ORIGINAL
Exploring the Associations between Diabetes Mellitus and Diabetic Retinopathy: Prevention and Management by focus on Machine Learning Technique
Explorando las Asociaciones entre Diabetes Mellitus y Retinopatía Diabética: Prevención y gestión mediante técnicas de aprendizaje automático
Sirajudeen Ameer John1 ![]() *, Senthilnathan Palaniappan2
*, Senthilnathan Palaniappan2
![]() *,
Ilayaraja Venkatachalam2
*,
Ilayaraja Venkatachalam2 ![]() *, Gopichand Ginnela2
*, Gopichand Ginnela2 ![]() *
*
1VIT Bhopal University, School of Computing Science and Engineering, Bhopal-Indore Highway, Kothrikalan, Sehore, Madhya Pradesh – 466114, India.
2Vellore Institute of Technology, School of Computer Science and Engineering, Vellore.
Cite as: Ameer JS, Palaniappan S, Venkatachalam I, Ginnela G. Exploring the associations between Diabetes Mellitus and Diabetic Retinopathy: Prevention and Management by focus on Machine Learning Technique. Salud, Ciencia y Tecnología 2023;3:556–556. https://doi.org/10.56294/saludcyt2023556.
Submitted: 01-09-2023 Revised: 22-10-2023 Accepted: 05-12-2023 Published: 06-12-2023
Editor: Dr.
William Castillo-González![]()
ABSTRACT
Introduction: diabetes Mellitus, a disorder impacting insulin production and utilization, led to elevated blood sugar levels. Immune system assaults on insulin-producing pancreas cells caused Type 1 Diabetes Mellitus, while Type 2 Diabetes Mellitus affected glucose processing, predominantly in adults but also observed in children. Unmanaged diabetes resulted in varied health issues including heart disease, kidney damage, nerve impairment, and diabetic retinopathy, a major cause of adult blindness.
Objective: to prevent diabetic retinopathy through glycemic control, achieved via management, lifestyle choices, screenings, treatments, education, and awareness. Machine learning techniques like transfer learning, ensemble learning, CNN-MNIST, and multiscale approaches showed promise in detection and diagnosis. Monitoring blood sugar and eye exams were vital for early retinopathy treatment.
Result: DR risk is elevated in those with positive complications like nephropathy, heart disease, cerebrovascular disease, foot ulcers and HbA1C levels ≥6,8 %. Retinal imaging aids diagnosis and monitoring of ocular diseases like DR, utilizing processed monochrome images for structural analysis.
Method: involved observing NPDR, MPDR via eye exams, measuring glucose, visual acuity, and retinal thickness. Retinal imaging aided ocular disease diagnosis, utilizing processed images for analysis.
Conclusion: diabetes prevalence rose globally, projected to affect 800 million adults by 2050. High India rates emphasized healthcare need, especially in remote areas, addressing diabetic retinopathy and early symptom awareness.
Keywords: Diabetes Mellitus; Gestational Complications; Machine Learning; Transfer Learning; Ensemble Learning; CNN-MNIST.
RESUMEN
Introducción: la diabetes mellitus, un trastorno que afecta a la producción y utilización de la insulina, provoca niveles elevados de azúcar en sangre. Las agresiones del sistema inmunitario a las células del páncreas productoras de insulina causaron la diabetes mellitus de tipo 1, mientras que la diabetes mellitus de tipo 2 afectó al procesamiento de la glucosa, predominantemente en adultos, pero también observada en niños. La diabetes no controlada provoca diversos problemas de salud, como cardiopatías, daños renales, alteraciones nerviosas y retinopatía diabética, una de las principales causas de ceguera en adultos.
Objetivo: prevenir la retinopatía diabética mediante el control glucémico, que se consigue a través de la gestión, las elecciones de estilo de vida, las revisiones, los tratamientos, la educación y la concienciación.
Técnicas de aprendizaje automático como el aprendizaje por transferencia, el aprendizaje por conjuntos, CNN-MNIST y enfoques multiescala resultaron prometedoras para la detección y el diagnóstico. El control de la glucemia y los exámenes oculares fueron vitales para el tratamiento precoz de la retinopatía.
Resultados: el riesgo de RD es elevado en aquellos con complicaciones positivas como nefropatía, cardiopatía, enfermedad cerebrovascular, úlceras en los pies y niveles de HbA1C ≥6,8 %. Las imágenes retinianas ayudan al diagnóstico y seguimiento de enfermedades oculares como la RD , utilizando imágenes monocromas procesadas para el análisis estructural.
Método: consistió en observar la RDNP y la RDMP mediante exámenes oculares, midiendo la glucosa, la agudeza visual y el grosor de la retina. Las imágenes retinianas ayudaron al diagnóstico de enfermedades oculares, utilizando imágenes procesadas para el análisis.
Conclusiones: la prevalencia de la diabetes aumentó en todo el mundo y se prevé que afecte a 800 millones de adultos en 2050. Las elevadas tasas de la India pusieron de relieve la necesidad de atención sanitaria, especialmente en zonas remotas, para abordar la retinopatía diabética y el conocimientoprecoz de los síntomas.
Palabras clave: Diabetes Mellitus; Complicaciones Gestacionales; Aprendizaje Automático; Aprendizaje de Transferencia; Aprendizaje Conjunto; CNN-MNIST.
INTRODUCCIÓN
Diabetes mellitus is extended metabolic condition measured by high blood HBA1C stages (hyperglycaemia) ensuing after a deficiency in insulin production, insulin feat else both. The pancreas secretes a hormone known as insulin that help regulate blood HBA1C stages by enabling the approval of HBA1C patterns to be used as vigour or kept for forthcoming use. Rendering to the International Diabetes Federation (IDF), According to the latest statistics, there were approximately 463 million adults aged between 22-78 years living with HBA1C diabetes globally in 2020 and by 2050, the projected figure is 800 million, indicating an increase from current levels. The popular cases, which range from 92 % to 98 %, are ascribed to Type 2 diabetes with HBA1C. India is home-based to the second-highest figure of adults with diabetes in the Universe, as reported by the Diabetes International Federation Atlas 2022, with an appraised 88 million individuals living with the condition. Diabetes Mellitus is prevalent in India, accounting for over 92 % of all diabetes cases. The general occurrence of diabetes in India was 12,0 %, as per a 2020 national study by the Indian Council which belongs to Medical Research (ICMR), with Diabetes Mellitus accounting for 12,6 % of all cases. Nevertheless, the occurrence of diabetes stayed far advanced in urban areas (16,4 %) than in countryside areas (12,0 %).
Based on the latest information supplied by the NDRR in India, it is approximated that between 40 % to 45 % of individuals diagnosed with diabetes experience diabetic retinopathy (DR), a complication that affects the eyes. In the early stages, Diabetes mellitus (DM) may not show any symptoms, leading to many diabetic patients being unaware of their condition. Although healthcare facilities are crucial for people's well-being, their absence can become a major challenge in remote areas that lack road connectivity.
METHODS
Case Study and complication of Diabetic retinopathy
Damage to the blood vessels in the retina, caused by diabetes, can lead to a condition known as diabetic retinopathy, which has the capacity to negatively affect one's vision. To conduct research on diabetic retinopathy, various study designs and population considerations are important. Cross-sectional studies, which determine the prevalence of the disease at a specific point in time, are the most commonly used study design. Observational studies conducted over a prolonged period can aid in determining the typical progression of diabetic retinopathy and evaluating the efficacy of interventions. Individuals with diabetes who are vulnerable to the onset of the ailment must be encompassed in the study of diabetic retinopathy, as they represent the target demographic. Individuals diagnosed with diabetes, whether it be type 1 or type 2, may develop diabetic retinopathy, with those who have been living with the condition for an extended duration being more susceptible to its onset. Additionally, it is imperative to incorporate individuals who possess higher risk factors such as hypertension and hyperlipidemia into the research analysis.
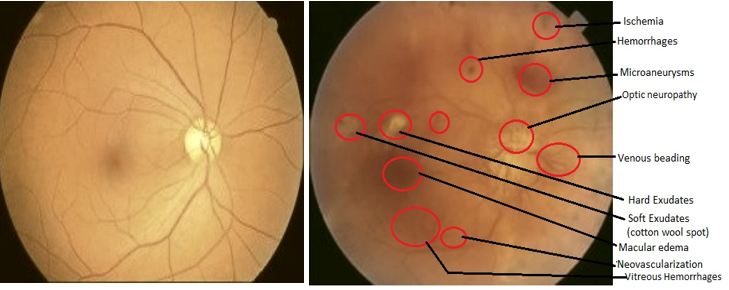
(a) (b)
Figure 1. (a) Fundus photo of healthy retina, (b) Retina with Diabetic Eye Disease
For longitudinal studies in diabetic retinopathy, it is crucial to have a sufficient sample size to attain appropriate statistical power since attrition can lead to the loss of retinal power. In order to be eligible for a study or analysis related to diabetic retinopathy, individuals must meet specific inclusion criteria such as having a diagnosis of diabetes and evidence of diabetic retinopathy determined by clinical examination or imaging. Depending on the severity of the retinopathy, individuals may be categorized as mild, moderate, severe, or proliferative. The age range, duration of diabetes, and level of visual acuity may also be considered depending on the research question. Inclusion criteria must be clearly defined and should also include a diagnosis of diabetes, while exclusion criteria may consist of ocular or systemic diseases that could affect the eye, and any contraindications to treatment. In addition, follow-up periods should be consistent across study participants to avoid bias and long enough to detect changes in diabetic retinopathy that may occur slowly over time. Proper study design and population are crucial in conducting effective research on diabetic retinopathy.
Specific measures and methods in research
To ensure the validity and reliability of research results, it is crucial to establish well-defined variables and operational definitions. When exploring diabetic retinopathy, a range of conditions can be observed during a dilated eye exam, such as minor nonproliferative diabetic retinopathy (NPDR), Intermediate NPDR, Extreme NPDR, and Multiplicative proliferative diabetic retinopathy (MPDR). Blood glucose levels, measured via a glucometer or blood test, may serve as a predictor of disease progression or treatment outcome measure. Other key measures in this field include visual acuity, which assesses a person's ability to see via an eye chart, and retinal thickness, which can be measured using optical coherence tomography (OCT) technology. The gathering of liquid in the central area of the retina, known as macular edema, can be identified with OCT and utilized as a parameter to assess the effectiveness of treatment in diminishing fluid, liquid accumulation and enhancing visual capacity.
Analyses and Complication
Type 2 Diabetes Mellitus, also known as T2DM, is a obstinate metabolic disorder that causes an increase in glucose levels in the bloodstream. Type 2 diabetes mellitus (T2DM) presents with a range of distinct symptoms including increased thirst, frequent urination, fatigue, vision impairment, and delayed wound healing. Treatment approaches for Type 2 Diabetes Mellitus (T2DM) usually consist of a blend of pharmaceutical interventions and lifestyle modifications. These can entail medication to lower blood glucose levels, dietary alterations, exercise routines, and achieving weight loss goals. Figure 2 presents an overview of the proposed system's sequence of operations. By examining the diagram, one can discern the individual stages that make up the recommended approach. Enhancing an image involves altering its brightness, contrast, color, and other attributes to enhance its visual appeal. The technique of histogram equalization can be employed to enhance the contrast of an image by redistributing the intensity of its pixels. The method operates through modifying the image's histogram to distribute the pixel values evenly across the full intensity spectrum. Through redistributing the pixel intensities, histogram equalization serves as an image enhancement technique capable of enhancing image contrast. Histogram equalization involves adjusting the image histogram in such a way that the pixel values are evenly distributed across the whole intensity range. By expanding the intensity range of the image, one can ensure that it fills the complete dynamic range of the display device.
The histogram of an image shows the frequency of occurrence of each pixel intensity value. In a well-contrasted image, the histogram will be spread out over the entire intensity range, whereas in a low-contrasted image, the histogram will be concentrated in a narrow range of intensity values. Histogram equalization works by redistributing the pixel values so that the histogram becomes more uniform across the intensity range. The basic steps involved in histogram equalization is to Compute the histogram of the image and also the cumulative distribution function (CDF) of the histogram. After computing the mapping function that maps the input intensity values to output intensity values based on the CDF, finally apply the mapping function to the input image to obtain the equalized image. Achieving uniformity in a histogram can be carried out through different software programs and programming languages such as MATLAB and Python. The OpenCV library in Python features a function called equalizeHist() which can be leveraged for the purpose of histogram equalization. The histeq() function available in MATLAB serves the identical purpose. Although histogram equalization has the potential to enhance the contrast of images, it may not be the ideal solution for every scenario, particularly for images with a high dynamic range or intricate lighting conditions. In certain types of images, this method may also produce unwanted artifacts or amplify noise. Consequently, it is essential to scrutinize the results of histogram equalization and modify the parameters or explore alternative techniques when necessary.
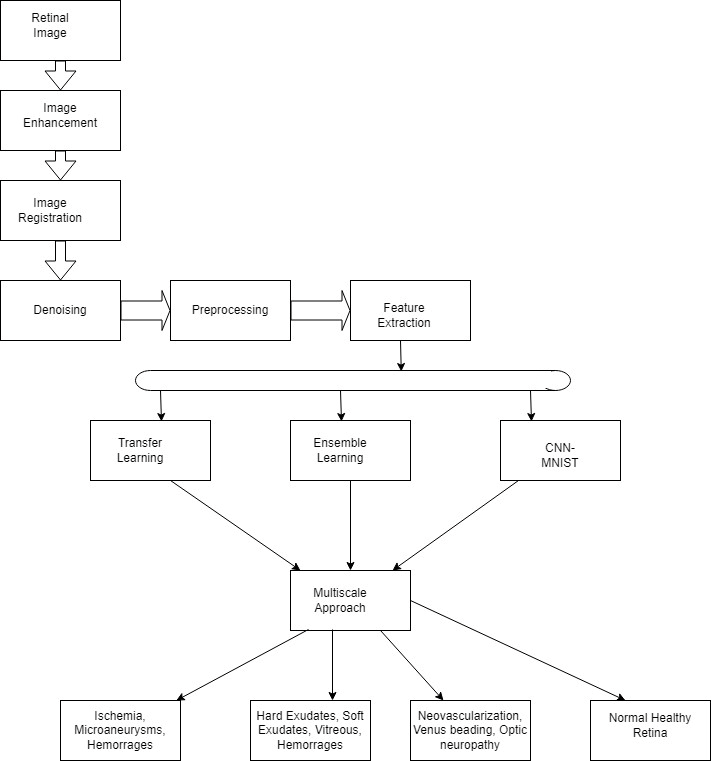
Figure 2. Overall flow of the Proposed System
The process of aligning multiple images of a single scene, captured from different perspectives and at different times, to synchronize their spatial information is referred to as image registration. The ultimate objective of image registration is to determine a geometrical transformation that can map the pixel coordinates of one image to the corresponding coordinates of another image. The process of aligning images, known as image registration, comprises multiple stages that can fluctuate depending on the application's particularities and the nature of the images undergoing registration. The procedure of denoising involves the elimination of extraneous distortions from a digital signal, like an image, while ensuring minimal distortion to the original signal. Undesirable interruptions referred to as noise can arise from multiple sources like a transmission channel or sensor, resulting in the deterioration of the signal's precision and quality. A wide range of denoising techniques are available for images, including basic filtering approaches and sophisticated statistical and machine learning-driven algorithms.
A methodology called data augmentation creates fresh examples for training by utilizing different modifications on the source images, which consist of adjustments such as rotations, scaling, flipping, and cropping. Augmenting data is a technique that can assist in enabling the FCN to acquire the ability to adapt to discrepancies in the input images, resulting in a decline in overfitting. An unsupervised learning approach for feature extraction from input data is presented by Deep Belief Networks (DBNs). These networks contain layers of Restricted Boltzmann Machines (RBMs), which are capable of learning the input data's probability distribution and are utilized as generative models. The initial tiers of the Deep Belief Network are responsible for grasping basic characteristics such as corners and edges, whereas the upper tiers concentrate on acquiring intricate and abstract characteristics.
RESULTS
Out of the limited number of patients with Diabetes Mellitus, around 16,5 % of people were identified with DR was more prevalent among male patients over the age of 70 who also had underlying health conditions such as hypertension, dyslipidemia, nephropathy, ischaemic heart syndrome, cerebrovascular syndrome, and Diabetic HBA1C Foot Base Ulcer. Additionally, the prevalence of DR was found to be higher in patients who had been living with diabetes for 25 years or more. The analysis of two variables revealed that patients aged 70 years or older had a nearly four-fold higher likelihood of developing DR when compared to other age groups. The associated confidence interval was 1,63-12,74. Moreover, male patients were 1,1 intervals, further likely to grow DR than females, through a confidence interval of 1,05-1,20. Additionally, diabetic patients with comorbidities, including hypertension, hyperlipidemia, cardiovascular disease, diabetic retinopathy, neuropathy, and nephropathy, were 2,1 periods more likely to develop DR when related to those without hypertension. The corresponding confidence interval was 1,1-2,2. Finally, dyslipidemia, an abnormality in lipid or fat levels in the blood, was found to be a significant risk factor for the growth of cardiovascular related disease, including syndrome of heart attack and stroke, in diabetic patients.
Regarding diabetic mellitus complications, individuals with positive conditions have a higher likelihood of developing DR or diabetic retinopathy, including nephropathy [OR 4,6 (96 % CI 3,7-4,8)], ischemic heart related disease [OR 1,8 (95 % CI 1,31-2,21)], cerebrovascular type of disease such as stroke, TIA, and cerebral aneurysms [OR 1,5 (95 % CI 1,05-2,19)], and diabetic foot ulcers [OR 4,7 (95 % CI 3,3-6,9)]. Furthermore, the duration of the disease is also positively associated with DR, as individuals with diabetic mellitus for 30 years or more are four whiles more possible to develop DR than persons with a shorter duration of the disease. The study's results also revealed that patients with an HbA1C level of 6,8 % or higher have a 1,4 times greater chance of developing diabetic retinopathy (95 % CI 1,26-1,49). The identification and isolation of particular regions of interest in a retinal image, known as "area of focus extraction," is a crucial stage in the examination of retinal images for a range of applications, such as disease diagnosis and detection, monitoring treatment effectiveness, and disease progression tracking. Retinal imaging is a valuable technique in ophthalmology that enables clinicians to observe and analyze the retina by taking a photograph or digital image of the light-sensitive tissue that lines the back of the eye, which is called the retina. A grayscale image pertains to an image where each pixel's intensity is conveyed through a solitary value, which usually spans from 0 (black) to 255 (white), displaying gray shades in between. Specialized cameras are employed to take retinal images that provide high-quality pictures of the retina. This part of the eye is comprised of light-sensitive cells that facilitate our vision. Ophthalmologists and other medical practitioners frequently rely on these visuals to identify and keep track of different ocular ailments, including but not limited to diabetic retinopathy, macular degeneration, and glaucoma. A modified or improved image that emphasizes specific features or structures within the retina is commonly known as a "processed image" in the field of retinal image processing. When working with retinal images, a "monochrome image" denotes an image that has undergone a grayscale conversion, wherein every pixel is denoted by a solitary value ranging from 0 (denoting black) to 255 (indicating white). Retinal image analysis frequently employs this particular image type due to its ability to streamline image data while maintaining crucial aspects such as contrast, texture, and edges. The assessment and treatment of a range of eye conditions such as glaucoma, age-related macular degeneration, and diabetic retinopathy often involve the use of retinal images. Analyzing such images entails the identification and quantification of distinct structures including blood vessels, the macula, and the optic disc.
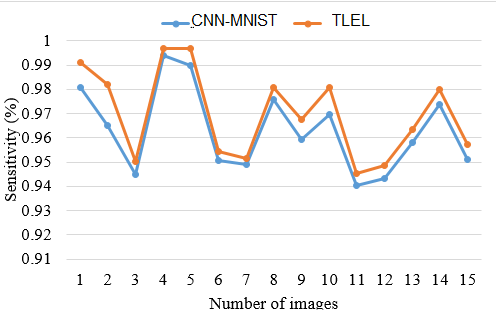
Figure 3. Impact of variations in TLEL and CNN-MNIST through sensitivity analysis
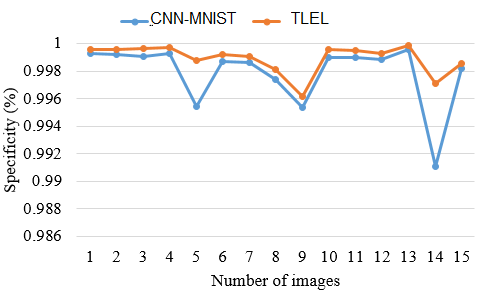
Figure 4. Impact of variations in TLEL and CNN-MNIST through Specificity Analysis
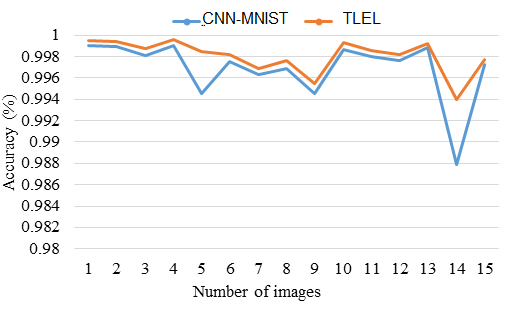
Figure 5. Impact of variations in TLEL and CNN-MNIST through Accuracy Analysis
DISCUSSION
Based on data from the NDRR registry, the prevalence of Diabetic Retinopathy was observed to be 16,5 % in p_-atients diagnosed with Diabetes Mellitus during the training phase. However, the frequency of Diabetic Retinopathy slightly differed across certain regions in India. Interestingly, the research uncovered a comparatively greater incidence of Diabetic Retinopathy, which might be linked to modifications in the method of collecting study samples. This research study, in contrast to the NDRR study, incorporated individuals under the age of 38, leading to a greater number of participants and an increased prevalence of Diabetic Retinopathy. According to the outcomes, it can be inferred that advanced age serves as a notable determinant for the emergence of Diabetic Retinopathy in patients diagnosed with Diabetes Mellitus. This discovery aligns with prior research studies that highlighted a 2,3 odds ratio linked to the age-induced susceptibility of Diabetic Retinopathy.(1,2)
As per the findings of the NDRR Registry's Wiscon Epidemiology Study on Diabetic Retinopathy (WESDR) III, there is a strong correlation between the severity of diabetic retinopathy (DR) and an early age of onset at the time of diagnosis. The NDRR study exhibited a higher likelihood of DR development among grown-ups due to vascular deviations in the retinal flow, corroborating the aforementioned finding. In elderly persons, if DR is not treated, it may result in blindness. After conducting an extensive NDRR investigation, we have discovered a significant correlation between the duration of diabetes mellitus and DR, suggesting that an increased span of diabetes mellitus is positively linked to the development of DR. Similar published studies have also reported this association, although our study showed a lower odds ratio, which may be due to differences in sociodemography and physical features of the training population. In our NDRR learning, 23,0 % of the sample had DR, with 23,0 % diagnosed with diabetes mellitus for less than four years, 26,0 % diagnosed between four to eight years, and 16,0 % diagnosed and treated for atleast more than ten years. The advanced occurrence of DR (23,0 %) in earlier studies compared to the clinical trial (16,5 %) may be owed to wider inclusion and presence criteria for the study population.
The incidence of recent Diabetic Retinopathy is closely related to effective diabetes management, with good control of HbA1C levels playing a crucial role. Conversely, inadequate diabetes control can result in unacceptable HbA1C levels that increase the likelihood of emerging Diabetic Retinopathy. Studies have found a important association among HbA1C levels and the enhancement of Diabetic Retinopathy,(5,6) with a decrease of 1,6 % in HbA1C being related with a 39,0 % drop in microvascular type of problems. Conversely, the implication of HbA1C levels as a finding for Diabetic Retinopathy is inconclusive,(4) and the main factor in its development appears to be periodic exposure to high levels in blood glucose. Diabetic Glycemic has to control through lifestyle changes such as physical activity, stress reduction, strong diet habits, and a healthy lifestyle is protective against Diabetic Retinopathy.(7) While pharmacological and lifestyle interventions are more common, pancreas replacement and islet cell kind of transplantation are also obtained for Diabetic Retinopathy.(8) Islet cell movement has exposed hopeful results in reducing the advance of DR, but Glucemic patients who has received transplants may have better baseline Glycemic HbA1C control than who did not,(9) and further research is needed to establish the efficacy of islet cell transplantation in Diabetic Retinopathy.(8) In terms of medical management, nonstop insulin pump treatment has been related with a greater reduction in Glycemic DR levels and superior benefits over conservative insulin treatment.(13)
Individuals diagnosed with Diabetic Retinopathy (DR) encounter numerous risks and complexities linked to the ailment. DR, a chronic diabetic complication, exerts its influence on the retinal blood vessels, the light-sensitive tissue situated at posterior part of the eye. [14]. Presented below are some perils frequently encountered by individuals grappling with DR. DR stands as the primary catalyst behind vision loss and the ensuing blindness that afflicts adults in their productive years.(15,16) The compromised blood vessels within the retina may discharge fluid or hemorrhage, thereby instigating swelling and distorted vision.(17) Should appropriate treatment be neglected, this condition may steadily advance towards irreversible vision loss.Effective management of diabetes requires close collaboration between medical professionals and patients. Maintaining intensive blood sugar control with minimal glucose level fluctuations has long-term benefits, including preventing the growth of Diabetic Retina and other complications in the Diabetes Mellitus, such as Diabetic Nephropathy, which affects the small blood vessels in the kidney and Peripheral Vascular Disease (PVD), which affects blood vessels external the heart and brain, and Coronary Heart Disease (CHD), which occurs when blood supply to a vessel is restricted or blocked.(10) According to a study, there is a robust correlation between Diabetic Retinopathy and Diabetic Nephropathy, with a 20,3 % occurrence rate of Diabetic Retinopathy among the patients with Diabetic Nephropathy.(11) The patho physiology of together both conditions is connected to the outcome of unrestrained blood glucose glycemic levels in the DR cell membrane and the production of oxidating pressure. Researchers have identified several mechanistic pathways that offer potential targets for therapeutic interventions and that help clarify diabetic problems, counting with the glycation in the proteins and development of advanced glycation end-products (AGEs). A suitable study occurrence in the pathogene of Diabetic Retinopathy and Diabetic Nephropathy found that AGEs played a role in the "metabolic memory" phenomenon underlying diabetes complications, and that this was related to HbA1C levels.(12) Advanced Diabetic Retinopathy is associated with cellular membrane changes in the eye, which may also occur in small nerves in the kidney.(2,3)
The utilization of pre-trained models to tackle novel tasks is a popular technique in machine learning known as transfer learning.(18) This approach has been implemented in the detection of diabetic retinopathy through the refinement of pre-existing models. The method of ensemble learning utilizes the combination of several models to enhance the system's overall performance, and has been implemented in detecting diabetic retinopathy by utilizing numerous CNN models. One method known as CNN-MNIST entails the training of CNN models utilizing the MNIST dataset, while another technique called multiscale approaches entails the use of several scales to examine images, which can aid in the identification of diabetic retinopathy. The detection of diabetic retinopathy has been improved by utilizing various CNN models trained on different image scales, employing machine learning techniques such as transfer learning, ensemble learning, CNN-MNIST, and multiscale approaches.(19) These methods have exhibited optimistic outcomes in the diagnosis and detection of the disease. The utilization of such methodologies holds promise in enhancing the precision and speed of diabetic retinopathy screening, ultimately mitigating the risk of impaired vision and complete loss of sight among individuals affected by diabetes.
CONCLUSIONS
Individuals with Diabetic Retinopathy face various risks and complications, including vision loss and blindness. Timely and intensive blood sugar control is essential for preventing the progression of DR and related complications. There is a robust correlation between Diabetic Retinopathy and other diabetes-related complications such as Diabetic Nephropathy and Peripheral Vascular Disease. Uncontrolled blood glucose levels play a central role in the development of these conditions. Transfer learning and ensemble learning techniques, utilizing pre-trained CNN models and various scales, have shown promise in enhancing the accuracy and speed of diabetic retinopathy screening and detection. This study findings contribute to the understanding of Diabetic Retinopathy and its correlation with diabetes management and other complications. Utilizing advanced techniques in detection holds potential for improving patient outcomes and reducing the risk of vision impairment and blindness among diabetic individuals.
REFERENCES
1. Lima VC, Cavalieri GC, Lima MC, Nazario NO, Lima GC. Risk factors for diabetic retinopathy: A case-control study. Int J Retin Vitr. 2016; 2(1):1–7. https://doi.org/10.1186/s40942-016-0047-6
2. Lim MCC, Shu YL, Cheng BCL, Wong DWK, Sze GO, Chong LA, et al. Diabetic retinopathy in diabetics referred to a tertiary centre from a nationwide screening programme. Ann Acad Med Singapore. 2008; 37(9):753–9. PMID: 18989491.
3. Klein R, Knudtson MD, Lee KE, Gangnon R, Klein BEK. The Wisconsin Epidemiologic Study of Diabetic Retinopathy XXII. Ophthalmology. 2008; 115(11):1859–68. https://doi.org/10.1016/j.ophtha.2008.08.023
4. Abougalambou SSI, Abougalambou AS. Risk factors associated with diabetic retinopathy among type 2 diabetes patients at teaching hospital in Malaysia. Diabetes Metab Syndr Clin Res Rev. 2015; 9(2):98–103. https://doi.org/10.1016/j.dsx.2014.04.019
5. Canova-Barrios C, Machuca-Contreras F. Interoperability standards in Health Information Systems: systematic review. Seminars in Medical Writing and Education 2022;1:7–7. https://doi.org/10.56294/mw20227
6. Yau JWY, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012; 35(3):556–64. https://doi.org/10.2337/dc11-1909
7. Inastrilla CRA. Data Visualization in the Information Society. Seminars in Medical Writing and Education 2023;2:25–25. https://doi.org/10.56294/mw202325
8. Raman R, Ganesan S, Pal SS, Kulothungan V, Sharma T. Prevalence and risk factors for diabetic retinopathy in rural India. Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetic Study III (SN-DREAMS III), report no 2. BMJ Open Diabetes Res Care. 2014; 2(1):e000005. https://doi.org/10.1136/bmjdrc-2013-000005
9. Kumar N, Reddy N, Kishan R. Diabetic eye screening in multi-ethnic population of Malaysia: epidemiological risk factors for development of diabetic retinopathy. Int J Res Med Sci. 2014; 2(3):1045.
10. Fiorina P, Shapiro AMJ, Ricordi C, Secchi A. The clinical impact of islet transplantation. Am J Transplant. 2008; 8(10):1990–7. https://doi.org/10.1111/j.1600-6143.2008.02353.x
11. Robertson RP. Islet Transplantation a Decade Later and Strategies for Filling a Half-Full Glass. Diabetes. 2010; 59:1285–91. https://doi.org/10.2337/db09-1846
12. Zabeen B, Craig ME, Virk SA, Pryke A, Chan AKF, Cho YH, et al. Insulin pump therapy is associated with lower rates of retinopathy and peripheral nerve abnormality. PLoS One. 2016; 11(4):1–10. https://doi.org/10.1371/journal.pone.0153033
13. Lee WJ, Sobrin L, Lee MJ, Kang MH, Seong M, Cho H. The relationship between diabetic retinopathy and diabetic nephropathy in a population-based study in Korea (KNHANES V-2, 3). Investig Ophthalmol Vis Sci. 2014; 55(10):6547–53.
14. Miao F, Chen Z, Genuth S, Paterson A, Zhang L, Wu X, et al. Evaluating the role of epigenetic histone modifications in the metabolic memory of type 1 diabetes. Diabetes. 2014; 63(5):1748–62. https://doi.org/10.2337/db13-1251
15. Sirajudeen A, Anuradha Balasubramaniam, S. Karthikeyan. "Novel angular binary pattern (NABP) and kernel-based convolutional neural networks classifier for cataract detection." Multimedia Tools and Applications - Springer. DOI:10.1007/s11042-022-13092-8. 2022.
16. Sirajudeen A & Dr. Ezhilarasi M. "Multi-scale LBP and SVM Classification to Identify Diabetic Retinopathy in Lesions." Current Medical Imaging Reviews, Benthem Science. 11.1 (2015): 49-55.
17. Auza-Santiváñez JC, Díaz JAC, Cruz OAV, Robles-Nina SM, Escalante CS, Huanca BA. Interactive formats: considerations for scientific publications. Seminars in Medical Writing and Education 2023;2:27–27. https://doi.org/10.56294/mw202327
18. Palaniappan S., Palli S., Gopichand G., Ameerjohn S., Gopal, S.S. "Enhanced handwritten number detection using kernel discriminant analysis (KDA)." Journal of Computational and Theoretical Nanoscience, 2018, 15(8), pp. 2539–2543. DOI:10.1166/jctn.2018.7494.
19. Dr. A. Sirajudeen. "A Review On Automatic Detection Of Diabetic Retinopathy Using Digital Fundus Images." Indian Journal of Scientific Research, Vol. 17(2), pp. 456-462, 2018.
20. Dr. Senthilnathan Palaniappan, Dr. Sirajudeen Ameer John, and Dr. Ilayaraja Venkatachalam. "Face Recognition Using Scale Invariant Feature Transform." Journal of Advanced Research in Dynamical and Control Systems, Institute of Advanced Scientific Research, no. 06, 2017, pp. 1-32.
21. Inastrilla CRA. Big Data in Health Information Systems. Seminars in Medical Writing and Education 2022;1:6–6. https://doi.org/10.56294/mw20226
22. Sirajudeen A & Dr. Ezhilarasi M. "Independent Component Analysis and Uncorrelated Discriminant Analysis for Diabetic Retinopathy Lesion Detection." Australian Journal of Basic & Applied Sciences, vol. 9, no. 5, pp. 238-244, 2015 - ISSN: 1991-8178.
23. Sirajudeen A & Dr. Ezhilarasi M. "A Pioneering Smartphone Application for the Detection of Diabetic Retinopathy." International Journal of Applied Engineering Research, vol. 9, no. 22, pp. 12577-12590, 2014 - ISSN 0973-4562.
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Dr. A. Sirajudeen, Dr. Senthilnathan Palaniappan, Dr. Gopichand G.
Data curation: Dr. A. Sirajudeen, Dr. Senthilnathan Palaniappan
Formal analysis: Dr. A. Sirajudeen, Dr. Ilayaraja Venkatachalam
Acquisition of funds: the authors did not receive financing for the development of this research.
Research: Dr. A. Sirajudeen, Dr. Senthilnathan Palaniappan
Methodology: Dr. A. Sirajudeen, Dr. Senthilnathan Palaniappan
Project management: Dr. A. Sirajudeen, Dr. Senthilnathan Palaniappan, Dr. Ilayaraja Venkatachalam
Resources: Dr. A. Sirajudeen, Dr. Senthilnathan Palaniappan,
Software: Authors used MatlabR2022a for this Research work.
Supervision: Dr. A. Sirajudeen
Validation: Dr. A. Sirajudeen, Dr. Senthilnathan Palaniappan
Display: Dr. A. Sirajudeen, Dr. Senthilnathan Palaniappan, Dr. Ilayaraja Venkatachalam
Drafting - original draft: Dr. A. Sirajudeen, Dr. Senthilnathan Palaniappan, Dr. Ilayaraja Venkatachalam
Writing - proofreading and editing: Dr. A. Sirajudeen, Dr. Senthilnathan Palaniappan, Dr. Ilayaraja Venkatachalam