REVIEW
A novel role for enhancing nurse-technology interfaces and medical device advancements for patient care
Novedoso rol para mejorar las interfaces enfermera-tecnología y los avances en dispositivos médicos para la atención al paciente
Basavaraj
Mudhol1 ![]() *,
Meena Krishna2
*,
Meena Krishna2 ![]() *, Asha Kademane3
*, Asha Kademane3 ![]() *
*
1Teerthanker Mahaveer University, College of Nursing. Moradabad, Uttar Pradesh, India.
2ATLAS SkillTech University, ISDI - School of Design & Innovation. Mumbai, India.
3JAIN (Deemed-to-be University), Department of Life Sciences. Karnataka, India.
Cite as: Mudhol B, Krishna M, Kademane A. A novel role for enhancing nurse-technology interfaces and medical device advancements for patient care. Salud, Ciencia y Tecnología. 2023;3(S1):463. https://doi.org/10.56294/saludcyt2023463
Submitted: 23-05-2023 Revised: 29-05-2023 Accepted: 06-08-2023 Published: 07-08-2023
Editor: Dr.
William Castillo-González ![]()
Associate Editor: Fasi
Ahamad Shaik ![]()
ABSTRACT
To instruct a new generation of professional, this paper will highlight two innovative nursing and health technology collaborations and produce cutting-edge research and breakthroughs. A highly competent response, including teams of experts from several disciplines, is required for complex health concerns. Opportunities for improved technology-nurse interaction and consequent innovation arise if the clinical perspective of nursing is included while viewing medical engineering through a wider lens. The finest training-seeking experienced nurse specialists who can be cutting-edge and bring unique suggestions to enhance patient care and results are found in double nursing engineering degree programs. The background in innovations and engineering in nursing is included in this examination, along with the justification for creating two state-of-the-art joint majors and information about those courses. This innovative program will advance healthcare-related technology and enhance the nursing profession’s capacity for innovation in both design and execution. Additionally, by providing interdisciplinary training and encounters with college students pursuing medical specialists or bachelor’s degrees in nursing, they can improve their knowledge and abilities. Even though nurses are not participating in designing and creating patient care devices, significant patient care improvement possibilities are lost. Creative nurse and engineer cooperation is required to capitalize on nurse creativity and develop patient care improvements.
Keywords: Medical Device Advancements; Nurse-Technology Interfaces; Patient Care; Healthcare Systems.
RESUMEN
Con el fin de instruir a una nueva generación de profesionales, este artículo destacará dos colaboraciones innovadoras entre enfermería y tecnología sanitaria, que dan lugar a investigaciones y avances punteros. Para hacer frente a problemas sanitarios complejos se requiere una respuesta altamente competente, que incluya equipos de expertos de varias disciplinas. Las oportunidades de mejorar la interacción entre tecnología y enfermería y la consiguiente innovación surgen si se incluye la perspectiva clínica de la enfermería al tiempo que se contempla la ingeniería médica a través de una lente más amplia. En los programas de doble titulación de ingeniería en enfermería se encuentran los mejores especialistas en enfermería que pueden estar a la vanguardia y aportar sugerencias únicas para mejorar los cuidados y los resultados de los pacientes. En este examen se incluyen los antecedentes de las innovaciones y la ingeniería en enfermería, junto con la justificación para crear dos especializaciones conjuntas de vanguardia e información sobre dichos cursos. Este innovador programa hará avanzar la tecnología relacionada con la asistencia sanitaria y mejorará la capacidad de innovación de la profesión enfermera tanto en el diseño como en la ejecución. Además, al proporcionar formación interdisciplinar y encuentros con estudiantes universitarios que cursan especialidades médicas o licenciaturas en enfermería, pueden mejorar sus conocimientos y habilidades. Aunque las enfermeras no participen en el diseño y la creación de dispositivos de atención al paciente, se pierden importantes posibilidades de mejora de la atención al paciente. Es necesaria una cooperación creativa entre enfermeras e ingenieros para aprovechar la creatividad de las enfermeras y desarrollar mejoras en la atención al paciente.
Palabras clave: Avances en Dispositivos Médicos; Interfaces Enfermera-Tecnología; Atención al Paciente; Sistemas Sanitarios.
INTRODUCTION
Digital technology can potentially address many issues and problems facing the care sector. Several medical facilities are struggling with issues, including a shortage of qualified employees and an increasing demand for long-term care due to demographic changes. A blossoming study topic on technological advances and care has been inspired by the hope that information technology may help people who need care maintain their autonomy, improve their standards of life, and boost their health.(1) This field also supports both professional and informal carers. Early studies concentrate on the advantages that digital platforms provide for things like patient security and process enhancements, which may help make the most use of the currently available assets. The interaction between nurses and different medical equipment, Electronic Health Records (EHRs), and other digital systems becomes more important as healthcare technology develops.(2) The latest advances in digital health are shown in figure 1.
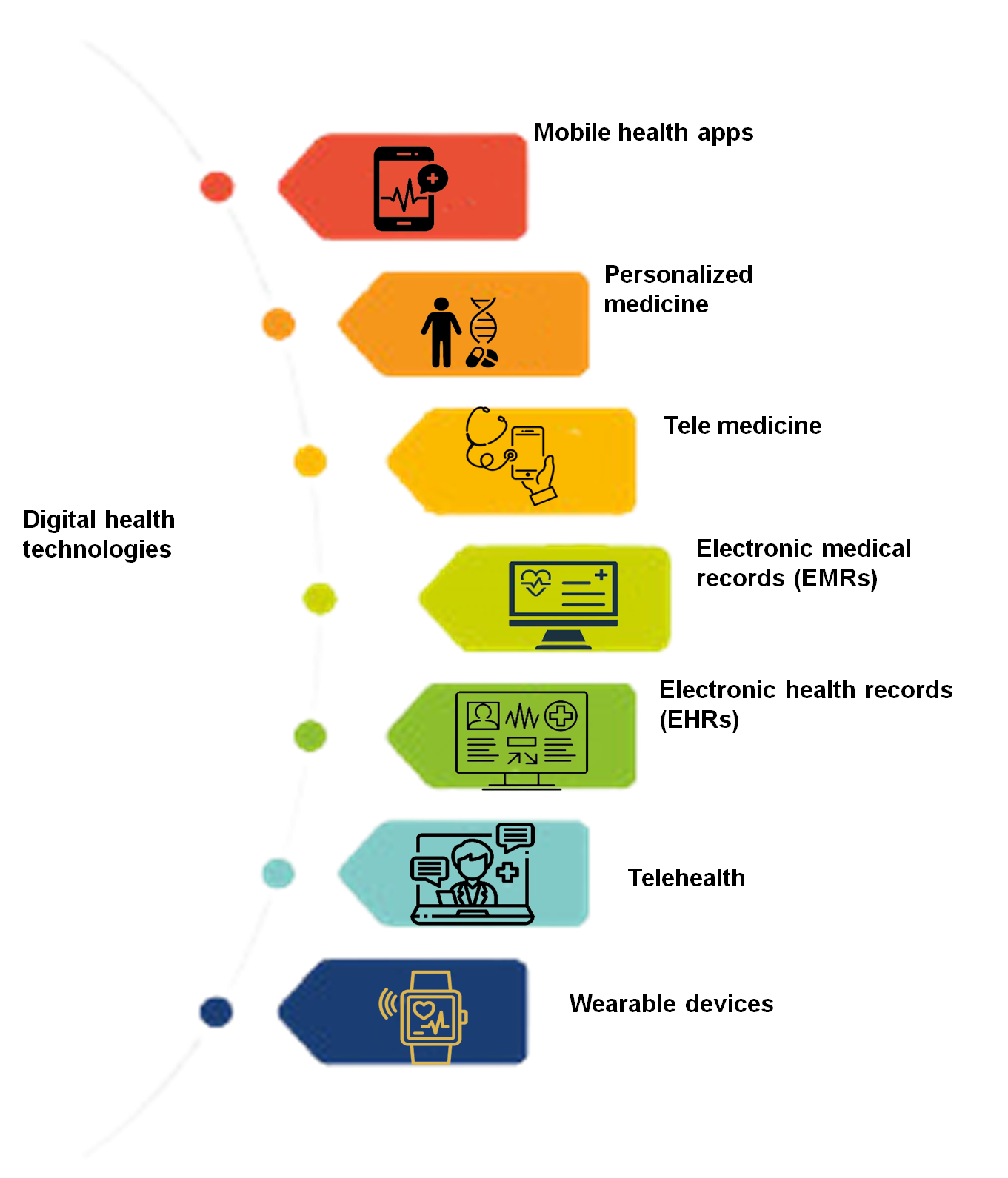
Figure 1. Digital health technologies
These interfaces' usability and user-centered design are crucial to ensure that nurses can efficiently browse, comprehend, and utilize the enormous quantity of patient data provided by technology. Facilitating smooth interactions, lowering cognitive burden, and enabling nurses to respond quickly to information are all benefits of improving nurse-technology interfaces. Considering the hazards of electrical shocks posed by medical equipment and our concern for the security of patients, especially biomedical engineering originated in the 1960s. Biomedical engineers are now responsible for improving medical technology for diagnostic and therapeutic reasons.(3) Making these advances clinically significant requires engineering and nursing knowledge. It is effective because these professionals are designing solutions to problems across the spectrum of healthcare, including direct-care surgical robots, recovery devices, and workflow enhancers. The ability of a nurse to use technologies and create technical solutions for the provision of nurse care and medical treatment requirements, such as automation, patient care machinery, or computerized simulations, would be significantly improved by training in biomedical engineering.(4) However, a medical scientist’s ability to handle medical issues would be significantly improved by a background in medicine combined with the necessary clinical expertise. It is very simple to go back over a century and pinpoint the advancements in medical electronics and technologies that have had a significant overall influence on people and society at large. Applying the same principles to current events is more challenging. Current efforts and successes can be fairly evaluated, but their total influence is trickier. It is very difficult to predict future advancements and their effects.(5)
Users of medical devices are engaged in creating and evaluating medical device technology because of their potentially crucial role in the invention, development, assessment, implementation, and distribution of the technology. Under current medical device rules, interaction with users is also necessary. Users' participation in creating and assessing a specific technology may be encouraged or dissuaded by the advantages and costs associated with such engagement.(6) Healthcare delivery has substantially transformed due to the quick development of medical gadgets. These cutting-edge technologies, which range from wearable sensors and smart infusion pumps to remote monitoring systems and Artificial Intelligence (AI)-enabled diagnostics, can potentially change patient care. Real-time patient monitoring, early warning signs of worsening illnesses, and individualized treatment regimens are all provided by these gadgets. Figure 2 depicts the application cases for AI in the pharmaceutical and healthcare sectors as of 2022.

Figure 2. Pharmaceutical and medical AI applications in 2020
To guarantee these devices' smooth incorporation into clinical processes and enhance their efficacy, nurse engagement in their development and deployment is essential (7). Advanced medical technologies and nurses working together increase patient safety measures. Nurses may obtain real-time patient data, continually monitor vital signs, and quickly spot possible concerns by using technology. Smart alarms, pharmaceutical delivery technology, and nurse call systems may all be integrated to assist in improving patient safety, decreasing mistakes, and stopping unfavorable outcomes. Nurses should also get thorough training to ensure proficiency in managing and correctly interpreting data from these devices. Healthcare organizations must emphasize continual training and cooperation to equip nurses to embrace and use these technological advancements, improving patient outcomes and transforming the healthcare environment.(8)
Chang et al.(9) proposed a preliminary investigation using social learning theory embedded in Spherical Video-Based Virtual Reality (SVVR) for childbirth instruction provided; furthermore, the learning outcomes of nursing students who took part in SVVR classroom instruction and those who learned using the conventional method were contrasted. Campbell et al.(10) outlined the procedure used in creating the updated 2018 Competencies. A comprehensive analysis and consensus-building process were carried out using a biphasic Delphi method. Together, four people from the fields of community/public health practice and education developed and put into action a methodical revision process for the QCC Competencies. One of the methods nurses use to aid patients in their recovery, particularly those with nursing issues related to mental diseases, is the therapeutic communication strategy. Siregar et al.(11) was carried out in response to concerns over the findings of observations, early research, and reports concerning the frequency of therapy failures for Schizophrenic patients brought on by communication problems during treatment. With the introduction of an IoT branch known as the Internet-of-Medical Things (IoMT) systems, healthcare systems are one of these applications that have been transformed by IoT.
Ghubaish et al.(12) proposed cutting-edge methods for protecting data in IoMT systems throughout collection, transmission, and storage. They provide an in-depth examination of all conceivable assaults on IoMT systems, including physical and network threats. Food and Drug Administration(13) proposed a structure for modifying AI/ML-based Software as a Medical Device (SaMD) that is based on the organization-based TPLC approach as envisioned in the Digital Health Software Precertification (Pre-Cert) Initiative, the benefit-risk framework of the FDA, and the globally harmonized International Medical Device Regulators Forum (IMDRF) risk classification standards. The US Food and Drug Administration (FDA) uses Medical Device Safety Communications (MDSCs) to alert patients and medical professionals about critical new safety information. Tau et al.(14) evaluated the first safety signal sources that lead to MDSC publishing and any possible relationships between the kind of safety concern, the MDSC data source, and subsequent FDA action. Srivastava et al.(15) investigated the use of Blockchain technology in the security of the Internet of Things (IoT) based on Remote Patient surveillance systems.
The study discussed the advantages of blockchain-based security methods in monitoring patients remotely using IoT devices and some practical challenges. Bayoumy et al.(16)addressed the fundamental engineering concepts of typical sensors worn by individuals and the situations in which they may be prone to inaccuracy. They also look at how these devices may be used to remotely screen for and diagnose disorders that affect the heart, such as arrhythmias, as well as treat patients who already have cardiac problems like heart failure. The gathering, assessment of quality, interpretation, and harmonization of data resulting from the vast number of heterogeneous IoT medical devices in use are some obstacles that IoT healthcare must overcome in an age of constant expansion. Gonzalez-Argote(17) and Mavrogiorgou et al.(18) developed a method for successfully resolving the junction of these difficulties. The approach allows for the initial collection and subsequent cleaning of the information from various devices. In this paper, we examine a new role in improving nurse-technology interfaces and technological advances in medical devices for patient care.
METHODS
Innovations in Technology
The expansion of walk-in clinics run by nurse practitioners and the shift toward more community-based treatment are all examples of the unprecedently rapid transformation that is taking place in the healthcare industry. However, as we've seen, the biggest influence on nursing, how nurses care for patients, and patient outcomes will come from using new technology. The rate of change is anticipated to quicken as new service models are created, and demand to contain healthcare costs continues to climb. A variety of "futurist" forecasts of how the future of health care would pan out have been made as a consequence of the need to coordinate projected technical advancements, capital expenditure, patient outcomes, and cost reductions. One such prediction is "Healthcare and Life Sciences Predictions 2020". Wearable monitoring technology, tailored genetic therapies, the use of machine learning in diagnostic and therapeutic procedures, and robotic medical and social applications are just a few of the predictions now accessible to physicians. In addition, electronic health records are still being developed, and dispersed information networks are being built between locations and providers. These innovations open up new fields of study and therapeutic applications.
Nursing
Additionally, nursing care is becoming harder to provide. It was stated that this isn't merely a result of patient complexity and acuity rising but also owing to the introduction of new technology that may affect how nursing care is organized, prioritized, and decided. As previously said, managing the human-technology interface and integrating new technologies into practice provide nurses with some of their biggest problems. Additionally, there are several ethical and data security concerns. As evidenced by Carol Huston's American Nurses Association webinar, "Touch Vs. Tech: Leading Care in a Technology-Driven Environment Without Losing the Human Touch," there have been long-standing and ongoing worries regarding using electronic devices in health care and its possible impacts on nursing care and patients. The work environment for nurses is evolving quickly and offers chances to use technology to enhance patient outcomes. To provide nursing care in the future, nurses will need to develop into more than simply proficient technology users. The greater involvement of nurses in the creation and development of novel medical devices and issues of practice and policy is required, given the changing clinical nursing environment. Partnerships between nurses and less traditional professionals, such as engineers, are increasing at a time when transdisciplinary education and practice are expected.
Even though research on the telerobotic cognitive nursing companion is still in its early stages, nurses and engineers are working to enhance the interface between people and robots so that robots may offer care utilizing fine motor skills and resemble people to help patients feel more at ease. Second, engineers from the Massachusetts Institute of Technology worked with Labor and Delivery (L&D) to assign challenging nursing personnel to nurse executives, gynecology and obstetrics specialists, and a busy labor and delivery unit will collaborate. To evaluate their decision-making with changes in the allotment of staff resources and the L&D population of patients, nurse managers took part in computer simulations. In real-world settings and computer simulations, an increasing unit census is linked to delays in patient treatment. Computer simulation is a practical and reliable way to show how treatment choices are affected by changes in patient volume. Medical professionals, engineers, and nursing anticipate adopting simulation to enhance clinical resource management.
The Nurse-Engineer is a New Profession
This has been proposed for about 25 years to formalize building bridges between medical and technical professions via education. Engineers and nurses both employ science and technology to address issues in the real world, but nurses emphasize the "art of caring" and "practice of health promotion." In comparison, engineers emphasize the "art of design" and "practice of building." The concept that a new profession, the nurse engineer, was required to design, create, and it was encouraged to train medical professionals and patients on how to utilize information systems. The notion of combining the two independent disciplines of nursing and biomedical engineering was discussed further by some who argued advocates for the formation of nursing technology, a new regulation akin to medical scientists. We argued that rather than combining nursing with a technical degree, there is presently no unified academic and professional curriculum that treats nursing and engineering as one discipline. A few universities have developed innovative combined degrees or partnerships to enhance patient experiences or increase the effectiveness of the healthcare system. Still, no institutions have established a new specialty, such as nurse engineering.
Every new system or product must have nursing input at the conceptual, research, and development phases. Nurses are too often simply involved in the testing or evaluating of a finished product, which may preclude important functioning adjustments. Delivering healthcare in settings with various administrative structures, nursing practice models, and practice locations, such as the hospital, communities, and homes, is more difficult. To examine patient and nursing requirements, it is necessary to develop a systematic technique. The promise of new technologies and practice advancements will need to be communicated to healthcare executives, managers, patients, caregivers, lawmakers, and the general public in innovative ways.
Possible Impacts of Technology Education on Nurses
Candidates from institutions that educate the underlying sciences, clinical nursing procedures, and the uses of medical engineering are practiced to work at the nexus of knowledge and be concerned for patients. Creators of medical equipment firms often develop a collection of proprietary information that forms the basis for an enterprise and early finance to contribute the first technical breakthrough. After a successful financing campaign, founders will unavoidably hire additional personnel to conduct clinical testing and continue technical development. With smaller projects, a nurse engineer may serve as both a clinical assessor and a technological developer, cutting expenses and speeding up the procedure for creating a product. This benefit could manifest in later stages of business when nursing engineers stay close ties between engineering development and clinical testing and, more crucially, clinical usefulness.
These issues are eliminated while teaching nurse engineers in a shared curriculum, which also offers the chance for educational synergy. The senior engineering capstone provides a chance to integrate the ideas from all previous classes, even if the relationship between the design of engineering and nursing care may be conceptual. Two colleges have taken steps to create integrated nursing and engineering programs to better address the multifaceted demands of patients and the healthcare system as a whole. Here are descriptions of both strategies. Details on the strategic choices and investments undertaken to achieve this aim are given. The planning phase of the curriculum at the University of Massachusetts-Amherst is presently underway. This study provides an overview of the dual degree program that Duquesne University has already started, including its curriculum, programmatic components, and objectives for measuring academic progress.
The Amherst Model from the College of Massachusetts
A dual degree in nurse engineering is being planned by the schools of nursing and engineering at the University of Massachusetts-Amherst. After each institution secured a $25 000 yearly stipend from alumni to fund studies in technology and medical health care, the groundwork for the combined degree planning was built in 2008. The fellowship aimed to encourage students to engage in cross-disciplinary research and use engineering-based methods to solve practical issues encountered in clinical settings. There was the overall conviction that to find long-term, patient-centered solutions to contemporary healthcare issues, a multidisciplinary approach was necessary. A collaborative nursing and engineering examination of qualifications led to the awarding of the 1-year scholarships to Ph.D. candidates at the start of their studies. Twelve fellowships have been given out, six leading to doctoral degrees.
The research conducted since the community scheme's inception may be generally categorized as analyses of patient safety problems, information services, and service optimization. The creation and use of a computerized system for monitoring failures in group geriatric facilities, as well as a review of how well-designed health information websites are for patients with cardiac and diabetic disorders, were among the projects in one group that looked at novel approaches to communicating health-related information and services using technology for communication. Another research looked at how Hispanic patients managed their HbA1c levels by using portable diabetes monitoring devices. To see whether changes in nurses' eye-scanning patterns may help detect medical mistakes in replicated clinical settings before they endanger patient safety, researchers used tracking technologies to observe their eye-scanning patterns. The idea behind this research was that medical personnel might be taught the best visualization techniques for administering medications safely at home or in a hospital.
The Department of Nursing recruited two tenure-track lecturers with postgraduate expertise in managing symptoms will join the department the following academic year, one of whom knew the use of wearable technology. The engineering college hired specialists to design and construct wearable health gadgets at the same time as these nurse hires took place. This has the effect of bringing multidisciplinary research ideas in healthcare together and expanding them. Additionally, it marked the start of several academics centering their study on the objectives of the College of Nursing, either by taking part in National Institutes of Health summer academies or competing for funds to collaborate with established researchers in their area.
Model of Duquesne
In the autumn of 2015, a brand-new, the 5-year Biomedical Engineering and Nursing Bachelor of Science (BME/BSN) curriculum was launched. It includes an expedited second-degree curriculum lasting one year with a conventional 4-year engineering curriculum. Participants will be more prepared to develop and use technological medical treatments in a realistic setting, workable, and patient-centered way by equipping students with the expertise of both disciplines. A maximum of 20 students are allowed to enroll in each BME cohort in order to promote a superior learning environment and guided research. The Commission of Collegiate Nursing Education and the Pennsylvania State Board of Nursing have both granted authorization has accredited Duquesne University's BME/BSN curriculum. Having at least four years of verifiable professional experience qualifies engineers to sit for the Professional Engineering Exam.
The capstone project, which represents the pinnacle of the biomedical engineering educational process, is an essential part for all students. In the fifth year of study, the work is finished in two five-credit courses. The student team will investigate medically linked medical issues for the final assignment and provide a technological solution based on the knowledge learned in the classroom and clinical settings throughout nursing courses. Most often, a medical procedure or equipment will be the answer. An engineering and economic study of the solution is conducted after finishing mechanistic and statistical examinations of the issues, coming up with a solution, making a prototype, and putting it to the test. Students will submit their ideas to a panel of teachers, engineers, medical specialists, and business executives at the conclusion of their fifth year.
RESULTS
New Approaches to Evaluating Academic Results
This distinct paradigm requires a new evaluation instrument to provide reliable metrics and assessment, even if nursing and engineers have discipline-specific accrediting techniques and organizations. Due to the fundamental differences between the two professions and the course's early low graduation rate, this assessment is made more challenging. Evaluation at Duquesne will unavoidably include determining educational results and gauging early career development. A system for tracking ongoing advancements in academic relevance will also be implemented by the program, and it will take into account student feedback, achievement, satisfaction with work, job placement, remuneration, and career progression.
There will be a separate internal panel monitoring program success to lessen the managerial load brought on by two official accrediting authorities for engineering and nursing. Faculty from engineering, nursing, and the health professions will all be represented in this review group. Every year, this committee will assess student performance. These outcomes will be added to those used for engineering and nursing certification. The results specific to the nurse engineer idea will be established by the review committee's first implementation. Last but not least, we'll create an independent advisory council comprised of scholars and professional experts in engineering, nursing, and business. The purpose of this advisory board is to ensure the continuation of the dual-degree programs relevant to both business and academics by reviewing the curriculum and educational materials, offering insight into recent advancements, and the changing nature of the professional field.
The use of medical devices
There were a total of 1 306 clinical trials included, and out of them, 763 papers (57,2 %) used medical devices for diagnosis or therapy, while only 543 articles (40,6 %) did not. Table 1 lists the 1 342 instances between 2018 and 2022 in which medical devices were employed in clinical research; diagnostic devices were used 931 times (or 70 %), while medical devices were used 411 times (or 30 %).
|
Table 1. Clinical studies that involve medical gadgets |
||
|
|
Top ten medical equipment used |
Quantity of articles |
|
Diagnostic Instrument 931 |
Ultrasound scanners |
80 (8,5) |
|
DITI equipment |
57 (6,1) |
|
|
HRV measurement equipment |
43 (4,6) |
|
|
Body composition analyzer |
41 (4,4) |
|
|
EMG equipment |
28 (3,0) |
|
|
Endoscope |
21 (2,2) |
|
|
Etc. |
19 (2,0) |
|
|
Treatment device 403 |
Electroacupuncture devices |
148 |
|
TENS equipment |
82 (20,3) |
|
|
ICT equipment |
74 (18,4) |
|
|
Ultrasound devices |
66 (16,4) |
|
|
IR equipment |
23 (5,7) |
|
|
M/W equipment |
23 (5,7) |
|
|
EST equipment |
19 (4,7) |
|
|
Laser devices |
12 (3,0) |
|
|
SSP equipment |
11 (2,7) |
|
|
Etc. |
11 (2.7) |
|
|
MRI scanners |
n (%) |
|
|
X-ray machines |
194 (20,6) |
|
|
CT scanners |
172 (18,3) |
|
|
EKG equipment |
139 (14,8) |
|
In the clinical investigations, diagnostic tools were employed 942 times. In table 1, the ten most popular diagnostic tools are listed. Instruments for electrocardiography (EKG) were utilized in 79 trials (7,4 %); CT scans have been employed in 128 studies (14,8 %); 56 studies (5,1 %) employed ultrasound machines; 42 investigations (4,6 %) used Digital Infrared Thermal Imaging (DITI) technology; 41 studies (4,4 %) used heart rate variability (HRV) measuring tools; and 27 studies (5,1 %) used body composition monitors. The development of the MoH device acquisitions prices/Ad hoc device standard selling prices ratio over three years is shown in figure 3.

Figure 3. Comparison charts showing the MoH's chosen medical equipment purchase pricing for each of the three time periods
Therapy with medical gadgets was utilized in 412 instances in the 1 306 clinical trials examined. In table 1 there is a list of the top 10 therapy devices. There were 82 studies (20,3 %) using electroacupuncture devices; 66 studies (16,3 %) using Interferential Current Therapy (ICT); 74 studies (18,4 %) using Transcutaneous Electrical Nerve Stimulation (TENS); 23 studies (5,7 %) using ultrasound and infrared (IR) devices; 19 studies (4,7 %) using microwave therapy (M/W); 12 studies (3 %); and 0,0 % using electrical stimulation treatment (EST) equipment; lasers and silver sputtering.
The annual use of medical devices
From 2018 to 2022, there was a decline in the usage of medical devices, which rose by 2016. In 2012, medical gadgets were used the most (312 times). Overall, the use of diagnostic tools showed a downward tendency. Figure 4 shows that after a reduction in the usage of treatment devices from 2018 to 2021, a sharp surge was seen in 2022.

Figure 4. From 2018 to 2022, the use of medical devices
The top 5 medical diagnostic tools were used to diagnose various illnesses. In 16 studies (8,2 %), 12 studies (6,2 %), and five studies (2,6 %), MRI was utilized to identify lumbar discherniation, stroke, and rotator cuff tears, respectively. Scoliosis was detected by X-ray machines appeared in 9 trials (5,1 %), whereas pneumonia and herniated lumbar discs appeared in 4 research (2,2 %) each. Four trials (2,9 %) utilized CT scanners to detect stomach cancer and lumbar disc herniation; eight researchers (5,7 %) used them to detect stroke; and five studies (3,5 %) used them to detect lung cancer. EKG was used in 4 trials (5,0 %) to diagnose amyotrophic lateral sclerosis and stroke. As indicated in table 2, ultrasound devices were used to diagnose uterine myoma in three studies (5,3 %), infertility in four studies (7,0 %), frozen shoulders in two studies (3,5 %), hepatitis in two studies (3,5 %), gastronomies tears in two studies, and uterine hemorrhage in one study (3,5 %).
|
Table 2. Illnesses that have been identified by diagnostic tools |
||
|
Diagnostic Equipment |
Top 3 utilized diseases |
N (%) |
|
X-ray machines |
Pneumonia and herniation of lumbar disc |
4 (2,3) |
|
Scoliosis |
9 (5,2) |
|
|
Ultrasound scanners |
Hepatitis, frozen sholder, gastrocnemius tear, drug-induced liver injury, and uterine bleeding |
2 (3,5) |
|
Uterine myoma |
3 (5,3) |
|
|
Infertility |
4 (7,0) |
|
|
EKG equipment |
Parkinson disease |
2 (2,5) |
|
Amyotrophic lateral sclerosis and stroke |
4 (5,0) |
|
|
MRI scanners |
Stroke |
12 (6,2) |
|
Rotator cuff tear |
5 (2,6) |
|
|
Herniation of a lumbar disc |
16 (6,2) |
|
|
CT scanners |
Lung cancer |
5 (3,6) |
|
Herniation of lumbar disc and gastric cancer |
4 (2,9) |
|
|
Stroke |
8 (5,8) |
|
The research demonstrates that in clinical investigations, diagnostic gadgets have been employed more often than therapeutic devices. The data on utilization each year reveal that both medical devices have been gradually employed from 2018 to 2022 when examining the diagnostic and therapeutic devices used in clinical investigations. Historically, the practitioners diagnosed their patients using the ancient techniques of seeing, smelling, inquiring, and touching and then treated them with acupuncture, moxibustion, and herbal remedies. Medical technology has advanced so that gadgets are now employed for diagnosis and therapy. At first, not even medical professionals used technology to diagnose and treat patients. This transformation was made possible by objective data based on the use of contemporary medical instruments, and it is anticipated that these kinds of medical actions will continue to alter as scientific technology advances.
CONCLUSIONS
The utilization of medical equipment by physicians was examined. It helped people comprehend the current state and trends in physicians' medical conduct related to medical devices. According to this research, physicians use medical equipment to diagnose and treat patients. It is vital to institutionalize when taking doctor-patient interactions into account. This information may also be used as a resource for deciding on policies and teaching initiatives. The MakerNurse movement, new biomedical and nursing degree partnerships, and other trends have the potential to significantly alter how nurses and technology interact. Collaborations between nurses and engineers can change how we think, develop technology, and address pressing clinical issues due to these innovative initiatives. Through more involvement in and acknowledgment of significant and beneficial patient care equipment advancements, this paradigm shift also gives specially trained nurses a chance to enhance patient care and ensuing results.
REFERENCES
1. Ratta P, Kaur A, Sharma S, Shabaz M, Dhiman G. Application of blockchain and internet of things in healthcare and medical sector: applications, challenges, and future perspectives. J Food Qual. 2021;2021:1-20.
2. Pai MM, Ganiga R, Pai RM, Sinha RK. Standard electronic health record (EHR) framework for Indian healthcare system. Health Serv Outcomes Res Methodol. 2021;21(3):339-362.
3. Wears R, Sutcliffe K. Still not safe: patient safety and the Middle-Managing of American medicine. Oxford University Press; 2019.
4. Wen A, Fu S, Moon S, El Wazir M, Rosenbaum A, Kaggal VC, Liu S, Sohn S, Liu H, Fan J. Desiderata for delivering NLP to accelerate healthcare AI advancement and a Mayo Clinic NLP-as-a-service implementation. NPJ digital medicine. 2019;2(1):130.
5. Tobore I, Li J, Yuhang L, Al-Handarish Y, Kandwal A, Nie Z, Wang L. Deep learning intervention for health care challenges: some biomedical domain considerations. JMIR mHealth uHealth. 2019;7(8):e11966.
6. Shah SGS, Robinson I. Benefits and barriers to involving users in medical device technology development and evaluation. Int J Technol Assess Health Care. 2007;23(1):131-137.
7. Gu H, Huang J, Hung L, Chen XA. Lessons learned from designing an AI-enabled diagnosis tool for pathologists. Proc ACM Hum Comput Interact. 2021;5(CSCW1):1-25.
8. Hammerschmidt J, Manser T. Nurses’ knowledge, behaviour and compliance concerning hand hygiene in nursing homes: a cross-sectional mixed-methods study. BMC Health Serv Res. 2019;19(1):1-13.
9. Chang CY, Sung HY, Guo JL, Chang BY, Kuo FR. Effects of spherical video-based virtual reality on nursing students’ learning performance in childbirth education training. Interactive Learning Environments. 2022;30(3):400-416.
10. Campbell LA, Harmon MJ, Joyce BL, Little SH. Quad Council Coalition community/public health nursing competencies: Building consensus through collaboration. Public Health Nurs. 2020;37(1):96-112.
11. Siregar I, Rahmadiyah F, Siregar AFQ. Therapeutic communication strategies in the nursing process of angry, anxious, and fearful schizophrenic patients. Br J Nurs Stud. 2019;1(1):13-19.
12. Ghubaish A, Salman T, Zolanvari M, Unal D, Al-Ali A, Jain R. Recent advances in the internet-of-medical-things (IoMT) systems security. IEEE Internet Things J. 2020;8(11):8707-8718.
13. Food and Drug Administration. Proposed regulatory framework for modifications to artificial intelligence/machine learning (AI/ML)-based software as a medical device (SaMD). 2019.
14. Tau N, Shepshelovich D. Assessment of data sources that support US Food and Drug Administration medical devices safety communications. JAMA Intern Med. 2020;180(11):1420-1426.
15. Srivastava G, Crichigno J, Dhar S. A light and secure healthcare blockchain for iot medical devices. In: 2019 IEEE Canadian conference of electrical and computer engineering (CCECE). IEEE; 2019:1-5.
16. Bayoumy K, Gaber M, Elshafeey A, Mhaimeed O, Dineen EH, Marvel FA, Martin SS, Muse ED, Turakhia MP, Tarakji KG, Elshazly MB. Smart wearable devices in cardiovascular care: where we are and how to move forward. Nat Rev Cardiol. 2021;18(8):581-599.
17. Gonzalez-Argote J. Use of virtual reality in rehabilitation. Interdisciplinary Rehabilitation / Rehabilitación Interdisciplinaria. 2022;2:24. https://doi.org/10.56294/ri202224
18. Mavrogiorgou A, Kiourtis A, Perakis K, Pitsios S, Kyriazis D. IoT in healthcare: achieving interoperability of high-quality data acquired by IoT medical devices. Sensors. 2019;19(9):1978.
FUNDING
No financing.
CONFLICTS OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Conceptualization: Basavaraj Mudhol, Meena Krishna, Asha Kademane.
Methodology: Basavaraj Mudhol, Meena Krishna, Asha Kademane.
Drafting - original draft: Basavaraj Mudhol, Meena Krishna, Asha Kademane.
Writing - proofreading and editing: Basavaraj Mudhol, Meena Krishna, Asha Kademane.