. However, further research is required to overcome this problem.
REFERENCES
1. Slawomirski L, Auraaen A, Klazinga NS. The economics of patient safety: strengthening a value-based approach to reducing patient harm at the national level. OECD Health Working Papers. 2017;91:1-35. Available from: https://doi.org/10.1787/18152015
2. Gourevitch MN, Thorpe LE. Advancing population health at academic medical centers: a case study and framework for an emerging field. Acad Med. 2019;94(6):813-820. Available from: https://doi.org/10.1097/ACM.0000000000002561
3. Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Dig Med. 2020;3:17. Available from: https://doi.org/10.1038/s41746-020-0221-y
4. Potter PA, Perry AG, Stockert PA, Hall A. Fundamentals of nursing-e-book. Elsevier Health Sciences; 2021.
5. Maas AI, Menon DK, Adelson PD, Andelic N, Bell MJ, Belli A, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16(12):987-1048.
6. Trakulsunti Y, Antony J. Can Lean Six Sigma be used to reduce medication errors in the healthcare sector? Leadersh Health Serv. 2018. Available from: https://doi.org/10.1108/LHS-09-2017-0055
7. Khalil H, Bell B, Chambers H, Sheikh A, Avery AJ. Professional, structural, and organizational interventions in primary care for reducing medication errors. Cochrane Database Syst Rev. 2017;(10). Available from: https://doi.org/10.1002/14651858.CD003942.pub3
8. Farzi S, Irajpour A, Saghaei M, Ravaghi H. Causes of medication errors in intensive care units from the perspective of healthcare professionals. J Res Pharm Pract. 2017;6(3):158-164. Available from: https://doi.org/10.4103/jrpp.JRPP_17_47
9. Hammoudi BM, Ismail S, Abu Yahya O. Factors associated with medication administration errors and why nurses fail to report them. Scand J Caring Sci. 2018;32(3):1038-1046. Available from: https://doi.org/10.1111/scs.12546
10. Naseralallah LM, Hussain TA, Jaam M, Pawluk SA. Impact of pharmacist interventions on medication errors in hospitalized pediatric patients: a systematic review and meta-analysis. Int J Clin Pharm. 2020;42(4):979-994. Available from: https://doi.org/10.1007/s11096-020-01034-z
11. Debono D, Taylor N, Lipworth W, Greenfield D, Travaglia J, Black D, et al. Applying the theoretical domains framework to identify barriers and targeted interventions to enhance nurses’ use of electronic medication management systems in two Australian hospitals. Implement Sci. 2017;12(1):1-13. Available from: https://doi.org/10.1186/s13012-017-0572-1
12. Robertson JJ, Long B. Suffering in silence: medical error and its impact on health care providers. J Emerg Med. 2018;54(4):402-409. Available from: https://doi.org/10.1016/j.jemermed.2017.12.001
13. Assiri GA, Shebl NA, Mahmoud MA, Aloudah N, Grant E, Aljadhey H, et al. What are the epidemiology of medication errors, error-related adverse events, and risk factors for errors in adults managed in community care contexts? A systematic review of the international literature. BMJ Open. 2018;8(5):e019101. Available from: http://dx.doi.org/10.1136/bmjopen-2017-019101
14. Wei H, Sewell KA, Woody G, Rose MA. The state of the science of nurse work environments in the United States: A systematic review. Int J Nurs Sci. 2018;5(3):287-300. Available from: https://doi.org/10.1016/j.ijnss.2018.04.010
15. Walsh EK, Hansen CR, Sahm LJ, Kearney PM, Doherty E, Bradley CP. The economic impact of medication error: a systematic review. Pharmacoepidemiol Drug Saf. 2017;26(5):481-497. Available from: https://doi.org/10.1002/pds.4188
FUNDING
No financing.
CONFLICTS OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Conceptualization: Malathi Hanumanthayya, Basavaraj Mudhol, Varsha Agarwal.
Methodology: Malathi Hanumanthayya, Basavaraj Mudhol, Varsha Agarwal.
Drafting - original draft: Malathi Hanumanthayya, Basavaraj Mudhol, Varsha Agarwal.
Writing - proofreading and editing: Malathi Hanumanthayya, Basavaraj Mudhol, Varsha Agarwal.