ORIGINAL Article
Serological markers associated with poor prognosis in positive Covid-19 patients
Marcadores serológicos asociados a mal pronóstico en pacientes Covid-19 positivos
Paola
Micaela Lasluisa-Toalombo1 ![]() , Daniela Alexandra Rosero Freire1
, Daniela Alexandra Rosero Freire1 ![]() *, Angela Carolina Jácome-Lara2
*, Angela Carolina Jácome-Lara2 ![]() , Luis Fabian Salazar-Garcés1,3
, Luis Fabian Salazar-Garcés1,3 ![]()
1Faculty of Health Sciences, Technical University of Ambato, Ambato, Ecuador.
2General Hospital IESS-Ambato, Ambato, Ecuador.
3Allergy and Acarology Laboratory, Federal University of Bahia, Bahia, Brazil.
Cite as: Lasluisa-Toalombo PM, Jacome-Lara AC, Rosero Freire DA, Salazar-Garcés LF. Serological markers associated with poor prognosis in positive Covid-19 patients. Salud Cienc. Tecnol. 2022;2:141. https://doi.org/10.56294/saludcyt2022141
Received: 29-11-2022 Reviewed: 06-11-2022 Accepted: 11-12-2022 Published: 12-12-2022
Editor:
Lic. Mabel Cecilia Bonardi ![]()
ABSTRACT
Background: Covid-19 is a disease caused by a new coronavirus known as SARS-CoV-2. Spike viral protein binds to ACE2 body receptors and determines its infectivity. This process has many effects on the host, causing damage to the respiratory system and at the systemic level in general, evidenced in the elevation of laboratory markers such as Interleukin-6, Ferritin and D-Dimer.
Objective: to analyze biomarkers (Interleukin-6, Ferritin and D-Dimer) as factors of poor prognosis in Covid-19.
Methods: the data was collected from Covid-19 patients who also had results of IL-6, D-D and Ferritin obtained through the IESS Ambato hospital databases.
Findings: we reported 114 Covid-19 patients, whom we analyzed serological markers. D-D and IL-6 show a 1,34 OR (C.I.: 1,14 - 1,58) and 1,26 OR (C.I.: 1,11 - 1,43) respectively. Ferritin had a positive association in female population 1,11 OR (C.I.: 0,99 – 1,24), but in the male population, we didn’t find a significant association 3,91 OR (C.I.: 0,46 - 32,99). It was found that comorbidities were a protective factor with a negative association of 0,88 OR. Secondary causes of death in Covid-19 patients were cardiac arrest and pneumonia (23,1 %).
Conclusion: IL-6, Ferritin and D-D markers were evaluated and proved valuable tools to predict poor prognosis in patients with Covid-19. These markers proceeded independently of other factors like comorbidities. The findings of this study may help manage other pathologies with a similar curse and to focus more on the importance at the laboratory level as a prognostic support.
Keywords: Covid-19; Interleukin-6; Ferritin; D-Dimer; Biomarkers.
RESUMEN
Antecedentes: Covid-19 es una enfermedad causada por un nuevo coronavirus conocido como SARS-CoV-2. La proteína viral Spike se une a los receptores corporales ACE2 y determina su infectividad. Este proceso tiene muchos efectos en el huésped, causando daños en el sistema respiratorio y a nivel sistémico en general, evidenciados en la elevación de marcadores de laboratorio como la Interleucina-6, Ferritina y D-Dímero.
Objetivo: analizar los biomarcadores (Interleuquina-6, Ferritina y D-Dímero) como factores de mal pronóstico en Covid-19.
Métodos: se recolectaron los datos de los pacientes con Covid-19 que además tenían resultados de IL-6, D-D y Ferritina obtenidos a través de las bases de datos del hospital IESS Ambato.
Resultados: reportamos 114 pacientes con Covid-19, a quienes analizamos los marcadores serológicos. D-D e IL-6 muestran una OR de 1,34 (C.I.: 1,14 - 1,58) y 1,26 (C.I.: 1,11 - 1,43) respectivamente. La ferritina tuvo una asociación positiva en la población femenina 1,11 OR (C.I.: 0,99 - 1,24), pero en la población masculina, no encontramos una asociación significativa 3,91 OR (C.I.: 0,46 - 32,99). Se encontró que las comorbilidades eran un factor protector con una asociación negativa de OR = 0,88. Las causas secundarias de muerte en los pacientes Covid-19 fueron la parada cardiaca y la neumonía (23,1 %).
Conclusiones: los marcadores IL-6, Ferritina y D-D fueron evaluados y demostraron ser herramientas valiosas para predecir el mal pronóstico en pacientes con Covid-19. Estos marcadores procedieron independientemente de otros factores como las comorbilidades. Los hallazgos de este estudio pueden ayudar al manejo y pronóstico.
Palabras clave: Covid-19; Interleucina-6; Ferritina; D-Dímero; Biomarcadores.
INTRODUCTION
Covid-19 is a disease caused by a new coronavirus known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It was identified in late 2019 as the causative agent of several cases of unknown pneumonia in Wuhan, China.(1) Generating an epidemiological alert in the Asian country that escalated to the point of being declared a pandemic by the WHO in March 2020.
The effectiveness of SARS-CoV-2 infectious process has been determined thanks to its spike protein (S)(2) which contains two subunits S1 y S2; S1 contains the receptor binding domain of the angiotensin-converting enzyme 2 (ACE2)(2) while S2 allows the fusion of the viral membrane with the cell membrane, becoming a highly conserved zone.(3,4) Nutshell, the S protein allows the virus to bind to ACE2 and adhere mainly to cells of the respiratory tract and conjunctiva.(3)
Different studies have shown that SARS-CoV-2 infection, in addition to causing damage to the respiratory system, also causes systemic effects.(1,2) New evidence suggests a direct relationship between SARS-CoV-2 infection and increased heart attacks in patients who have developed the most severe form of Covid-19.(5)
Studies have revealed several immune response mechanisms that are activated in the response to SARS-CoV-2 infection, one of them is the elevation of levels of Interleukin-6 (IL-6) in Covid-19 patients.(6,7)
IL-6 is typically released in viral infections and tissue damage.7 It is expressed by cells of the innate immune system such as macrophages and by non-immune cells such as vascular endothelial cells, mesenchymal cells, and fibroblasts.(8)
This following the detection of damage-associated molecular patterns (DAMPs) or pathogen-associated molecular patterns (PAMPs) which are host strategies to remove infected cells and eliminate tissue damage.(7)
On the other hand, the excessive production of IL-6 leads to the development of chronic inflammatory diseases and hyperinflammation processes known as cytokine storms, in which the patient presents a hyper-reactive immune response.(7)
According to Coomes & Haghbayan,(6) several studies have shown elevated IL-6 levels in patients with Covid-19, and there is evidence that these patients have developed severe disease. According to a survey conducted at Jin Yin-tan and Tongji hospitals in Wuhan, China,(9) elevated IL-6 values were identified in patients who died of Covid-19 compared to those who survived.
Furthermore, the role of ferritin in developing SARS-CoV-2 infection severity has also been studied.(10,11) Ferritin is a spherical coat-like molecule called "apoferritin".(10)
Esper et al.(12) mediated that ferritin expression is mediated by inflammatory processes such as oxidative stress, hormonal response, growth factors, hypoxia, ischemia and hyperoxia. Within the SARS-CoV-2 infection process, hypoxia is a stimulus that forces the organism to produce a large amount of ferritin to compensate the lack of oxygen in patients with Covid-19.
At the same time, hypoxia causes vasoconstriction that reduces blood flow and increases endothelial size, causing oxygen to take longer to reach the various organs.(2) Studies such as the one by Cheng et al. (2020) have shown that it can be considered a good marker of cell damage. In addition, it is a critical factor in the process of immune deregulation since it comes from damaged cells, which contributes to the cytokine storm, which has been associated with high mortality in patients admitted to the ICU.(11)
D-dimer (D-D) is a specific biomarker in the formation and degradation of fibrin clots.(13) In healthy individuals, serum levels are low, while it tends to be elevated in conditions associated with thrombotic processes.
Therefore, it is studied in the diagnosis and monitoring of venous thromboembolism (VTE), disseminated intravascular coagulation (DIC), and the identification of patients at high risk of developing VTE as is the case of patients with Covid-19.(13,14)
Due to pathological events, such as hypoxia secondary to excessive lung damage in these patients.(15) With this evidence, it is of utmost importance to address D-D as a predictor of Acute Myocardial Infarction (AMI) and mortality because, according to Weitz et al.(13) some studies suggest an association between elevated D-D levels and the risk of developing cardiovascular events. Also, several investigations express a high connection between increases in D-D and mortality in Covid-19 patients as mentioned by Rostami & Mansouritorghabeh.(14,16)
This study aims to analyze the serological markers (Interleukin-6, Ferritin and D-Dimer), which have become notorious in the study of the severity and poor prognosis of individuals who develop the most severe cases of Covid-19. Besides, we pretend to establish whether there is a relationship between these biomarkers and the mortality of patients hospitalized due to this pathology.
In addition, this study is relevant since the usefulness of biomarkers is being evaluated in relation to their predictive value of mortality in patients diagnosed with Covid-19 and together with the severity of the clinical conditions of the patients and their relationship with the origin of acute respiratory distress syndrome and multi-organ failure due to cytokine storm and thrombotic events.
METHODS
The present study analyzed data from patients whose diagnosis was Covid-19 and who were admitted to the General Hospital of the Ecuadorian Social Security Institute (IESS) Ambato during the period July 2021 - March 2022.
Data patient recruitment: the data analyzed in this study was from patients diagnosed with Covid-19 by either Reverse transcription-polymerase chain reaction in real time (RT-PCR) test or by rapid antigen test (CIE-10 UO071). Besides, those cases ranging in age between 18 and 95 years, who also had results of Interleukin-6, D-Dimer and Ferritin. By searching the hospital databases, a population of 114 patients with the aforementioned criteria was obtained.
Sample collection and processing: we filtered the necessary information using the databases without accessing any clinical history. The samples were collected and processed by the hospital clinical laboratory staff allowing us to have the results for this study.
RT-PCR: nasopharyngeal samples were collected by the staff of the clinical laboratory service of the General Hospital IESS-Ambato and sent to the General Hospital IESS-Quito Sur (referential hospital), following the refrigeration and sample shipping protocols. In the referential hospital the techniques for RNA extraction and RT-PCR essays were applied according to specifications stablished by PWO and WHO.(17,18)
Rapid antigen Test: were performed in private clinical laboratories, using the standardized method of lateral flow immunochromatography, following the procedure stablish globally.(17)
IL-6, DD, and Ferritin determination: IL-6: Determination was based on the Electrochemiluminescence (ECLIA) method using the Elecsys IL-6 kit (N°54022601, Roche, Germany). Cobas e411 equipment was used to analyze the samples following the manufacturer's specifications.
Ferritin: the samples were analyzed in Cobas e411 analyzer through the ECLIA Elecsys Ferritin kit (N° 53055101 and N°54864001, Roche, Germany), the specification used for making these determinations are available in the insert.
D-Dimer: the samples were analyzed in Cobas c311 analyzer under the particle-enhanced immunoturbidimetry test Elecsys D-Dimer (N° 52868701 and 55531401, Roche, Germany) following the manufacturer's protocol.
Ethics: this study was approved by the teaching and research department and the medical direction of General Hospital IESS- Ambato who allow us the access to the services of statistics, internal medicine, and clinical laboratory service. The ethics committee of the Technical University of Ambato reviewed and approved this research for publication. Patients were managed by numerical codes, protecting their identity. In this way, the confidentiality of the extracted results was also ensured.
Statical Analysis: Kolmogorav Smirnov and Shapiro Wilk tests were used to assess the normality of the data. Where appropriate, the Wilcoxon signed-rank test or paired t-tests were used to compare paired groups of continuous measurements. Values of P < 0,05 were considered statistically significant results. The statistical analysis software GraphPad Prism 7.0 and SPSS 25 were used.
RESULTS
The population was of 114 patients, of which 38 were women (33,3 %), and 76 were men (66,7 %) (Table 1) with a median age of 62,68 years (range 22-95 years).
Besides, the eatery group with higher frequency was 47 to 70 years (47,4 %) shown in Figure 1.
The frequency of dead people was 11,4 % that means 13 people (Figure 2), of which 3 were women (23,1 %) and 10 were men (76,9 %) (Table 2). The mean age of this population was 73,69 years with a minimum age of 63,5 and a maximum of 80 years.
In our population 51 patients showed higher values of D-D compared with reference values (0-0,5 ugUEF/mL). Of these 51 patients, 13 of them died (25,5 %). Of the 63 patients with typical values, none died; about association analyses we could observe a positive association with a 1,34 OR (C.I.:1,14 - 1,58), this means more risk of death when this biomarker is elevated (Table II).
IL-6 results are positively associated with the risk of death (1,26 OR C.I.:1,11 - 1,43). Our results show that in 63 patients with elevated serum levels of IL-6, 13 died (20,6 %). For this, the reference value was 0-14 pg/mL
|
Table 1. Characteristics of patients with Covid-19 diagnosis |
||
|
Characteristics |
Frequency |
Percent (%) |
|
Sex |
|
|
|
Female |
38 |
33,3 |
|
Male |
76 |
66,7 |
|
Total |
114 |
100,0 |
|
Age |
|
|
|
22 - 45 years |
22 |
19,3 |
|
46 - 70 years |
54 |
47,4 |
|
71 - 95 years |
38 |
33,3 |
|
Total |
114 |
100 |
|
Comorbidities |
|
|
|
Arterial Hypertension |
|
|
|
No |
107 |
93,9 |
|
Yes |
7 |
6,1 |
|
Total |
114 |
100 |
|
Diabetes Mellitus |
|
|
|
No |
109 |
95,6 |
|
Yes |
5 |
4,4 |
|
Total |
114 |
100 |
|
EPOC |
|
|
|
No |
112 |
98,2 |
|
Yes |
2 |
1,8 |
|
Total |
114 |
100 |
|
Kidney Chronic Disease |
|
|
|
No |
110 |
96,5 |
|
Yes |
4 |
3,5 |
|
Total |
114 |
100 |
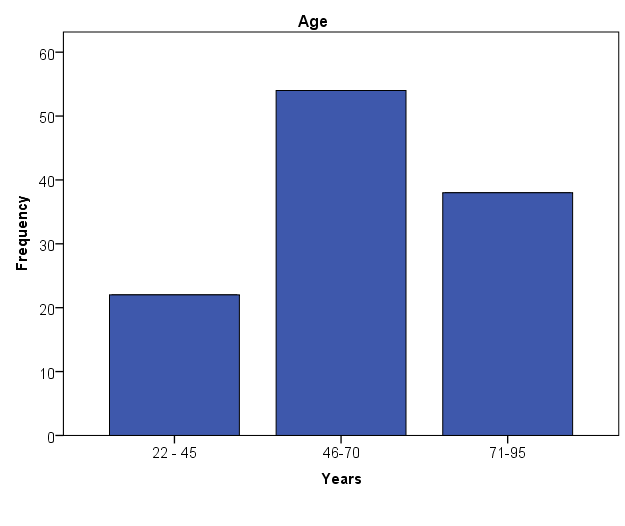
Figure 1. Age distribution of Covid-19 patients
(Table 2). On the other hand, the remaining 50 patients had IL-6 values within the reference values, and no declines were observed in this group.
The determination of Ferritin in the female population had a reference value of 13-150 ng/mL, where 31 patients reported a higher value; three died (9,7 %). Seven patients within range value no one died. It results in 1,11 OR (C.I.: 0,99 – 1,24) which means borderline effect with a positive association with the risk of death. For the male population, we had a 3,91 OR (C.I.: 0,46 - 32,99) and didn’t find association between higher results and death. In this case, the reference value was 30-400 ng/mL, and 55 had a higher value to whom 9 died (16,4 %), and of the 21 patients with markers within the reference, one died (5 %) (Table 2).
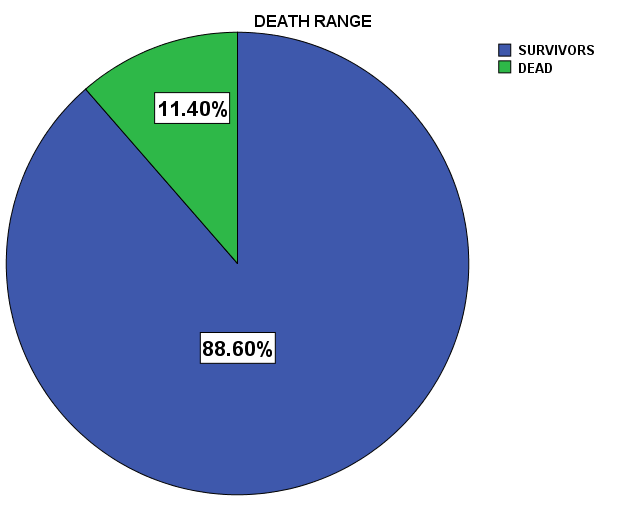
Figure 2. Death range of Covid-19 confirmed patients
|
Table 2. Relationship between the characteristics and death on Covid-19 patients |
|||
|
Characteristics |
Total |
Number (%) |
OR (CI) |
|
Sex |
|
|
|
|
Female |
38 |
3 (23,1) |
1 |
|
Male |
76 |
10 (76,9) |
1,77 (0,46-6,84) |
|
Laboratory biomarkers |
|
|
|
|
D-Dimer (ugUEF/mL) |
|
|
|
|
0,00 - 0,50 |
63 |
0 (0,0) |
1 |
|
> 0,50 |
51 |
13(100) |
1,34 (1,14 - 1,58) |
|
IL-6 (pg/mL) |
|
|
|
|
0,00 - 14,00 |
51 |
0 (0,0) |
1 |
|
> 14,00 |
63 |
13 (100) |
1,26 (1,11 - 1,43) |
|
Ferritin (ng/mL) |
|
|
|
|
Female |
|
|
|
|
13,00 - 150,00 |
7 |
0 (0,0) |
1 |
|
>150,00 |
31 |
3 (100) |
1,11(0,99 - 1,24) |
|
Male |
|
|
|
|
30 - 400 |
21 |
1 (10) |
1 |
|
>400,00 |
55 |
9 (90) |
3,91 (0,46 - 32,99) |
|
Comorbidities |
|
|
|
|
Arterial hypertension |
|
|
|
|
No |
107 |
13 (12,1) |
1 |
|
Yes |
7 |
0 (0,0) |
0,88 (0,82 - 0,94) |
|
Diabetes Mellitus |
|
|
|
|
No |
109 |
13 (11,9) |
1 |
|
Yes |
5 |
0 (0,0) |
0,88 (0,82 - 0,95) |
|
EPOC |
|
|
|
|
No |
112 |
13 (11,6) |
1 |
|
Yes |
2 |
0 (0,0) |
0,88 (0,83 - 0,95) |
|
Kidney chronic disease |
|
|
|
|
No |
110 |
11 (10) |
1 |
|
Yes |
4 |
2 (50) |
4,13 (0,35 - 48,97) |
|
Bold values mean a significant relevance in statistical analyses OR (CI) |
|||
To know the death reason and the relation between the elevated biomarkers, we made the investigation having the following results: 3 cases (23,1 %) of pneumonia, 3 cases of heart attack (23,1 %), 1 case of septic shock (7,7 %) and respiratory insufficiency in 1 patient (7,7 %). In the other hand, we had a 38,4 % of the dead population without a second cause of death just because of the SARS-CoV-2 infection (Table 3).
|
Table 3. Secondary death causes of Covid-19 patients |
||
|
Secondary egress cause |
Frequency |
Percent(%) |
|
Pneumonia |
3 |
23,1 |
|
Cardiac arrest |
3 |
23,1 |
|
Septic shock |
1 |
7,7 |
|
Respiratory insufficiency |
1 |
7,7 |
|
No secondary cause |
5 |
38,4 |
|
Total |
13 |
100 |
DISCUSSION
The current study shows the risk factors for patients diagnosed with Covid-19 to develop a severe prognosis. We focused mainly on specific laboratory biomarkers. Still, at the same time, relevant data regarding age, sex, and comorbidities were found during the research development.
Several studies report that age alone is the most significant risk factor for developing the severe form of COVID-19.(16,19) In this investigation, most hospitalized patients were between 46 y 70 years old. Hypothetically, this could be due to carelessness and lack of precaution of this populational group, because it’s a range age economically active and necessity couldn’t comply with the lockdown, causing the disease to become more complicated, requiring hospitalization.
Evidence has been found in the study conducted by O’Driscoll, et al.(20) which support our hypothesis; here, it’s suggested that those patients older than 65 years are considered at higher risk and tend to be isolated and protected on time. Consequently, they have less need for hospitalization and lower mortality.
Additionally, reference to the death age showed an average of 73,96 years, a minimum age of 63,5 years, and a maximum of 80 years. These findings are supported by studies such as the one by Wu, et al.,(16) made in Italy, where takes evidence that the mortality rate increased with age.
This investigation focused on the effectiveness of biomarkers: Interleukin-6, Ferritin and D-dimer as a prognostic aid in the mortality of Covid-19 patients. Our study showed that having high levels of D-D is associated with death. Here, it was reported 13 people dead, of which all had values above the reference range. These results are closely related to other studies like Barzola, et al.(21) y Rostami, et al.,(14) since they show that higher levels of D-D increase the probability of death due to thrombotic processes caused by damage to the microvascular system, which have been reported as clots, observed more frequently in Covid -19 patients than in normal patients.(21)
For Interleukin-6, we identified that it as an effective biomarker for poor prognosis in patients with Covid-19. Because of the 13 deceased, all of them had a value above 14 pg/mL. Studies supporting this, such as Coomes et at. & Kang et al.,(6,7) showed that patients who developed the severe disease had elevated IL-6 values up to 3 times higher than its reference value. This elevation in values is due to the cytokine storm to which the organism infected by SARS-CoV-2 is exposed. In many cases, it becomes lethal because it causes a series of fatal processes such as respiratory failure, shock and multiorgan failure (6) favoring the exacerbated elevation of this cytokine, especially in uncontrolled viral infections.(8)
Ferritin has been analyzed in several studies as a poor prognostic factor in patients with Covid-19,(11) as it is a mediator of immune dysregulation with notable immunosuppressive and proinflammatory effects contributing to a cytokine storm.
Besides, it could be a significant biomarker of viral replication for its release against viral infections.(11) This study shows a borderline association within a positive association between female patients with elevated serum ferritin levels and mortality (OR de 1,11 C.I.: 0,99 – 1,24).
At the same time, the male population does not show an OR association (OR 3,91 C.I.: 0,46 - 32,99), which is based on the reference range used in both categories. On the one hand, the reference values for the female population are between 13 to 150 ng/mL and the reference range for the male population is 30 to 400 ng/mL. Thus, a male patient presenting a value higher than 150 ng/mL was categorized as a patient with typical values. This could generate a bias in the analysis, which is why statistically, Ferritin in men does not show a positive association as in the case of women. However, in other studies (10,11) where the reference value is unified for men and women, a positive association was observed, which means that at elevated ferritin levels the risk of death is higher regardless of the sex of the patient.
On the other hand, correlation studies of comorbidities and death risk in Covid-19 patients have shown a very supported data about this association, as shown in a survey carried out in Wuhan-China,(19) where it was found that the risk factors for developing severe Covid-19 disease were age, male sex, obesity, and comorbidities such as hypertension, type 2 diabetes mellitus, among others.(18,19)
Nevertheless, in our research, this turns out to be a conflicting point with various data from the literature since we obtained results that arterial hypertension, type 2 diabetes mellitus, and chronic obstructive pulmonary disease (COPD) could act as protective factors and not risk factors. With the clarification that for this negative association to being fulfilled, the comorbidities must be controlled under medical supervision and adequate administration of medications.
Patients suffering from Arterial Hypertension, Diabetes Mellitus and COPD at the same time as being diagnosed as Covid-19 positive were considered as survivors in our study, since; statistically, they had a negative association with an OR of 0,88 (C.I.: 0,82-0,94 for arterial hypertension, C.I.: 0,82-0,95 diabetes mellitus y C.I.: 0,83-0,95 COPD); in other words, those patients suffering from any of these comorbidities survived.
Hospitalized patients suffering from arterial hypertension and diabetes-mellitus maintained control of their disease due to medications such as Losartan (ARBs), Enalapril (ACEI), and chlorthalidone. Some studies manifest that ARBs (Angiotensin II receptor blockers) and ACEI (Angiotensin converting enzyme inhibitors) increase ACE2 expression,(18,22) as does chlorthalidone (type of diuretic), which is considered harmful in the context of Covid-19.(23)
On the other hand, according to a study by Esler y Esler (23) suggests that the use of both, ACEI and ARBs reduces the ACE2 expression by facilitating the transformation of angiotensin I to angiotensin II and by the reduction of renin releasing, respectively. Thus, these could be use preferably for Covid-19 patients.(23)
On the contrary, a meta-analysis performed by Pirola & Sookoian,(24) shows evidence that suggests the use of ARBs and ACEI as protective drugs in Covid-19 patients, thereby supporting our findings that comorbidities acted as a protective factor because having comorbidities under controlled, the complication and death risk decreased.
Clinical records revealed that the most frequent causes of death were pneumonia and cardiac arrest, followed by septic shock and respiratory failure due to viral infection. All these secondary causes of death are explained by the same reason;(5,9,11) the organism undergoes a series of inflammatory processes that deteriorate the health of the individual causing insufficient oxygen to reach the different organs, either by blockage of the arteries by the formation of clots or by an exacerbated response of the immune system causing serious damage especially in heart and lung tissues, as evidenced in our study by the elevation of the biomarkers IL-6, Ferritin and D-D.
Thus, the death of our population was not directly related to comorbidities but rather to the course of the Covid-19 infection itself, which deteriorated the organism, as demonstrated in the study by Elezkurtaj, et al.(25)
CONCLUSION
In this study we were able to demonstrate that the IL-6, Ferritin and D-D proposed as poor prognostic biomarkers in Covid-19 have potential to be considered as predictors of death in patients, regardless of age, sex, and comorbidities, which is why it is of utmost importance to approach them as a predictor of mortality in infection cases, as in this case was for SARS-Cov-2.
REFERENCES
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med 2020;382:727-33. https://doi.org/10.1056/NEJMoa2001017.
2. Valverde AJS, Temoche CEM, Caicedo CRC, Hernández NBA, Padilla TMT. Covid-19: fisiopatología, historia natural y diagnóstico. Revista Eugenio Espejo 2021;15:98-114. https://doi.org/10.37135/ee.04.11.13.
3. Cevik M, Kuppalli K, Kindrachuk J, Peiris M. Virology, transmission, and pathogenesis of SARS-CoV-2. BMJ 2020;371:m3862. https://doi.org/10.1136/bmj.m3862.
4. Jin Y, Yang H, Ji W, Wu W, Chen S, Zhang W, et al. Virology, Epidemiology, Pathogenesis, and Control of COVID-19. Viruses 2020;12:372. https://doi.org/10.3390/v12040372.
5. Mafham M, Baigent C. What is the association of COVID-19 with heart attacks and strokes? Lancet 2021;398:561-3. https://doi.org/10.1016/S0140-6736(21)01071-0.
6. Coomes EA, Haghbayan H. Interleukin-6 in Covid-19: A systematic review and meta-analysis. Reviews in Medical Virology 2020;30:e2141. https://doi.org/10.1002/rmv.2141.
7. Kang S, Kishimoto T. Interplay between interleukin-6 signaling and the vascular endothelium in cytokine storms. Exp Mol Med 2021;53:1116-23. https://doi.org/10.1038/s12276-021-00649-0.
8. Akira S, Taga T, Kishimoto T. Interleukin-6 in Biology and Medicine. En: Dixon FJ, editor. Advances in Immunology, vol. 54, Academic Press; 1993, p. 1-78. https://doi.org/10.1016/S0065-2776(08)60532-5.
9. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 2020;46:846-8. https://doi.org/10.1007/s00134-020-05991-x.
10. Mahroum N, Alghory A, Kiyak Z, Alwani A, Seida R, Alrais M, et al. Ferritin – from iron, through inflammation and autoimmunity, to COVID-19. Journal of Autoimmunity 2022;126:102778. https://doi.org/10.1016/j.jaut.2021.102778.
11. Cheng L, Li H, Li L, Liu C, Yan S, Chen H, et al. Ferritin in the coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. J Clin Lab Anal 2020;34:e23618. https://doi.org/10.1002/jcla.23618.
12. Carrillo Esper R, Peña Pérez C, Zepeda Mendoza AD, Meza Márquez JM, Neri Maldonado R, Meza Ayala CM, et al. Ferritina y síndrome hiperferritinémico: Su impacto en el enfermo grave; conceptos actuales. Revista de la Asociación Mexicana de Medicina Crítica y Terapia Intensiva 2015;29:157-66.
13. Weitz JI, Fredenburgh JC, Eikelboom JW. A Test in Context: D-Dimer. Journal of the American College of Cardiology 2017;70:2411-20. https://doi.org/10.1016/j.jacc.2017.09.024.
14. Rostami M, Mansouritorghabeh H. D-dimer level in COVID-19 infection: a systematic review. Expert Review of Hematology 2020;13:1265-75. https://doi.org/10.1080/17474086.2020.1831383.
15. Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thrombosis Research 2020;191:145-7. https://doi.org/10.1016/j.thromres.2020.04.013.
16. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Internal Medicine 2020;180:934-43. https://doi.org/10.1001/jamainternmed.2020.0994.
17. World Health Organization. Technical guidance publications. WHO 2022. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance-publications (accedido 8 de diciembre de 2022).
18. Shu L, Wang X, Li M, Chen X, Ji N, Shi L, et al. Clinical characteristics of moderate COVID-19 patients aggravation in Wuhan Stadium Cabin Hospital: A 571 cases of retrospective cohort study. Journal of Medical Virology 2021;93:1133-40. https://doi.org/10.1002/jmv.26414.
19. Chen Y, Klein SL, Garibaldi BT, Li H, Wu C, Osevala NM, et al. Aging in COVID-19: Vulnerability, immunity and intervention. Ageing Res Rev 2021;65:101205. https://doi.org/10.1016/j.arr.2020.101205.
20. O’Driscoll M, Ribeiro Dos Santos G, Wang L, Cummings DAT, Azman AS, Paireau J, et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature 2021;590:140-5. https://doi.org/10.1038/s41586-020-2918-0.
21. Barzola CMP, Amay CLP, Delgado KAC, Fierro LMM. Trastornos de la coagulación en pacientes infectados con coronavirus: Covid-19. RECIAMUC 2020;4:50-7. https://doi.org/10.26820/reciamuc/4.(3).julio.2020.50-57.
22. Sommerstein R, Kochen MM, Messerli FH, Gräni C. Coronavirus Disease 2019 (COVID‐19): Do Angiotensin‐Converting Enzyme Inhibitors/Angiotensin Receptor Blockers Have a Biphasic Effect? Journal of the American Heart Association 2020;9:e016509. https://doi.org/10.1161/JAHA.120.016509.
23. Esler M, Esler D. Can angiotensin receptor-blocking drugs perhaps be harmful in the COVID-19 pandemic? Journal of Hypertension 2020;38:781-2. https://doi.org/10.1097/HJH.0000000000002450.
24. Pirola CJ, Sookoian S. Estimation of Renin-Angiotensin-Aldosterone-System (RAAS)-Inhibitor effect on COVID-19 outcome: A Meta-analysis. Journal of Infection 2020;81:276-81. https://doi.org/10.1016/j.jinf.2020.05.052.
25. Elezkurtaj S, Greuel S, Ihlow J, Michaelis EG, Bischoff P, Kunze CA, et al. Causes of death and comorbidities in hospitalized patients with COVID-19. Sci Rep 2021;11:4263. https://doi.org/10.1038/s41598-021-82862-5.
FUNDING
The author did not receive funding for the development of this research.
CONFLICT OF INTEREST
The author declares no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Paola Micaela Lasluisa-Toalombo, Daniela Alexandra Rosero Freire.
Data curation: Paola Micaela Lasluisa-Toalombo.
Formal analysis: Paola Micaela Lasluisa-Toalombo, Luis Fabian Salazar-Garcés.
Investigation: Paola Micaela Lasluisa-Toalombo.
Methodology: Paola Micaela Lasluisa-Toalombo, Daniela Alexandra Rosero Freire, Luis Fabian Salazar-Garcés.
Project administration: Angela Carolina Jácome-Lara, Daniela Alexandra Rosero Freire, Luis Fabian Salazar-Garcés.
Resources: Paola Micaela Lasluisa-Toalombo, Angela Carolina Jácome-Lara.
Validation: Paola Micaela Lasluisa-Toalombo, Angela Carolina Jácome-Lara, Daniela Alexandra Rosero Freire, Luis Fabian Salazar-Garcés.
Writing – original draft: Paola Micaela Lasluisa-Toalombo, Angela Carolina Jácome-Lara, Daniela Alexandra Rosero Freire, Luis Fabian Salazar-Garcés.
Writing - revision and editing: Paola Micaela Lasluisa-Toalombo, Angela Carolina Jácome-Lara, Daniela Alexandra Rosero Freire, Luis Fabian Salazar-Garcés.